Practice Essentials
Participation in athletic activities has been shown to improve physical, mental, and emotional well-being. [1] As we age, it is important to maintain an active lifestyle, whether it is through weekend sports, resistance training, or highly competitive senior events. (Prior to starting an exercise program, it is important for patients to discuss with their physician an appropriate plan based on their medical history.)
Degeneration of the lumbar disc, associated degenerative facet arthritis, and spinal stenosis are the most common causes of low back and leg pain in the aging population, and the mature athlete is not immune from these processes.
Back pain has been associated with higher costs of treatment, cessation of training/competition, decreased quality of life, and limitations to performance. [2]
The images below depict degenerative lumbar disc disease.
 Degenerative lumbar disc disease in the mature athlete. Degenerative changes of the lumbar spine, including decreased signal intensity and disc bulging at the L-3/4, L-4/5 and L-5/S-1 discs.
Degenerative lumbar disc disease in the mature athlete. Degenerative changes of the lumbar spine, including decreased signal intensity and disc bulging at the L-3/4, L-4/5 and L-5/S-1 discs.
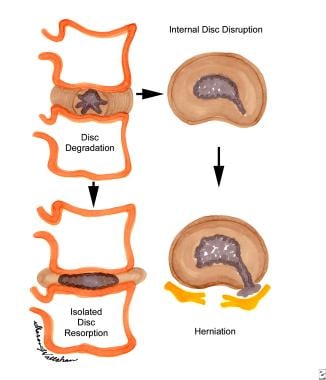 Degenerative lumbar disc disease in the mature athlete. The process of disc degeneration following internal disc disruption and herniation.
Degenerative lumbar disc disease in the mature athlete. The process of disc degeneration following internal disc disruption and herniation.
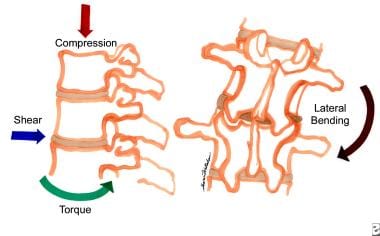 Degenerative lumbar disc disease in the mature athlete. The various forces placed upon the discs of the lumbarspine that can result in degenerative changes.
Degenerative lumbar disc disease in the mature athlete. The various forces placed upon the discs of the lumbarspine that can result in degenerative changes.
Many mature athletes (typically aged 40 years or older) present with complaints of low back pain (LBP), radicular symptoms, neurogenic claudication, or a combination of all of these symptoms. These clinical syndromes in the mature athlete should be fully evaluated, accurately diagnosed, and appropriately treated ensure safe return to play as well as screening for potential underlying systemic pathology.
Epidemiology
United States statistics
Low back pain has an incidence of 5-10% per year and a prevalence of up to 85% in the general population. Epidemiological studies have found that the frequency of LBP increases as age increases to 60 years; in those older than 60 years, the frequency declines with increasing age.
Disc degeneration has been found in at least one lumbar level in 35% of patients aged 20-39 years and all patients aged 60-80 years. [3]
Certain groups of athletes, including weightlifters and soccer players, appear to have a higher incidence of disc space narrowing and spondylolisthesis, but this does not correlate to a greater incidence of back pain compared with the general population. It is important to remember that low back pain is a symptom and not a diagnosis. [2]
Etiology
Deterioration of the spinal structures is a universal phenomenon with progression of age, occurring in both athletic and nonathletic populations. The intervertebral disc is part of a 3-joint complex; therefore, damage at the level of either the zygapophyseal joints or the disc affects the function of the entire unit.
The deteriorative process most likely begins with the intervertebral disc. Tiny blood vessels enter and exit the disc in the early decades of life, but these vessels become obliterated, leaving the intervertebral disc an avascular structure. Thereafter, nutrition of the disc is supported only through extracellular fluid osmosis. Water is drawn into the disc, and, with motion, the water is partially expelled. This constant movement of water into and out of the disc is thought to allow the disc to remain healthy by bringing in needed nutrients. With the aging process, there is a loss of some of the connective tissue fibers within the disc and an alteration in the properties of the nucleus pulposus. This causes less water to be drawn into the disc and, ultimately, may lead to impairment of nutrition. The water content of a disc in young persons is roughly 88%, but it is reduced to less than 70% in elderly persons.
