Practice Essentials
Piebaldism is a rare autosomal dominant disorder of melanocyte development characterized by a congenital white forelock and multiple symmetrical hypopigmented or depigmented macules. This striking phenotype of depigmented patches of skin and hair has been observed throughout history, with the first descriptions dating to early Egyptian, Greek, and Roman writings. Generation after generation demonstrated a distinctive, predictable familial mark—a white forelock. Families have sometimes been known for this mark of distinction, carrying such surnames as Whitlock, Horlick, and Blaylock. Note the image below.
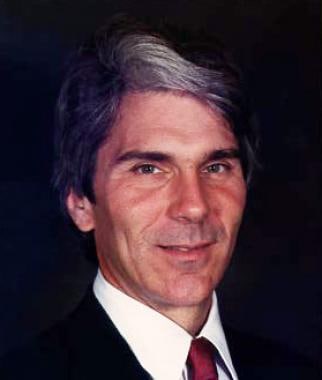 Distinguished physician with mark of distinction, a white forelock that his father and grandfather also shared.
Distinguished physician with mark of distinction, a white forelock that his father and grandfather also shared.
The word piebald itself has been attributed to a combination of the "pie" in the magpie (a bird of black and white plumage) and the "bald" of the bald eagle (the United States' national bird, which has a white feathered head).
Piebaldism is due to an absence of melanocytes in affected skin and hair follicles as a result of mutations of the KIT proto-oncogene. [1] As of a 2001 review by Richards et al, 14 point mutations, 9 deletions, 2 nucleotide splice mutations, and 3 insertions of the KIT gene were believed to be mutations causing piebaldism. [2] The severity of phenotypic expression in piebaldism correlates with the site of the mutation within the KIT gene. The most severe mutations seem to be dominant negative missense mutations of the intracellular tyrosine kinase domain, whereas mild piebaldism appears related to mutations occurring in the amino terminal extracellular ligand-binding domain with resultant haplo insufficiency. A novel deletion mutation of KIT gene was described in a 5-generation Chinese family. [39]
Most piebald patients have the above-described mutation of the KIT gene encoding a tyrosine kinase receptor involved in pigment cell development. [3] The white hair and patches of such patients are completely formed at birth and do not usually expand thereafter. However, 2 novel cases of piebaldism were described in which both mother and daughter had a novel Val620Ala mutation in their KIT gene and showed progressive depigmentation. These findings are consistent with the hypothesis that progressive piebaldism might result from digenic inheritance of the KIT (V620A) mutation that causes piebaldism and a second, unknown locus that causes progressive depigmentation. [4] Another novel mutation in KIT was described in 2 Japanese individuals. [5]
Piebaldism is one of the cutaneous signs of Waardenburg syndrome, along with heterochromia of the irides, lateral displacement of inner canthi, and deafness. [6, 7] Also see Genetics of Waardenburg syndrome.
Etiology
Piebaldism is a rare autosomal dominant genetic disorder Basically, it is a complex interconnecting regulatory network of mutated genes and synergistic interactions. [8, 17]
Prognosis
Piebaldism is a benign disorder. However, patients are at risk for actinic complications related to absence of cutaneous melanocytes. Although spontaneous repigmentation in an infant with piebaldism has been described, it is most unusual. [18]
History
Graft versus host disease may arise solely within an area affected by piebaldism; therefore, piebaldism-affected skin may be immunologically different from normal skin. [19]
Diagnostics
Targeted next-generation sequencing can be effectively used for molecular diagnosis. [30]
Regarding histology findings, poliosis has either decreased or absent melanin and/or melanocytes in the hair bulbs of the affected hair follicles, which can be confirmed using special stains for melanin or melanocytes. [28] The epidermal melanocytes are usually unaffected unless there is also vitiligo.
Treatment
See Treatment.
