Practice Essentials
Acute otitis media (AOM) is defined by convention as the first 3 weeks of a process in which the middle ear shows signs and symptoms of acute inflammation. One consideration in the emergent management of AOM is that diagnostic certainty for the disease is based on all three of the following criteria, as set forth by the American Academy of Pediatrics (AAP) and the American Academy of Family Physicians (AAFP): acute onset, middle ear effusion (MEE), and middle ear inflammation. Studies have shown that, despite adequate access to clinical guidelines, the prescribing rates for antibiotics in acute otitis media (AOM) in some emergency departments remain high. [1, 2]
Severe illness is defined as moderate to severe otalgia or temperature greater than 39°C, whereas nonsevere illness is defined as mild otalgia and temperature less than 39°C. AOM most commonly occurs in children and is the most frequent specific diagnosis in children who are febrile. Clinicians often overdiagnose AOM. Recurrent AOM is defined as 3 episodes within 6 months or 4 or more episodes within 1 year.
Distinguishing between AOM and otitis media with effusion (OME) is important. OME is more common than AOM. When OME is mistaken for AOM, antibiotics may be prescribed unnecessarily. OME is fluid in the middle ear without signs or symptoms of infection. It is usually caused when the eustachian tube is blocked and fluid becomes trapped in the middle ear. Signs and symptoms of AOM occur when fluid in the middle ear becomes infected. (See the images below.)
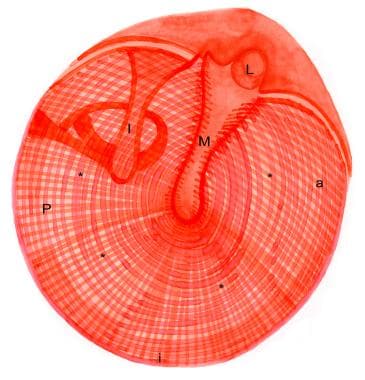 Drawing of a normal right tympanic membrane. Note the outward curvature of the pars tens (*) of the eardrum. The tympanic annulus is indicated anteriorly (a), inferiorly (i), and posteriorly (P). M = long process of the malleus; I = incus; L = lateral (short) process of the malleus.
Drawing of a normal right tympanic membrane. Note the outward curvature of the pars tens (*) of the eardrum. The tympanic annulus is indicated anteriorly (a), inferiorly (i), and posteriorly (P). M = long process of the malleus; I = incus; L = lateral (short) process of the malleus.
 Tympanic membrane of a person with 12 hours of ear pain, slight tympanic membrane bulge, and slight meniscus of purulent effusion at bottom of tympanic membrane. Reproduced with permission from Isaacson G: The natural history of a treated episode of AOM. Pediatrics. 1996; 98(5): 968-7.
Tympanic membrane of a person with 12 hours of ear pain, slight tympanic membrane bulge, and slight meniscus of purulent effusion at bottom of tympanic membrane. Reproduced with permission from Isaacson G: The natural history of a treated episode of AOM. Pediatrics. 1996; 98(5): 968-7.
 Days after onset of symptoms, vessels continue across pars tensa, and a fluid layer of pus is noted. Reproduced with permission from Isaacson G: The natural history of a treated episode of AOM. Pediatrics. 1996; 98(5): 968-7.
Days after onset of symptoms, vessels continue across pars tensa, and a fluid layer of pus is noted. Reproduced with permission from Isaacson G: The natural history of a treated episode of AOM. Pediatrics. 1996; 98(5): 968-7.