The deterioration process leads to a stiffening of the intervertebral disc and a change in its shape, causing the disc to lose its ability to distribute load uniformly.
The fibers of the annulus run in different directions at different depths and allow the annulus to accommodate complex motions. Axial rotation of the spine or rotation of a flexed spine may isolate some of the annular fibers and cause small annular tears. These annular tears may or may not be symptomatic; however, in time, they may coalesce to weaken the annulus fibrosus. This can lead to disc bulging, disc space narrowing, or even frank herniation.
In addition, the loss of disc space height may lead to segmental instability and increased forces on zygapophyseal joints, resulting in sclerosis and hypertrophy. The loss of disc height also causes bulging of the annulus into the spinal canal and buckling of the ligamentum flavum. Ultimately, this degenerative cascade can lead to a narrowing of the spinal canal and intervertebral foramen, producing an acquired spinal stenosis.
These degenerative changes begin as early as the second to third decade of life and progress with advancing age. The clinical consequences of this deterioration vary with the age of the patient.
In persons aged 30-50 years, degenerative changes and tears in the annulus of the disc may cause frank herniation of the disc material. This population usually has some compromise of the integrity of the disc, yet the nucleus is still pliable enough to be extrudable, and the spine is mobile enough to produce the required forces for herniation.
With aging of the spine, the nucleus pulposus becomes firmer, spinal motion lessens, and bony overgrowth increases. The intervertebral discs do not herniate as frequently, and spinal stenosis becomes the prominent clinical picture.
Athletes and nonathletes alike are subject to these progressive degenerative changes. However, it is not completely clear how the potentially beneficial effects of training interact with the potentially harmful effects of loading experienced by athletes. The greatest incidence of discogenic disease would be expected to be found in those athletes participating in sports with the greatest axial stresses.
Hellstrom et al found that disc height reduction was much more common in athletes than nonathletes, and, specifically, it is most prevalent in wrestlers and male gymnasts. Horne et al found a high frequency of disc space narrowing in the thoracolumbar spines of water-ski jumpers.
Other studies have failed to show a correlation between physical loading and increased spinal pathology or low back symptoms, and some evidence suggests that certain types of loading may slow down the degenerative process.
Videman et al reported that former elite athletes overall reported less back pain than control groups in later adulthood. However, they did find an increase in the degenerative changes throughout the entire spine in former weight lifters and in the lower lumbar levels in soccer players when compared to controls. Despite these increased degenerative findings, the former weight lifters and soccer players still had less reported back pain than those in the control groups. This study and others provide some evidence that certain forceful athletic activities may accelerate the degenerative process, but that the degenerative changes seen on imaging studies do not correlate well with clinical symptoms. [4]
Functional Anatomy
The spine is composed of a series of spinal functional units, wherein each unit consists of 3 joints with an anterior and posterior segment. The anterior segment consists of 2 adjacent vertebral bodies and the intervertebral disc between them. The posterior segment consists of the laminae and their processes. One joint is formed between the 2 vertebral bodies, while the other 2 joints are formed by the articulation of the superior articular processes of 1 vertebra with the inferior articular processes of the vertebra above. The intervertebral disc consists of an inner core of gelatinous material called the nucleus pulposus. The nucleus pulposus is enclosed by a ring called the annulus fibrosus.
The individual lumbar nerve roots exit laterally through the intervertebral foramen located on each side of the spinal functional unit. Each intervertebral foramen is bound anteriorly by the vertebral column and intervertebral disc. The intervertebral foramen is bound superiorly and inferiorly by a pedicle, while posteriorly it is bound by the vertebral lamina and zygapophyseal joint. The outer one third of the intervertebral disc is an innervated structure, while the remainder of the disc, including the nucleus pulposus, lacks any innervation.
The sinuvertebral nerves are recurrent branches of the ventral rami that reenter the intervertebral foramina to be distributed within the vertebral canal. These nerves are mixed nerves, formed by a somatic root from a ventral ramus and an autonomic root from a gray ramus communicans. The sinuvertebral nerve supplies the posterior margin of the annulus fibrosus, anterior dura mater, dural sleeve, posterior vertebral periosteum, and the posterior longitudinal ligament. The anterior longitudinal ligament and the lateral aspect of the annulus fibrosus are both innervated by ventral rami and gray ramus communicans. The posterior rami of the spinal nerves supply zygapophyseal joints above and below the nerve, as well as the paraspinous muscles at multiple levels.
