Practice Essentials
Pelvic fracture is a disruption of the bony structures of the pelvis, including pelvic ring fractures, acetabular fractures, and avulsion fractures. Generally, pelvic fractures occur because of high-energy trauma; however, elderly patients may suffer pelvic injuries caused by lower-energy mechanisms. The bony pelvis consists of the ilium, the ischium, and the pubis, which collectively form an anatomic ring with the sacrum. Disruption of this ring requires significant energy, often leading to multiple fractures. Because of the forces involved, pelvic fractures frequently cause injury to organs contained within the bony pelvis. In addition, trauma to extrapelvic organs is common. Pelvic fractures are often associated with severe hemorrhage because of the extensive blood supply to the region. [1, 2, 3, 4, 5, 6, 7]
Most commonly, pelvic fractures result from motor vehicle crashes, pedestrians being struck by motor vehicles, and falls. There tends to be a bimodal distribution of these injuries, with younger males sustaining high-energy pelvic fractures, along with associated traumatic injuries, and elderly females experiencing low-energy pelvic fractures without associated injuries. [8, 9]
Physical examination should not be used to rule out a pelvic fracture in unconscious patients, but it can nearly definitively rule it in. [10] The clinical exam is useful for patients who are awake and alert. [11] Signs that may suggest a pelvic fracture include hematuria; a hematoma over the ipsilateral flank, inguinal ligament, or proximal thigh or within the perineum; neurovascular deficits in the lower extremities; and rectal bleeding.
Anteroposterior pelvic radiography (see the image below) is a basic screening test for pelvic fracture and has historically been indicated in all blunt trauma patients according to Advanced Trauma Life Support (ATLS) protocols. For patients who are hemodynamically stable, it may be reasonable to forego pelvic plain films and rely on computed tomography (CT), as this will likely not change management or outcomes. [12, 13, 14, 15]
CT scanning (see the image below) has largely replaced plain radiography except for screening, and it has virtually eliminated the use of auxiliary views. By correctly identifying a pelvic ring injury, trauma surgeons and emergency physicians can provide adequate initial treatment and can convey important information about the anatomy of injured structures to the orthopedic surgeon who is managing the patient’s care. [16]
 Windswept pelvis (lateral compression injury) as seen on a pelvic CT scan. The patient sustained a left lateral compression injury with internal rotation of the left hemipelvis and a characteristic sacral buckle fracture. Note the concomitant left sacroiliac joint diastasis. The lateral force vector continued across the pelvis to produce external rotation of the right hemipelvis and diastasis of the right sacroiliac joint. The combination of injuries resulted in a windswept pelvis.
Windswept pelvis (lateral compression injury) as seen on a pelvic CT scan. The patient sustained a left lateral compression injury with internal rotation of the left hemipelvis and a characteristic sacral buckle fracture. Note the concomitant left sacroiliac joint diastasis. The lateral force vector continued across the pelvis to produce external rotation of the right hemipelvis and diastasis of the right sacroiliac joint. The combination of injuries resulted in a windswept pelvis.
The pelvis should be rapidly stabilized with a sheet or commercial pelvic external stabilizer. It is very important to perform this procedure before neuromuscular blockade, because the muscles alone may be maintaining pelvic stability. When stabilizing the pelvis, be sure to place the binder around the greater trochanters to provide adequate compression.
The primary treatment for pelvic fracture is the administration of narcotic analgesics for pain. One should avoid nonsteroidal anti-inflammatory drugs (NSAIDs) until hemorrhage has been excluded. If open pelvic fracture is diagnosed or suspected, empiric antibiotics should be given within 6 hours to prevent osteomyelitis. Initial therapy should target gram-positive organisms with antibiotics such as cefazolin. [17] If there is concern for associated perforation of the bowel or vagina, broad-spectrum antibiotic coverage against gram-negative and anaerobic pathogens should be considered. Patients with open pelvic fractures should also receive prophylaxis against tetanus.
Pathophysiology
Pelvic fractures are most commonly described using 1 of 2 classification systems. The Tile Classification is based on the integrity of the posterior sacroiliac complex, as well as the stability of rotational and vertical planes. The Young and Burgess Classification System is based on mechanism of injury: lateral compression, anterioposterior compression, vertical shear, or a combination of these forces.
