Practice Essentials
Injuries to the peroneal tendons are common but not always clinically significant. [1] They are misdiagnosed as a lateral ankle sprain most of the time, because isolated injury to the peroneal tendons is rare. [2, 3, 4] Injury can occur in one or both peroneus longus and brevis tendons and is typically classified as acute or chronic. Function can be severely compromised by any tendon disruption; conversely, complete tendon rupture can be asymptomatic. Lesions have been seen in symptomatic patients, as well as in cadaver studies of patients who were presumably asymptomatic. [5] The reason for this variation is not known.
The image below depicts the anatomy of the lateral ankle.
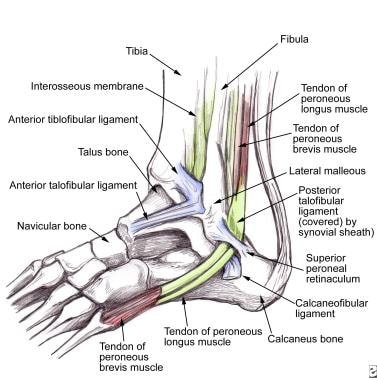 Lateral ankle anatomy demonstrates the peroneal tendons as they course beneath the superior retinaculum. The anterior talofibular, calcaneofibular, and posterior talofibular ligaments are also shown.
Lateral ankle anatomy demonstrates the peroneal tendons as they course beneath the superior retinaculum. The anterior talofibular, calcaneofibular, and posterior talofibular ligaments are also shown.
Acute injuries of the peroneal tendons include tendinitis, tear/rupture, laceration, and dislocation/subluxation. Acute injuries typically have 1 of 2 mechanisms as the cause: (1) inversion ankle injury, which is often seen with associated anterior talofibular ligament and/or calcaneofibular ligament disruption, and (2) a powerful contraction of the peroneal muscles with a forcefully dorsiflexed foot.
Chronic injuries include longitudinal tears [6, 7, 8, 9, 10] and recurrent subluxation [11, 12, 13] of the peroneus brevis tendon. [14] These chronic injuries are usually associated with ankle or subtalar arthritis and ankle instability. People with "bad" or "weak" ankles may have peroneal tendon pathology. Core and lower extremity biomechanics must be evaluated in any chronic atraumatic peroneal tendinopathy, as flaws in those mechanics are usually the culprit.
Magnetic resonance imaging (MRI) is the criterion standard for identifying peroneal tendon injuries, which are demonstrated by the high signal intensity within the affected tendon on T2-weighted axial views. [7, 15, 16, 17, 18]
In the acute phase, most ankle injuries are managed with rest, ice, compression, and elevation (RICE), with or without a short period of no weight bearing. Nonsteroidal anti-inflammatory drugs (NSAIDs) can also be prescribed to reduce inflammation and pain. Once the swelling and pain have decreased, a more extensive examination can be performed. If the symptoms are minimal and if no significant instability is present, a rehabilitation program can be started. This program should include an ankle strengthening, flexibility, and proprioception regimen.
Surgery is indicated in the acute phase for peroneus brevis tendon rupture, acute dislocation, and anomalous peroneal brevis muscle hypertrophy and for peroneus longus tears that are associated with diminished function. [19, 20, 21]
For excellent patient education resources, visit eMedicineHealth's First Aid and Injuries Center.
Etiology
Most peroneal tendon injuries are caused by the typical acute or recurrent lateral ankle sprain. As stated earlier, isolated injury to the peroneal tendons is rare.
-
Acute injury involves forceful dorsiflexion with contraction of the peroneal muscles or an inversion injury with a high load. Most acute injuries have subacute and chronic tendinopathy.
-
Chronic injury involves repeated inversion injuries, damage to the posterior talofibular and lateral malleolar retinaculum, and/or recurrent dislocation of the peroneal tendons, leading to chronic tears and lateral ankle instability. (See the image below.)
Biomechanical factors can set up the peroneal tendons for injury.
-
Gait abnormalities must be fully evaluated and treated. Excessive eversion can pinch and put pressure on the peroneal tendons as they travel between the lateral malleolus and the peroneal trochlea.
-
Severe pes planus or hindfoot deviation (valgus or varus) can be a factor.
