Practice Essentials
In 1903, Robert Osgood (1873-1956), a US orthopedic surgeon, and Carl Schlatter (1864-1934), a Swiss surgeon, concurrently described the disease that now bears their names. Osgood-Schlatter disease (OSD) is a common cause of knee pain in active adolescents.
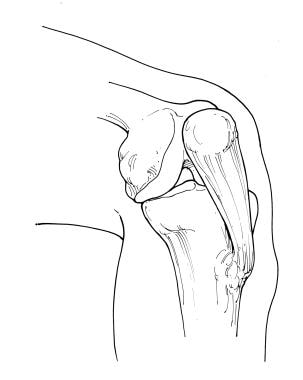
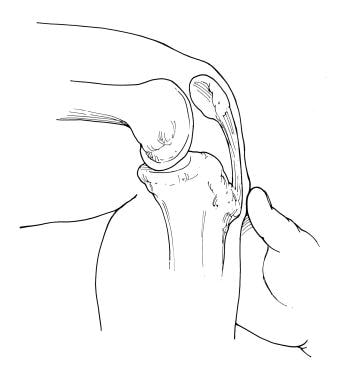
OSD is a traction phenomenon resulting from repetitive quadriceps contraction through the patellar tendon at its insertion upon the skeletally immature tibial tubercle. This occurs in preadolescence during a time when the tibial tubercle is susceptible to strain. The pain associated will be localized to the tibial tubercle and occasionally the patellar tendon itself. A similar process can occur at the patella-patellar tendon junction, which is referred to as Sinding-Larsen-Johansson syndrome (the adolescent equivalent of jumper's knee). [1] (See the images below.)
 Radiograph of a patient who is skeletally mature. Note that the tibial tubercle is enlarged and there is an ossicle. A bursa was overlying this.
Radiograph of a patient who is skeletally mature. Note that the tibial tubercle is enlarged and there is an ossicle. A bursa was overlying this.
OSD is a very common cause of knee pain in children aged 8-15 years. This condition can have a prolonged course and cause loss of time from athletics. However, it is rarely a cause of permanent impairment or disability. (See Etiology and Prognosis.) [2]
Signs and symptoms
The onset of OSD is usually gradual, with patients commonly complaining of pain in the tibial tubercle and/or patellar tendon region after repetitive activities. Typically, running or jumping activities that significantly stress the patellar tendon insertion upon the tibial tubercle aggravate the patient's symptoms. They may even have waxing and waning of symptoms that correspond to variations in their athletic seasons. A sudden onset of pain with no antecedent symptoms in the region of the tibial tubercle should alert the clinician to assess for a possible acute tibial tubercle avulsion rather than OSD. (See Presentation for more detail.)
Diagnosis
Because of a lack of a precise etiology and therefore definition, some practitioners may find differentiating OSD from avulsion fractures of the tibial tubercle to be difficult. In general if the patient is unable to ambulate, an acute avulsion fracture of the tibial tubercle is more likely. OSD patients typically can ambulate, albeit with pain. (See Presentation and Workup for more detail.)
Management
OSD is a self-limiting condition. In a study by Krause et al, 90% of patients treated with conservative care were relieved of all of their symptoms approximately 1 year after onset of symptoms. [3] After skeletal maturity, patients may continue to have problems kneeling. This typically is due to tenderness over an unfused tibial tubercle ossicle or a bursa that may require resection. [4] Minimal association seems to exist between residual anterior knee pain after OSD and patellar stability, as was noted in the Krause study. The authors also noted no cases of recurvatum from premature closure of the proximal tibial physis. (See Treatment for more detail.)
Development of Osgood-Schlatter disease
The insertion of the patellar tendon at the tibial tubercle consists of cartilaginous tissue in girls younger than age 11 years and in boys younger than age 13 years. The secondary ossification center, or apophysis, of the tibial tubercle develops when girls are aged 10-12 years and when boys are aged 12-14 years. (During this stage of skeletal development, the Osgood-Schlatter lesion may occur.) (See Etiology.)
By the end of the ensuing 2 stages of bony development (eg, epiphyseal and bony stages), the primary growth plate of the proximal tibia and the secondary ossification center of the tibial tubercle fuse in males and females (usually when aged 14-18 y), and the OSD usually subsides.