Using the Nationwide Emergency Department Sample database, Ren et al determined that between 2009 and 2011 the weighted total of emergency department visits for patients presenting with a primary diagnosis of AOM or acute mastoiditis reached more than 5.8 million, with the average patient age being 10.1 years. The investigators found that 0.26% of patients presented with a complication, with acute mastoiditis (0.16%), labyrinthitis (0.06%), and facial paresis (0.03%) being the most common and with complicated AOM tending to occur in adults (age 37 years) rather than children. [3]
In light of extreme weather events associated with climate change, a Viennese study by Nieratschker et al sought to determine whether such events impacted AOM-related emergency department (ED) visits. The investigators found that, while single-day extreme events did not significantly affect these visits, events such as extremely low temperatures, high relative humidity, and high atmospheric pressure, that stretched over 3 days did. However, the effect was in most cases seen after a multi-day lag time, so that, for example, 3 days of 89% humidity increased the cumulative relative risk (cRR) of AOM-related ED visits to 1.43 on the seventh day. On the other hand, RR was reduced to 0.94 on the seventh day in association with a 3-day period of 37% humidity. Prolonged heavy precipitation with total accumulations of 24 mm resulted in a decrease in the cRR from 0.70 to 0.52 between days 4 and 14. [4]
In a multisite, cross-sectional study, McLaren et al found that afebrile infants with AOM who were seen in emergency departments had a low prevalence of invasive bacterial infections and adverse events. Patients in the study were aged 90 days or younger, with blood and cerebrospinal fluid (CSF) cultures revealing no bacteremia or bacterial meningitis, respectively. An adverse event, specifically lymphadenitis or culture-negative sepsis, was seen in just two of the 645 infants (0.3%) who had 30-day follow-up. The investigators suggested that it may be reasonable for afebrile infants with clinician-diagnosed AOM to undergo outpatient management without diagnostic testing. [5]
Workup in acute otitis media
Diagnostic certainty in AOM is based on all three of the following criteria:
-
Acute onset
-
MEE
-
Middle ear inflammation
Severe illness is defined as moderate-to-severe otalgia or temperature greater than 39°C, whereas nonsevere illness is defined as mild otalgia and temperature less than 39°C.
Diagnosis can include use of the following:
-
Insufflation, tympanometry, and acoustic reflexometry - Helpful to identify the presence or absence of MEE; of these, insufflation is the only one commonly used in the emergency department (ED) setting
-
Tympanocentesis and/or myringotomy - May be appropriate to delineate the etiology of AOM in an immunocompromised patient, a patient with mastoiditis, [6] a patient with persistent fever in the face of antibiotic therapy, or a patient with intractable pain
Management of acute otitis media in the emergency department
The May 2004 AAP/AAFP clinical practice guidelines for the management of AOM in children aged 6 months to 12 years recommend that infants younger than age 6 months receive antibiotics and that children aged 6 months to 2 years receive antibiotics if the diagnosis is certain.
Children aged 2 years and older should receive antibiotics if the diagnosis is certain and if the illness is severe. If the diagnosis is uncertain, an observation period can be considered if the illness is nonsevere.
Diagnostic Considerations
Insufflation, tympanometry, and acoustic reflexometry are helpful to identify the presence or absence of MEE. Of these, insufflation is the only one commonly used in the emergency department (ED) setting. Tympanometry and acoustic reflexometry cannot be recommended as a routine screening test for acute otitis media (AOM). However, in a patient in whom examination is difficult, normal tympanometric results may help to rule out AOM.
Nasopharyngoscopy may reveal anatomic factors involved in AOM and show purulent matter at the nasal opening of the eustachian tube, but the findings are of no acute diagnostic value.