The spinal motions that frequently are encountered in many sports and other activities include axial compression/distraction, flexion and extension, torsion (rotational forces), and lateral flexion. Additionally, certain sports can subject the spine to tensile stress; shear forces in the anterior and posterior position, as well as to compressive forces in the craniocaudal direction. Protection of the functional units of the spine requires unrestricted and efficient motions between adjacent vertebral segments. Simple flexion/extension movements and even moderate axial compression forces are relatively well tolerated by the disc and the associated joint complexes of the spine.
Rotational forces and combined motions, such as forward flexion with rotation, have been shown to be the most injurious to the disc. Therefore, it is crucial that the supporting stabilizers of the spine, both static and dynamic, are sufficiently strong to offset some of these potentially injurious forces.
The static stabilizers of the lumbar spine include the longitudinal ligaments, the intervertebral discs between the vertebral bodies, and the zygapophyseal joint capsules connecting the posterior elements of the spine. The dynamic stabilizers comprise not only the musculature surrounding the lumbar spine, but also include the abdominal and hip muscles, including the hip flexors, extensors, and abductors.
The relationship of the pelvis to the spine is an important consideration when assessing problems in the lumbar spine. Increased lumbar lordosis may result from anterior pelvic tilt, resulting from weak abdominals and/or tight hip flexors. Decreased lumbar lordosis may result from posterior pelvic tilt, resulting from weak paraspinal extensor muscles and/or tight hamstring muscles. The dynamic stabilizers of the spine, when acting synergistically, can directly or indirectly reduce the shear forces to the intervertebral disc and to the zygapophyseal joints of the spine. Of note, in a study of elite athletes and nonathletes with low back pain, the amount of deconditioning of the lumbar extensor muscles was similar. In addition, similar strategies were employed to address spine stability and protection from pain and damage. [5]
Sport Specific Biomechanics
Sports injuries often involve a twisting or torsion movement, whereas falls are rarely a precipitating cause.
The most common area of complaint among male golfers of the Professional Golfer's Association is the lower back, with an estimated 10-33% of touring professionals reportedly playing with back complaints of some degree. Amateur golfers also identified LBP as their most common golf-related injury. The golf swing frequently has been implicated as a major source of injury to the spine in both professional and amateur golfers. Discogenic LBP most likely develops because of the axial rotation of the lumbar spine at the top of the backswing, with the subsequent uncoiling and hyperextension through the downswing and follow-through.
Several forces act on the lumbar spine during the golf swing. Rotational forces are developed as a result of twisting of the vertebral segments about the spine. Additionally, the spine is subjected to shear forces in the anteroposterior direction, axial compressive forces, and lateral bending forces.
Hosea and Gatt analyzed the various forces on the spine in the swings of amateur and professional golfers. [6] They determined that these forces were actually greater in amateur players compared to professional players. The amateur golfers generated greater lateral bending, anteroposterior shear, and rotational forces, with equal axial compression noted in the 2 groups. They determined that the loads required to cause disc disruption in cadaveric studies were similar to the loads that occur in the golf swing. The importance of trying to minimize forces on the spine through proper swing mechanics becomes clear. Additionally, strengthening the dynamic stabilizers of the spine to counteract the significant forces exerted on the spine during the golf swing is important in both the prevention and treatment of golf-related low back injuries.
Bartolozzi et al showed that players with improper technique had more radiographic evidence of lumbar degenerative disease than those with proper technique (62% vs 21%); however, the rate of LBP was not similar. [7]
-
Degenerative lumbar disc disease in the mature athlete. Degenerative changes of the lumbar spine, including decreased signal intensity and disc bulging at the L-3/4, L-4/5 and L-5/S-1 discs.
-
Degenerative lumbar disc disease in the mature athlete. The process of disc degeneration following internal disc disruption and herniation.
-
Degenerative lumbar disc disease in the mature athlete. The various forces placed upon the discs of the lumbarspine that can result in degenerative changes.