The most commonly accepted theory regarding the development of OSD is that repeated traction (traction apophysitis) on the anterior portion of the developing ossification center leads to multiple subacute microavulsion fractures and/or tendinous inflammation, resulting in a benign, self-limited disturbance manifested as pain, swelling, and tenderness.
The most common long-term ramifications of OSD are pain on kneeling as an adult and the cosmesis of a bony prominence on the anterior knee. Less common complications are the persistence of a painful ossicle requiring surgical excision and a displaced avulsion of a tibial tubercle.
Patient education
Inform patients about activities that aggravate Osgood-Schlatter disease and about the self-limiting nature of the condition.
Etiology
The cause of Osgood-Schlatter disease (OSD) is unknown; however, theories suggest that this condition is a result of repeated knee extensor mechanism contraction that causes partial microavulsions of the chondrofibro-osseous tibial tubercle. This proposed pathophysiology is supported by the repetitive runner, jumper athletic patient population OSD occurs most commonly.
During running, jumping, gymnastics, and other sports requiring repeated contractions of the quadriceps, an extra-articular osteochondral stress fracture or microavulsion occurs. The proximal area of the patellar tendon insertion separates, resulting in elevation of the tibial tubercle. During the reparative phase of this stress fracture, new bone is laid down in the avulsion space, which may result in a deviated and prominent tibial tubercle. When an individual with an injured tibial tubercle continues to participate in sports, more and more microavulsions develop, and the reparative process may result in a markedly pronounced prominence of the tubercle, with longer-term cosmetic and functional implications. A separated fragment may develop at the patellar tendon insertion and may lead to chronic, nonunion-type pain.
In a magnetic resonance imaging (MRI) study of 20 patients with OSD, the patellar tendon was noted to attach more proximally and in a broader area to the tibia in patients with OSD. [5] Approximately 50% of patients with OSD relate a history of precipitating trauma.
Histologic studies support a traumatic etiology.
Risk factors
Risk factors for OSD include the following:
-
Age: females aged 8-12 years and males aged between 12 and15 years
-
Male sex (3:1)
-
Rapid skeletal growth
-
Repetitive sprinting and jumping sports
A study by Nakase et al found that quadriceps femoris muscle tightness and strength during knee extension and flexibility of the hamstring muscles were risk factors for incidence of Osgood-Schlatter disease. [6]
Epidemiology
Incidence
One study found that Osgood-Schlatter disease (OSD) affected approximately 21% of athletic adolescents surveyed, as compared with a frequency of 4.5% in age-matched nonathletic controls. [7]
One Finnish study found that OSD affected 13% of athletes.
Sex predilection
OSD occurs more frequently in boys, with a male-to-female ratio of 3:1.
Age predilection
OSD usually is seen in the adolescent years, after a patient has undergone a rapid growth spurt the previous year.
Girls who are affected are typically aged 10-11 years but can range from age 8-12 years.
Boys who are affected are typically aged 13-14 years but can range from age 12-15 years.
Prognosis
The prognosis in Osgood-Schlatter disease (OSD) is excellent. OSD is usually self-limiting and resolves by the time the patient is aged 18 years, when the tibial tubercle apophysis ossifies. [8] In approximately 10% of patients, however, the symptoms continue unabated into adulthood despite all conservative measures. [9] This may be from residual enlargement of the tuberosity or from ossicle formation in the patellar tendon.
The likelihood for long-term sequelae increases in severe cases, in cases in which treatment is not sought, or in cases in which the patient demonstrates poor compliance with the physician's recommendations.
In the study by Krause et al, 90% of patients treated with conservative care were relieved of all of their symptoms approximately 1 year following symptom onset. [3]
In some cases, however, discomfort may persist for 2-3 years until the tibial growth plate closes.
-
Radiograph of a patient who is skeletally mature. Note that the tibial tubercle is enlarged and there is an ossicle. A bursa was overlying this.
-
Radiograph of a patient who is skeletally immature. The tubercle is elongated and fragmented.
-
Courtesy of John T Killion, MD, OSA Pediatric Orthopaedics.
-
Courtesy of John T Killion, MD, OSA Pediatric Orthopaedics.