No definitive laboratory examination exists for AOM, and hearing tests are not helpful in diagnosing the condition. Radiography and/or computed tomography (CT) scanning of the mastoid air cells may be helpful in select cases of suspected mastoiditis, but imaging studies are not valuable for diagnosis of AOM. [7]
Tympanocentesis, myringotomy, or both may be appropriate to delineate the etiology of AOM in an immunocompromised patient, a patient with mastoiditis, [6] a patient with persistent fever in the face of antibiotic therapy, or a patient with intractable pain. If AOM is present in infants younger than 2-3 months, some authors recommend tympanocentesis. These procedures often are performed by the ear, nose, and throat (ENT) consultant. In the event that a tympanocentesis is performed, a sample of the effusion should be sent for culture and sensitivity. [8]
Guidelines
A 2013 update to guidelines from the AAP and the AAFP recommends the following criteria for the diagnosis of AOM in children [9] :
-
Clinicians should diagnose AOM in children who present with moderate to severe bulging of the tympanic membrane (TM) or new onset of otorrhea not due to acute otitis externa; evidence quality: grade B
-
Clinicians may diagnose AOM in children who present with mild bulging of the TM and recent (less than 48 hours) onset of ear pain (holding, tugging, rubbing of the ear in a nonverbal child) or intense erythema of the TM; evidence quality: grade C
-
Clinicians should not diagnose AOM in children who do not have middle ear effusion (MEE) (based on pneumatic otoscopy and/or tympanometry); evidence quality: grade B
Emergency Department Diagnosis
As previously mentioned, diagnostic certainty in acute otitis media (AOM) is based on all 3 of the following criteria: acute onset, MEE, and middle ear inflammation. Severe illness is defined as moderate-to-severe otalgia or temperature greater than 39°C, whereas nonsevere illness is defined as mild otalgia and temperature less than 39°C.
Although the definition of AOM is relatively uniform, the diagnosis is not always as clear. It is this diagnostic uncertainty that may lead to overdiagnosis and unnecessary antibiotic use or to underdiagnosis and an increase in complications. Overdiagnosis of AOM is frequently a result of all of the following:
-
Difficulty in differentiating AOM from OME
-
Difficulty in confirming Mee
-
Poor compliance with guidelines for diagnosis
Several studies have demonstrated the difficulty and inconsistency with which practitioners diagnose AOM. [10, 11] In a study of interrater agreement on AOM in children, Blomgren et al noted a substantial discrepancy concerning practitioner impressions of the tympanic membrane. The clinicians agreed on only 64% of the diagnoses of AOM. The use of a pneumatic otoscopy and tympanometry reduces the number of AOM diagnoses by greater than 30%, suggesting that AOM is misdiagnosed often. [12, 13]
Emergency Department Treatment
The May 2004 AAP/AAFP clinical practice guidelines for the management of AOM in children aged 6 months to 12 years recommend that infants younger than age 6 months receive antibiotics and that children aged 6 months to 2 years receive antibiotics if the diagnosis is certain. (See Table 1.)
Children aged 2 years and older should receive antibiotics if the diagnosis is certain and if the illness is severe. If the diagnosis is uncertain, an observation period can be considered if the illness is nonsevere, and antibiotic therapy can be considered for severe illness.
According to AAP/AAFP guidelines, an observation period may be recommended depending on the patient's age, the diagnostic certainty, and the severity of illness. [14] An observation period is an option when the diagnosis is uncertain or when it is certain and nonsevere. The observation option is a 48-hour to 72-hour period of symptomatic treatment with analgesics and without antibiotics.
For an observation option to be considered, the parent or caregiver must be able to communicate with the clinician and have access to follow-up care whenever problems ensue or symptoms worsen. Studies in the ED setting have shown that the observation option is feasible and well accepted. [15, 16]
If prescribed antibiotics, children younger than age 2 years and those aged 2-5 years with severe disease should receive 10 days of therapy. For those who are age 6 years or older with mild to moderate disease, 5-7 days is appropriate.
Pain management is an important part of treating AOM. Appropriate analgesics should be offered.