Tile Classification System [18] (Open Table in a new window)
| Type A | Sacroiliac complex is intact. Stable fractures of the pelvic ring can be managed nonoperatively. |
| Type B | Rotationally unstable, vertically stable. This occurs as the result of external or internal rotation forces causing partial disruption of the posterior sacroiliac complex. |
| Type C | Rotationally and vertically unstable. Complete disruption of the posterior sacroiliac complex is seen. |
Young and Burgess Classification System [19] (Open Table in a new window)
| Lateral Compression | |
|---|---|
| Grade I | Sacral compression fracture on side of impact. |
| Grade II | Sacral compression fracture with associated posterior iliac fracture on side of impact. |
| Grade III | Type I or II plus associated contralateral sacroiliac joint injury. |
| Anterior-Posterior Compression | |
| Grade I | Mild widening of the pubic symphysis with intact posterior pelvic ring ligaments and sacroiliac ligaments. |
| Grade II | Diastasis of pubic symphysis with associated anterior sacroiliac joint widening and intact posterior sacroiliac joint ligaments. |
| Grade III | Diastasis of pubic symphysis with complete disruption of sacroiliac joint and posterior pelvic ring ligaments. |
| Vertical Shear | Displacement of the hemipelvis superiorly or posteriorly involving diastasis of the pubic symphysis, fractures of the rami, displacement of the sacroiliac joint, and/or fractures of the iliac wing or sacrum. |
| Combined Mechanism | Because of the high-energy nature of these injuries, the mechanisms are often combined and difficult to determine and categorize. |
(See the images of anterior-posterior compression and vertical-sheer fractures below.)
A comparison of Tile and Young and Burgess classification systems applied to a group of trauma patients with pelvic ring fractures showed no difference in predictive value for mortality, need for transfusion, or associated injuries. [20] Intraobserver and interobserver variability among orthopedic surgeons asked to use these systems to classify pelvic fractures may limit their utility. [21]
Acetabular fractures most commonly involve disruption of the acetabular socket when the hip is driven backward in a motor vehicle accident. Occasionally, they occur in a pedestrian struck by a vehicle moving at a significant rate of speed.
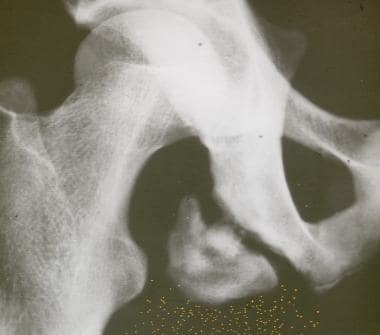
Pelvic avulsion fractures (see the image below) occur as the result of indirect trauma from sudden muscular contraction causing injury to the muscular attachment on the pelvis. These most often occur in skeletally immature athletes because of inherent weakness of the pelvic apophyses. The 3 most common sites are the anterior superior iliac spine (ASIS), the anterior inferior iliac spine (AIIS), and the ischial tuberosity, because of contraction of the sartorius, rectus femoris, and hamstring muscles, respectively. [22]
Epidemiology
Pelvic fractures constitute about 3% of all skeletal injuries. Open pelvic fractures are rare and represent only 2-4% of all pelvic fractures. [23] Of all pelvic ring fractures, approximately 55% are stable, whereas 25% have rotational instability and 20% have rotational and vertical instability. Approximately 16% of patients have associated acetabular fractures. [24]
A study of a large patient database in the United States found that around 70% of patients who sustain pelvic ring fractures are female. [25] A trauma registry review from New South Wales, Australia, revealed that most patients who sustain high-energy pelvic ring fractures, such as from a motor vehicle crash, are male, whereas low-energy injuries predominantly occur in females. [9] Males also sustain associated genitourinary injuries more commonly than females. [26]
In the United States, the incidence of pelvic fracture is highest among those between the ages of 15 and 28 years. For persons younger than 35 years, men are more commonly affected, whereas for those older than 35 years, women are more commonly affected. [16] A large patient database review found that the mean age of patients who sustain a pelvic ring fracture is about 65 years. Average age actually increased significantly over the 17-year study period, which may represent an increase in low-energy pelvic fractures. [25]
Prognosis
Mortality/Morbidity
Analysis of a database of more than 63,000 trauma patients revealed that pelvic fracture was associated with higher mortality compared to trauma without pelvic fracture; however, these studies are difficult to interpret because of confounders. Because pelvic fractures generally occur via high-energy mechanisms, patients are more likely to suffer other associated injuries that may contribute to increased mortality. [27]
