Practice Essentials
Erythema dyschromicum perstans (ashy dermatosis) is a distinct and somewhat controversial cutaneous eruption that may be best regarded as a form of lichen planus or lichen planus actinicus. [1, 2, 3] A consensus on terminology has been delineated. [4] Some favor a new entity, identified as acquired macular pigmentation of unknown etiology, under which the rubric erythema dyschromicum perstans, ashy dermatosis, lichen planus pigmentosus, and idiopathic eruptive macular pigmentation would fit. [5] Acquired dermal macular hyperpigmentation is an almost identical and preferable alternative umbrella term. [6]
Signs and symptoms
Erythema dyschromicum perstans has a slow onset and is unlikely to resolve spontaneously. [7] The clinical course of childhood (prepubertal) may differ from that of adults; erythema dyschromicum perstans may be more likely to resolve within 2-3 years. A proposed clinical classification has been devised, dividing ashy dermatoses from erythema dyschromicum perstans with the former lacking erythematous borders, and having a third category for simulators such as lichen planus variants, and medication-induced melanodermas. [8]
Erythema dyschromicum perstans is an asymptomatic eruption of oval, polycyclic, or irregularly shaped, gray-blue hyperpigmented macules on the trunk, the arms, the face, and the neck. It begins as ash-colored macules, sometimes with an erythematous or elevated border (see the image below). No systemic symptoms or associations exist.
Erythema dyschromicum perstans may resolve in 2-3 years in prepubertal children, but it is more likely to persist in adults. [9]
 Ash-colored, partially confluent, macular lesions over the patient's back. Reprint with permission from Cutis 1986; 37: 42-44.
Ash-colored, partially confluent, macular lesions over the patient's back. Reprint with permission from Cutis 1986; 37: 42-44.
On physical examination, erythema dyschromicum perstans has asymptomatic, gray-blue hyperpigmented patches of variable shape and size and an elevated erythematous border in the early stages (see the image below). The eruption is symmetrically distributed on the face, the trunk, and the upper extremities. The oral cavity and the genitals are spared. Dermatoscopic features are variable. [10] Pigmentation on dermatoscopic examination is due to epidermal papillomatosis, and small brown dots correspond to pigmentary incontinence, two findings, which, when combined, may produce a “Wagyu beef–like” appearance. [11]
 Close-up photograph shows ash-colored macular lesions and lack of an inflammatory border. Reprint with permission from Cutis 1986; 37: 42-44.
Close-up photograph shows ash-colored macular lesions and lack of an inflammatory border. Reprint with permission from Cutis 1986; 37: 42-44.
Diagnostics
Erythema dyschromicum perstans (EDP) patients have negative laboratory study results, which include the following:
-
Bacterial, viral, and mycologic cultures
-
Erythrocyte sedimentation rate
-
Glucose studies
-
Liver function test
-
Urinalysis
Radiographic studies in EDP patients have not shown abnormalities.
Histologic findings
The biopsy specimen is obtained as much to rule out other diagnoses as to confirm that of erythema dyschromicum perstans because the EDP histologic pattern is relatively nonspecific. One should attempt to obtain a biopsy sample of the border of an active macule, which usually demonstrates mild basal cell layer vacuolar degeneration overlying an upper dermis with a mild perivascular mononuclear cell infiltrate and increased melanophages.
Distinguishing ashy dermatosis from lichen planus pigmentosus (LPP) is not always easy. A Mexican study of 20 patients with EDP and 11 with LPP provided clear clinical delineation between the 2 often histologically indistinguishable disorders. [12] LPP has pruritic brownish black macules or patches, with no active border, on the face and the flexor folds. EDP does not involve mucosal surfaces, where LPP does. In favor of EDP being either a subset of idiopathic lichen planus or a lichenoid drug eruption are reports of lichen planus and EDP occurring in the same patient, the clinical resemblance of EDP to atrophic lichen planus, and similar histologic patterns with immunofluorescence in both EDP and LPP.
The border of an active EDP lesion and the border of an LPP lesion often both show hyperkeratosis, a thinned epidermis, hydropic degeneration of the basal layer, pigment incontinence, and a perivascular lymphohistiocytic infiltrate (see the images below). Colloid bodies are occasionally seen in both.
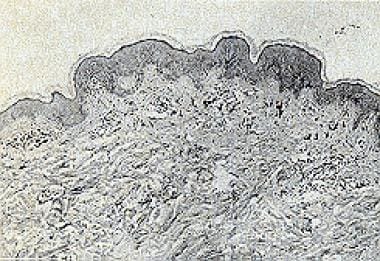 Photomicrograph of a lesion on the patient's back shows slight basilar vacuolar change, extensive pigment incontinence, dilatation of dermal lymphatics, and lack of inflammation (hematoxylin & eosin, original magnification X24.8). Reprint with permission from Cutis 1986; 37: 42-44.