The aforementioned 2013 update to the AAP/AAFP guidelines includes the following recommendations regarding the care of pediatric patients with AOM [9] :
-
The management of AOM should include an assessment of pain; if pain is present, the clinician should recommend treatment to reduce pain; evidence quality: grade B
-
Severe AOM: The clinician should prescribe antibiotic therapy for AOM (bilateral or unilateral) in children aged 6 months or older with severe signs or symptoms (ie, moderate or severe otalgia, otalgia for at least 48 hours, or temperature of 102.2°F or higher); evidence quality: grade B
-
Nonsevere bilateral AOM in young children: The clinician should prescribe antibiotic therapy for bilateral AOM in children aged 6 months through 23 months without severe signs or symptoms (ie, mild otalgia for less than 48 hours and temperature of less than 102.2°F); evidence quality: grade B
-
Nonsevere unilateral AOM in young children: The clinician should either prescribe antibiotic therapy or offer observation with close follow-up based on joint decision-making with the parent(s)/caregiver for children aged 6-23 months of age with unilateral AOM without severe signs or symptoms (ie, mild otalgia for less than 48 hours and temperature less than 102.2°F); evidence quality: grade B
-
Nonsevere AOM in older children: The clinician should either prescribe antibiotic therapy or offer observation with close follow-up based on joint decision-making with the parent(s)/caregiver for children aged 24 months or older with AOM (bilateral or unilateral) without severe signs or symptoms (ie, mild otalgia for less than 48 hours and temperature less than 102.2°F); evidence quality: grade B
Table: Criteria for Initial Antibacterial Treatment
Studies have also shown that, despite adequate access to clinical guidelines, the prescribing rates for antibiotics in acute otitis media (AOM) in some emergency departments remain high. [1, 2] (In accordance with the guidelines, however, administration of amoxicillin and analgesics has increased.) [17] Nonetheless, in a retrospective study of children with refractory acute otitis media (AOM) treated in a pediatric emergency department (mean age 19 mo), Pitaro et al found that out middle ear cultures for 55 ears, two were positive for Streptococcus pneumoniae and one for Moraxella catarrhalis, with most of the cultures being sterile. [18]
Table 1. Criteria for Initial Antibacterial Agent Treatment or Observation in Children With Acute Otitis Media [19] (Open Table in a new window)
Age |
Certain Diagnosis |
Uncertain Diagnosis |
< 6 mo |
Antibacterial therapy |
Antibacterial therapy |
6 mo–2 y |
Antibacterial therapy |
Antibacterial therapy if severe illness; observation option* if nonsevere illness |
≥2 y |
Antibacterial therapy if severe illness; observation option* if nonsevere illness |
Observation option* |
*Observation is an appropriate option only when follow-up can be ensured and antibacterial agents started if symptoms persist or worsen. Nonsevere illness is mild otalgia and fever of less than 39°C in the previous 24 hours. Severe illness is moderate to severe otalgia or fever greater than or equal to 39°C. A certain diagnosis of AOM meets all 3 criteria: (1) rapid onset, (2) signs of MEE, and (3) signs and symptoms of middle-ear inflammation. [19] |
||
Considerations in Pharmacologic Therapy
Antibiotics
Studies have shown that antibiotics provide little benefit beyond placebo in mild cases of acute otitis media (AOM).
Infants with frequent recurrences of AOM may be considered for daily antibiotic prophylaxis with sulfamethoxazole or amoxicillin for a period of several months. However, the decrease in frequency of recurrent episodes is small to none. [20, 21]
The potential consequences of excessive antibiotic use are well known, and newer recommendations are that antibiotic prophylaxis for AOM should be avoided whenever possible.
If antibiotic therapy is chosen, the AAP and FAAP recommend that amoxicillin 80-90 mg/kg/d be the antibiotic of choice. The length of treatment is 10 days for younger children and patients with severe illness, otherwise, a 5- to 7-day course is appropriate.
If additional beta-lactamase-positive Haemophilus influenzae and/or Moraxella catarrhalis coverage is desired, the administration of high-dose amoxicillin and clavulanate potassium is recommended.
If the patient is allergic to amoxicillin, alternatives are cefdinir, cefpodoxime, or cefuroxime if the allergic reaction is not a type 1 hypersensitivity. Patients with type 1 hypersensitivity should be given azithromycin or clarithromycin.
Ceftriaxone injection (50 mg/kg/d) is recommended for children who are unable to take oral antibiotics and for patients with compliance problems. However, a single injection of ceftriaxone is insufficient against nonsusceptible pneumococci, with a bacteriologic failure rate of approximately 40%. [22] In patients whose condition fails to improve after initial antibiotic therapy, a 3-day course of ceftriaxone offers outcomes better than those of a 1-day course.