Pathophysiology
Piebaldism is an autosomal dominant genetic disorder of pigmentation characterized by congenital patches of white skin and hair that lack melanocytes. [8] Piebaldism results from mutations of the KIT proto-oncogene, which encodes the cell surface receptor transmembrane tyrosine kinase for an embryonic growth factor, steel factor. [9] Several pathologic mutations of the KIT gene now have been identified in different patients with piebaldism. [10] Correlation of these mutations with the associated piebald phenotypes has led to the recognition of a hierarchy of 3 classes of mutations that result in a graded series of piebald phenotypes. KIT mutations in the vicinity of codon 620 lead to the usual phenotype of static piebaldism. Mutations of the KIT proto-oncogene produce variations in phenotype in relation to the site of the KIT gene mutation.
In an analysis of 26 unrelated patients with piebaldismlike hypopigmentation (ie, 17 typical patients, 5 patients with atypical clinical features or family histories, and 4 patients with other disorders that involve white spotting), novel pathologic mutations or deletions of the KIT gene were observed in 10 (59%) of the typical patients and in 2 (40%) of the atypical patients. Overall, pathologic KIT gene mutations were identified in 21 (75%) of 28 unrelated patients with typical piebaldism. Patients without apparent KIT mutations had no apparent abnormalities of the gene encoding steel factor itself; however, genetic linkage analyses in 2 of these families implied linkage of the piebald phenotype to KIT. Thus, most patients with typical piebaldism seem to have abnormalities of the KIT gene. A complex network of interacting genes regulates embryonic melanocyte development.
Piebaldism almost always has a static course. Genetic analysis of a mother and daughter with progressive piebaldism revealed a novel Val620Ala (1859T>C) mutation in the KIT gene. This KIT mutation and others of the tyrosine kinase domain affect the intracellular tyrosine kinase domain and may imply a severe phenotype. [11] This is a newly described phenotype with melanocyte instability leading to advancing loss of pigmentation and the progressive appearance of the hyperpigmented macules.
A South African girl of Xhosa ancestry with severe piebaldism and profound congenital sensorineural deafness had a novel missense substitution at a highly conserved residue in the intracellular kinase domain of the KIT proto-oncogene, R796G. Although auditory anomalies in mice with dominant white spotting due to KIT mutations may occur, deafness is not typical in human piebaldism. Thus, sensorineural deafness extends considerably the phenotypic range of piebaldism due to KIT gene mutation in humans and strengthens the clinical similarity between piebaldism and the various forms of Waardenburg syndrome. [7] A novel mutation of the KIT gene was described in a Chinese family with piebaldism. [12] In 2017, a novel missense mutation in TK1 region of KIT was described in a Chinese family with severe piebaldism. [13]
Manipulation of the mouse genome may be an important approach for studying gene function and establishing human disease models. [14] Mouse mutants generated and screened for dominant mutations yielded several mice with fur color abnormalities. One causes a phenotype similar to dominant-white spotting (W) allele mutants. This strain may serve as a new disease model of human piebaldism.
Genetic factors determining piebaldism in Italian Holstein and Italian Simmental cattle breeds were studied. [15] Variability in the microphthalmia-associated transcription factor gene explained the differences between spotted and nonspotted phenotypes, although other genetic factors were also important.
A splicing mutation, producing the deletion of exon 17 of KIT, and co-segregated it with 2 phenotypes of the severe form of piebaldism and auburn hair color was documented in a Chinese Han family. [16]
Patient Education
Educate patients about the genetic transmission of the disorder.
Educate patients about use of sunscreens, sunprotective measures (eg, wide-brimmed hat, long-sleeved shirts, long pants), sun avoidance during peak hours of ultraviolet exposure during the day, and self-examinations because recurrent sun damage may result in an increased risk of cutaneous malignancy.
Patients who are self-conscious about the appearance of their skin may benefit from use of a camouflage cover-up, such as Dermablend or other similar camouflage measures.
-
Distinguished physician with mark of distinction, a white forelock that his father and grandfather also shared.