Photomicrograph of a lesion on the patient's back shows slight basilar vacuolar change, extensive pigment incontinence, dilatation of dermal lymphatics, and lack of inflammation (hematoxylin & eosin, original magnification X24.8). Reprint with permission from Cutis 1986; 37: 42-44.
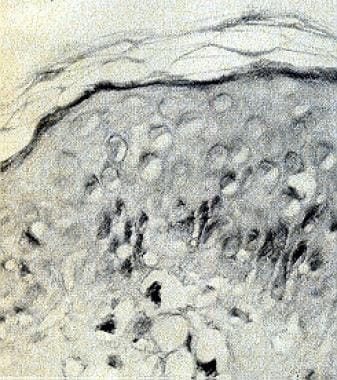 Higher-power photograph shows slight vacuolar basilar change, marked dilatation of intradermal lymphatics, incontinence of melanin pigment, and lack of inflammation (hematoxylin & eosin, original magnification X238). Reprint with permission from Cutis 1986; 37: 42-44.
Higher-power photograph shows slight vacuolar basilar change, marked dilatation of intradermal lymphatics, incontinence of melanin pigment, and lack of inflammation (hematoxylin & eosin, original magnification X238). Reprint with permission from Cutis 1986; 37: 42-44.
Immunopathologic study of EDP shows immune-associated (Ia) antigen expression in keratinocytes and strong OKT 4 and OKT 6 staining of Langerhans cells. It also shows dermal infiltration by T lymphocytes of both helper-inducer and suppressor-cytotoxic phenotypes, a pattern commonly seen with lichen planus. CD36 expression is evident in the viable upper epidermis on lesional keratinocytes, which may imply a delayed hypersensitivity reaction. Beneath, in the dermis, the cellular infiltrate has been found to express CD69 and the cytotoxic cell marker CD94. In addition, as with lichen planus, the colloid bodies stained immunoglobulin G positive.
Ultrastructural findings demonstrate immature, small, irregular-shaped melanosomes in melanocytes and peripheral localization of melanosomes in keratinocytes. [13]
Management
Many therapeutic options are available for erythema dyschromicum perstans (EDP), but few have been effective, except for clofazimine. In one series of 8 patients, 7 had a good or excellent response to clofazimine administered either 100 mg every other day to patients weighing less than 40 kg or 100 mg every day to patients weighing more than 40 kg. This medication was continued for 3 months, then reduced to 200 mg/wk and 400 mg/wk, respectively. The one remaining patient had only a marginal response. One study found some improvement in early cases, but no cures were reported. This medication seems to have a valuable effect on the inflammatory phase of EDP.
Clofazimine is a lipophilic rhimophenazine dye with both antimicrobial and anti-inflammatory properties originally developed to treat tuberculosis. Although its mechanism of action is unclear, it seems to exert its main effect upon neutrophils and monocytes in a variety of ways, such as stimulating phagocytosis and release of lysosomal enzymes. [14]
Clofazimine is administered orally, with improved bioavailability when taken with food. It concentrates in lipid-rich tissues, including the reticuloendothelial system, the intestine, the breasts, and the liver. Its half-life is 70 days. Isoniazid increases its serum levels and enhances its urinary excretion. Its most common adverse effects are in the skin, the gut, and the eye. It gives a temporary orange discoloration of the skin and the eye (ie, cornea, conjunctivae); it also may produce ichthyosis. Its most serious adverse effect is crystal deposition in the gut that produces a potentially fatal enteropathy. This rare complication is associated with months of high-dose (>100 mg/d) therapy. Nausea and diarrhea are more common. Splenic infarction and eosinophilic enteritis are also rare adverse effects.