When prescribing antibiotics to the pediatric population, one also has to consider the probability of noncompliance to therapy. In this age group, the palatability of a drug may influence adherence to treatment. If prescribing cephalosporins, consider the use of cefdinir (Omnicef), as it has a more accepted taste when compared with the other recommended cephalosporins (eg, cefuroxime). [23]
Topical quinolones are the preferred agents for the treatment of AOM in children with tympanostomy tubes (AOMT) and/or perforations. The treatment options for AOMT, as discussed in a clinical review by Schmelzle et al, include systemic or topical antibiotics. [24] Topical treatment with fluoroquinolones is superior to that with systemic antibiotics and results in less antibiotic resistance and fewer adverse effects (ototoxicity) than do other treatments.
Because of potential ototoxicity, topical aminoglycosides should be avoided and not used to treat the draining ear. [24]
Other medications
The management of AOM should always include assessment of pain and fever. Antipyretics and analgesics may be necessary and should be prescribed liberally.
The addition of dexamethasone to a topical antibiotic may decrease the length of time necessary for middle ear drainage when compared with a topical antibiotic alone. The evidence for superior outcomes with the addition of steroids lacks strength; plus, the addition of steroids exacerbates overall treatment costs, and this may lead to nonadherence to treatment. [24]
Steroids, decongestants, and antihistamines are not effective in the treatment of AOM and may instead cause complications.
Several complementary and/or alternative medicine (CAM) therapies, such as homeopathy, acupuncture, herbal remedies, chiropractic treatments, and nutritional supplements, have been used by parents/caregivers for the treatment of AOM. The preferred therapy is largely dependent on cultural background and/or practices. Data supporting complementary and alternative therapies are limited and controversial. Currently, there are no recommendations for the use of CAM for the treatment of AOM. [19]
Follow-Up Care
Most cases of otitis media are self-limited. If the signs and symptoms of acute otitis media (AOM) are resolved, patients should follow up with their primary care provider (PCP) in 4-6 weeks to evaluate for persistent OME. In addition, patients discharged with or without antibiotic therapy should be reexamined 4-6 weeks after their initial presentation for evidence of middle ear aeration.
Patients whose symptoms (eg, pain, fever) do not resolve within 48-72 hours of treatment should be reevaluated. Patients with persistent symptoms or recurrent AOM should be referred to an otorhinolaryngologist for evaluation and possible tympanocentesis. If antibiotics were started initially and if the patient's condition fails to improve, the antibiotic should be changed, and compliance must be emphasized.
If an observation period is chosen, failure to improve within 48-72 hours should prompt initiation of antibiotic therapy.
A study by Hendrickson et al of follow-up preferences among PCPs and emergency medicine providers (EMCs) in a regional health system found that for patients with upper respiratory tract infection or AOM, PCPs were more likely than EMCs to direct patients to pursue as-needed follow-up rather than definite follow-up. [25]
-
Drawing of a normal right tympanic membrane. Note the outward curvature of the pars tens (*) of the eardrum. The tympanic annulus is indicated anteriorly (a), inferiorly (i), and posteriorly (P). M = long process of the malleus; I = incus; L = lateral (short) process of the malleus.
-
Tympanic membrane of a person with 12 hours of ear pain, slight tympanic membrane bulge, and slight meniscus of purulent effusion at bottom of tympanic membrane. Reproduced with permission from Isaacson G: The natural history of a treated episode of AOM. Pediatrics. 1996; 98(5): 968-7.
-
Days after onset of symptoms, vessels continue across pars tensa, and a fluid layer of pus is noted. Reproduced with permission from Isaacson G: The natural history of a treated episode of AOM. Pediatrics. 1996; 98(5): 968-7.
-
Tympanic membrane.