-
Equinus or restricted ankle dorsiflexion can lead to injury of the peroneal tendons.
-
Anterolateral ankle impingement, particularly soon after an ankle sprain, can lead to peroneal overcompensation.
-
Poor fitting equipment, such as ice skates or basketball high-top shoes, can be factors in peroneal tendon injuries. [22]
Epidemiology
United States statistics
The occurrence of injuries to the peroneal tendons is not actually known. DiGiovanni et al found that 25-77% of patients with chronic lateral ankle instability had some type of injury to the peroneal tendons. [23] Over 33 months, Fallat et al noted that of 638 acute ankle "sprains" seen at the Oakwood Hospital Downriver Center Emergency Room and Occupational Medicine Clinic in Dearborn, Michigan, only 83 involved damage to the peroneal tendons, whereas more than 450 involved the anterior talofibular ligament. [1]
Functional Anatomy
The peroneal tendons originate in the lateral compartment of the leg. The peroneus longus originates from the head and proximal two thirds of the fibula, whereas the peroneus brevis originates from the distal two thirds of the fibula. Both tendons have a musculotendinous portion that courses just below the lateral malleolus.
At the posterior aspect of the lateral malleolus, the peroneal tendons lie within the fibular groove, with the peroneus brevis medial and anterior to the peroneus longus. The fibular groove forms the anterior border of the fibro-osseous tunnel that the peroneal tendons course through. The inferior retinaculum and the calcaneofibular ligament form the posterior border.
The posterior talofibular and the calcaneofibular ligaments form the medial border. The superior retinaculum forms the lateral border. Just inferior to the lateral malleolus, the peroneus brevis courses anteriorly, crossing over the cuboid to insert on the fifth metatarsal styloid. (See the following image.)
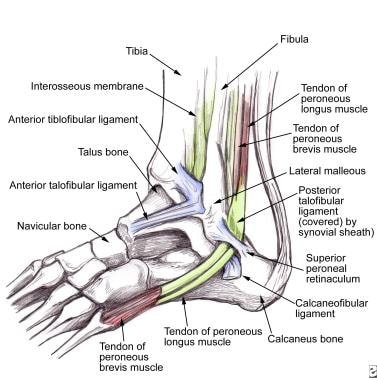 Lateral ankle anatomy demonstrates the peroneal tendons as they course beneath the superior retinaculum. The anterior talofibular, calcaneofibular, and posterior talofibular ligaments are also shown.
Lateral ankle anatomy demonstrates the peroneal tendons as they course beneath the superior retinaculum. The anterior talofibular, calcaneofibular, and posterior talofibular ligaments are also shown.
Inferior to the peroneus brevis, the peroneus longus turns beneath the cuboid in a tunnel formed by the long plantar ligament and the groove of the cuboid. It then courses to insert onto the first metatarsal and medial cuneiform. In 20% of the population, an os peroneum may be present within the peroneus longus tendon as it turns under the cuboid bone. In 0.1% of the population, a structure known as the os vesalianum—a sesamoid bone—is found at the insertion of the peroneus brevis tendon.
A common variant in anatomy—the peroneus quartus muscle—occurs in approximately 6.6% of the population. Although the muscle may have a number of different attachments, it most commonly arises from the peroneus brevis muscle and is inserted into the retrotrochlear eminence of the calcaneus.
Sport-Specific Biomechanics
Basic
Most sports have elements of running and lateral movement. Sports such as soccer, basketball, and football can be highly demanding on the lower extremity.
The role of the peroneus muscles is to evert the ankle and stabilize its subtalar motion. In balancing the foot, they play off the posterior tibialis muscle on the opposite side of the tibia. Maximal exertion occurs with side-to-side movement and jumping.
The importance of the peroneus muscles is most obvious after lateral ankle sprains. Trauma to the lateral ankle distorts the proprioceptive sense and stretches the connective tissues. The peroneus muscles are often stretched and injured from traction when the foot inverts.
Ankle instability ensues and continues until the lateral retinaculum heals, the peroneal muscles recover, and proprioception returns. If the retinaculum does not heal properly and cannot retain its tension to stabilize the peroneal tendons, symptoms of instability may not resolve without further intervention.