Many other therapeutic modalities have been attempted, none with satisfactory results. These include ultraviolet exposure, ultraviolet avoidance, antibiotics, antihistamines, griseofulvin, chemical peels, antibiotics, corticosteroids, vitamins, isoniazid, chloroquine, and psychotherapy. The use of narrow-band UVB phototherapy has shown success in a few patients. [15, 16] A low-potency topical steroid applied twice a day to the affected areas may be used, with or without a 4% hydroquinone cream for the hyperpigmentation. [17] A favorable result with isotretinoin has been observed. [18] A patient from Turkey was described to have responded remarkably well to treatment with dapsone. [19] Combination nonablative fractional photothermolysis and topical tacrolimus ointment may be a safe and effective option. [20] Tacrolimus also may be used successfully as monotherapy. [21]
Background
C. Oswaldo Ramirez of San Salvador, El Salvador, first described erythema dyschromicum perstans (EDP) in 1957. [22] He called the patients with this eruption Los cenicientos, meaning the ashen ones. The Spanish term cenicienta also means Cinderella because of this folklore character's close association with ashes from sitting at home alone by the fireplace. Later, erythema dyschromicum perstans was called dermatosis ceniciento, meaning ashy dermatosis, because of its ashy bluish gray color. The term erythema dyschromicum perstans is credited to Marion B. Sulzberger, who suggested it when examining Convit's [23] patients in Caracas. Sulzberger's comment, in discussion of another paper, is as follows:
... the narrow red border (which is often hard to find), represents the active lesions. This is why I suggested a name which contains the term "erythema" and which also suggests the variety and persistence of the final dyschromias.
The descriptive term ashy dermatosis was also used as a designation for their coloration. In South America, another name, erythema chronicum figuratum melanodermicum, is also used.
Pathophysiology
The etiology of erythema dyschromicum perstans is unknown, but many consider erythema dyschromicum perstans to be a variant of lichen planus actinicus. A variety of predisposing factors have been cited. These include ingestion of ammonium nitrite, an intestinal parasitosis caused by nematodes (whipworm infection, control of which produced erythema dyschromicum perstans remission), orally administered radiographic contrast media, and, possibly, an occupationally associated cobalt allergy in a plumber. One case may be particularly revealing, that of a 13-year-old rural northern European truant who repeatedly ingested small amounts of a fertilizer, ammonium nitrate, to induce erythema dyschromicum perstans and avoid school. Chlorothalonil exposure among banana farm workers is another possible cause of erythema dyschromicum perstans. [24]
An abnormality in cell-mediated immunity might play a role. However, substantial immune dysfunction is limited at present to 1 report of an HIV-seropositive 41-year-old homosexual patient of Chinese lineage with erythema dyschromicum perstans. [25, 26]
HLA-DR association with the genetic susceptibility to develop ashy dermatosis in Mexican Mestizo patients was analyzed, the results of which were reported by Correa in 2007. [27] The most frequent allele was HLA-DR4 (65%), compared with 23% in controls. These Mexican patients had HLA-DR4 subtype *0407, which is also found in the Amerindian population. [28, 29] Thus, although many factors may be involved, an important genetic susceptibility appears to be conferred by genes located within the major histocompatibility complex region.
Etiology
The etiology of erythema dyschromicum perstans remains unknown. It has been associated with ingestion of ammonium nitrate and whipworm infestation, but a specific etiology has not been established in any instance. The geographical distribution of erythema dyschromicum perstans has led some authors to suggest environmental factors, but all attempts to find these pollutants have failed.
Epidemiology
Frequency
Erythema dyschromicum perstans is most common in Latin America and Asia; most of the cases occur in El Salvador where the first case was identified. Cases in Europe have also been described, including in Italy. [30]
Race
Darker-skinned individuals seem to be affected more often than lighter-skinned individuals. It is a rare disorder of pigmentation that is most common in Hispanic patients. [7] It may also occur in children from the Indian subcontinent. [31] Unlike adult patients, who are most commonly of Hispanic origin, children with erythema dyschromicum perstans are usually white. [32, 33]
Sex and age
Both sexes are affected, but women are affected more often than men.
The age range affected is wide, both in Latin America and around the world. Erythema dyschromicum perstans has been observed in children aged 1 year and adults aged 80 years. For example, a 6-year-old British girl and 4 Finnish children aged 8-12 years were described, as were many older patients. An early report had a series of 5 patients; 3 males aged 11-36 years and 2 women.
Prognosis
Erythema dyschromicum perstans may persist for years. Erythema dyschromicum perstans has a benign outcome, with most complaints relating to cosmetic issues.
-
Ash-colored, partially confluent, macular lesions over the patient's back. Reprint with permission from Cutis 1986; 37: 42-44.
-
Close-up photograph shows ash-colored macular lesions and lack of an inflammatory border. Reprint with permission from Cutis 1986; 37: 42-44.
-
Photomicrograph of a lesion on the patient's back shows slight basilar vacuolar change, extensive pigment incontinence, dilatation of dermal lymphatics, and lack of inflammation (hematoxylin & eosin, original magnification X24.8). Reprint with permission from Cutis 1986; 37: 42-44.
-
Higher-power photograph shows slight vacuolar basilar change, marked dilatation of intradermal lymphatics, incontinence of melanin pigment, and lack of inflammation (hematoxylin & eosin, original magnification X238). Reprint with permission from Cutis 1986; 37: 42-44.