Cited mortality in patients with any type of pelvic fracture ranges from 4 to 15%. In-hospital mortality among patients with unstable fractures is 8.3%. Mortality is 21.3% in the subset of patients with open unstable fractures. [28]
One study of pelvic fractures in children aged 16 years or younger cited mortality of 5%, with death most commonly due to hemorrhage or multiple injuries. [29] Among hemodynamically unstable patients, pelvic hemorrhage is venous in origin in 80-90% of cases. [30]
Despite aggressive intervention, elderly patients with pelvic fractures have worse outcomes than younger patients with similar injuries. [28, 31]
Ultimately, the patient's Injury Severity Score—not the nature of the pelvic fracture—is the best predictor of mortality. Hemorrhage, either pelvic or extrapelvic, and associated severe head injury are the most common causes of early death, whereas multisystem organ failure and sepsis resulting from soft tissue infection near the fracture site are the main reasons for delayed death. [32]
Patients with pelvic fractures combined with acetabular fractures have higher Injury Severity Scores and mortality rates and a greater need for transfusion than those with either type of fracture alone. [33]
The complication rate associated with pelvic fractures is significant and is related to injury of underlying organs, bleeding, and multiorgan system failure. [34] Because of the tremendous force necessary to cause most unstable pelvic fractures, concomitant severe injuries are common and are associated with high morbidity and mortality.
Blunt traumatic extraperitoneal bladder rupture is a rare occurrence that typically is associated with concomitant pelvic fracture in patients presenting with hematuria. This injury tends to occur as a result of high-impact motor vehicle or motorcycle collisions and is associated with increased morbidity and mortality. Dedicated bladder imaging should be considered in blunt abdominopelvic trauma patients presenting with hematuria in the absence of pelvic fracture when the patient's underlying medical conditions or comorbidities increase the risk of bladder rupture. [35]
Although transarterial embolization (TAE) is an effective way to control arterial bleeding associated with pelvic fracture, clinical outcomes according to door-to-embolization (DTE) time are unclear. A retrospective review concluded that shorter DTE time was associated with better survival in the first 24 hours, as well as other clinical outcomes, in patients with complex pelvic fracture who underwent TAE. Efforts to minimize DTE time are recommended. [36]
Pelvic fractures increase the incidence of pulmonary emboli. [37]
Lower long-term quality of life based on validated questionnaires has been reported among patients with pelvic fractures following high-energy trauma. [38, 39]
Increasing life expectancy has led to higher incidence of fragility fractures of the pelvis. These demographic changes may have a direct impact on fracture patterns. A retrospective cross-sectional study conducted at a Swiss trauma center evaluated demographic trends in patients with pelvic ring injury and analyzed the influence of these trends on fracture patterns. Study results corroborate the trend of increasing frequency of fragility fractures in an aging society. This demographic shift has a direct impact on fracture pattern, with a disproportionate increase in partially stable compression fractures of the pelvis. [40]
-
Anterior-posterior (AP) compression pelvic fracture.
-
Vertical shear (VS) fracture pattern.
-
Anteroposterior (AP) compression injury as seen on an AP radiograph of the pelvis. Characteristic features of an AP compression injury include symphyseal and sacroiliac joint diastasis. In this patient, the pubic symphysis and right sacroiliac joint are widened.
-
Windswept pelvis (lateral compression injury) as seen on a pelvic CT scan. The patient sustained a left lateral compression injury with internal rotation of the left hemipelvis and a characteristic sacral buckle fracture. Note the concomitant left sacroiliac joint diastasis. The lateral force vector continued across the pelvis to produce external rotation of the right hemipelvis and diastasis of the right sacroiliac joint. The combination of injuries resulted in a windswept pelvis.
-
Pelvic apophyseal avulsion fracture of the ischial tuberosity due to contraction of the hamstring muscles. Courtesy of Wikipedia (https://de.wikipedia.org/wiki/Apophyse).