An analysis of overall biomechanics is essential in finding out the factors involved with peroneal tendon damage, especially when there is no traumatic insult. Leg-length discrepancies, femoroacetabular impingement, core instability, and low back pain are some of the correlated factors involved with lower extremity repetitive injuries, but little research has cemented the relationship. However, the core is the powerhouse of the body, and if foot planting is not well controlled by the hip and thigh, then extraneous forces run through the lower leg, ankle, and foot. This can only be controlled by increasing the activity of the supporting muscles, of which the peroneal tendons belong.
Role of core stability
Somatic dysfunctions in the lumbosacropelvic region can inhibit muscle firing. One of the most common causes of dysfunctions in a patient who is active and typically has no functional issues is limping, something that happens quite frequently with traumatic ankle injuries.
When the core is destabilized, the following problems may develop, not all of which are conscious to the patient:
Gluteus medius muscle firing is slower and weaker, allowing more femoral adduction and internal rotation with gait. The tensor fascia latae tends to avoid such inhibition and instead tightens up. This is a common cause of lateral snapping hip syndrome.
Functional short leg may develop. This is related to rotation of the ilium, sacral torsion or shear, hypertonic psoas major, quadratus lumborum, or iliacus muscle, lumbar rotational dysfunction, or all of the above. This shifts load onto one side more than the other and rotates the talus within the mortise, thus increasing pronation.
Low back tightness or soreness with prolonged sitting or standing can develop, which restricts hip extension, leading to more stress on the ankle.
An astute physical therapist evaluates the kinetic chain for these problems. A rushed examination that targets only the location of pain misses all this and leads to prolonged pain and disability. Once the core muscles develop a maladaptive compensation pattern, the road to recovery becomes much longer.
Prognosis
The prognosis for improvement with conservative treatment is excellent if there is no functional instability requiring surgery. Surgical repairs for acute dislocation and chronic tears are also good. Casting for an acute dislocation has a success rate of only 50%. Therefore, this option should be reserved for patients with contraindications to surgery.
A study reviewed the long-term clinical and patient-reported outcomes of a cohort of patients with peroneal tendon tears treated with debridement and primary repair. The study of 18 patients with an average follow-up of 6.5 years found excellent long-term functional outcomes for patients with tears of the peroneal tendons treated with debridement and primary operative repair. The study also observed that the majority of patients returned to their previous level of activity without the need for reoperation or revision of the repair. [24]
Complications
Complications of conservative treatment of a peroneal tendon injury are progression of pain and instability, and possible peroneal tendon rupture. Surgical complications vary depending on the procedure. A few common ones include sural nerve injury, progression of symptoms, chronic lateral ankle pain, and loss of range of motion. Any surgery poses a risk of infection and failure of the intent of the procedure.
-
Lateral ankle anatomy demonstrates the peroneal tendons as they course beneath the superior retinaculum. The anterior talofibular, calcaneofibular, and posterior talofibular ligaments are also shown.
-
Anterior drawer test, which assesses anterior talofibular ligament stability. The top hand stabilizes, while the lower hand translates the calcaneus and talus directly toward the operator. From Karageanes SJ. Principles of Manual Sports Medicine, Lippincott Williams & Wilkins, 2005.
-
Tilt test. The operator tilts the talus and calcaneus, not the forefoot. This assesses the integrity of the calcaneofibular ligament. From Karageanes SJ. Principles of Manual Sports Medicine, Lippincott Williams & Wilkins, 2005.
-
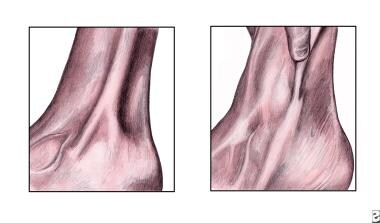
Dislocated peroneal tendons. Left, Note the course of the tendons anterior to the lateral malleolus. Right, Image demonstrates manual relocation of the displaced tendons.
-
Peroneal stability test. The patient pushes the foot laterally against resistance, while the operator monitors the tendon. From Karageanes SJ. Principles of Manual Sports Medicine, Lippincott Williams & Wilkins, 2005.