Practice Essentials
Before the use of shoulder arthroscopy and magnetic resonance imaging (MRI) in the diagnosis and management of shoulder problems, glenoid labrum lesions were underappreciated. More specifically, superior labrum lesions about the insertion of the long biceps tendon were typically noted or managed using standard open surgical techniques. An improved understanding of the surgical anatomy and the biomechanical contributions of the superior labrum have demonstrated its significance in shoulder stability and its role in the pathogenesis of shoulder pain.
Andrews et al published a study that examined glenoid labrum lesions related to the long head of the biceps (LHB) in 73 throwing athletes. [1] The authors observed that the LHB was contiguous with the superior labrum and that most of these patients had avulsed the anterosuperior labrum off the glenoid in conjunction with the biceps tendon. Subsequently, Snyder et al defined the pattern of superior labral injury in 27 patients who were described as having superior labrum anterior posterior (SLAP) lesions. [2] The authors described the SLAP lesion as a labral detachment originating posterior to the long biceps insertion and extending anteriorly. These lesions were subsequently categorized as types I-IV, as follows:
SLAP classification
Types I-IV are as follows:
-
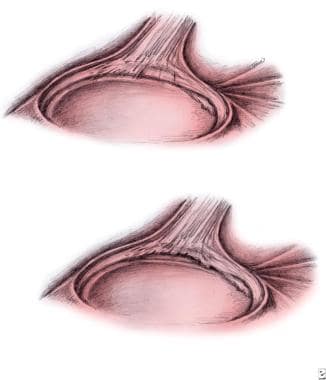
Type I: The glenoid labrum demonstrates degenerative changes and fraying at the edges but remains firmly attached to the glenoid rim. No avulsion of the biceps tendon is present (see the image below, upper left).
-
Type II: Degenerative changes and fraying are present in type II lesions. The glenoid labrum is detached completely from the anterosuperior to the posterosuperior glenoid rim. This portion of the labrum is lifted by the long biceps tendon, and the attachment of the biceps tendon is unstable (see the image below, lower right).
-
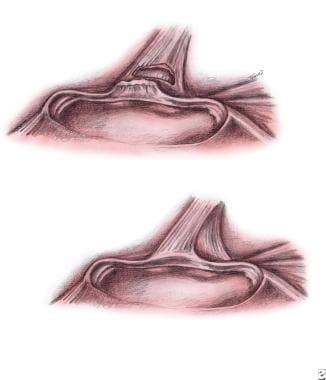
Type III: With type III lesions, the free margin of the superior labrum is displaced into the joint (bucket handle), whereas the labral attachment to the glenoid rim and biceps tendon remains intact. The insertion of the biceps tendon is not unstable (see the image below, upper left).
-
Type IV: The superior portion of the labrum is displaced into the joint (bucket handle) in type IV lesions. In contrast to type III tears, the long biceps tendon is also affected, involving partial rupture in the direction of the fibers (see the image below, lower right).
Superior labral pathology is now recognized as a potential sources of considerable pain and disability in active patients. The goal of this article is to familiarize the reader with the anatomy, pathophysiology, diagnosis, and management of labral tears of the superior glenoid.
For patient education materials, see the Hand, Wrist, Elbow, and Shoulder Center, as well as Rotator Cuff Injury and Shoulder Separation.
Related Medscape Reference topics:
Multidirectional Glenohumeral Instability
Posterior Glenohumeral Instability
Superior Labral Lesions [in the Orthopedic Surgery section]
Epidemiology
United States statistics
Snyder et al reported the result of over 140 patients who were treated operatively for superior labral lesions. [3] The authors noted a 6% incidence of SLAP lesions in persons undergoing shoulder arthroscopy for all diagnoses over an 8-year period. The percentages of the types of SLAP lesions encountered were as follows: type I, 21%; type II, 55%; type III, 9%; type IV, 10%; and complex lesions, 5%. Associated lesions included Bankart lesions (22%) and lesions of the rotator cuff (11%). Only 28% of SLAP lesions were found without associated pathology.
Kim et al reported that of 544 shoulder arthroscopy procedures, 139 (26%) demonstrated a SLAP lesion. [4] Of the SLAP lesions, 103 (74%) were type I, 29 (21%) were type II, 1 (0.7%) was type III, and 6 (4%) were type IV. Most (123) of the SLAP lesions were found to be associated with other intra-articular lesions.
A study by Gaudelli et al reported that a type IV SLAP lesion can be expected in 22% of patients with recurrent shoulder instability. [5]
Kampa and Clasper evaluated the presentation and incidence of SLAP lesions in military and civilian populations. [6] Of 178 patients who underwent arthroscopy for complaints of either pain, instability, or pain and instability, 39 (22%) SLAP lesions were found. According to the Snyder classification (see Introduction, SLAP classification), 20.5% were type I, 69.3% were type II, 5.1% were type III, and 5.1% were type IV. The authors found that patients with a history of trauma or symptoms of instability were more likely to have a SLAP lesion than patients presenting with atraumatic etiologies. Military patients also had a higher incidence of these lesions relative to civilian patients. [7]
Collectively, these data suggest that patients who suffer traumatic injuries of the shoulder are at increased risk for sustaining an injury to the superior labrum, and that the severity of the resulting lesion is variable. Traumatic SLAP lesions are often associated with other intra-articular shoulder injuries, and the examining physician must have a high index of suspicion for coexisting pathology.
Functional Anatomy
Grossly, the glenoid labrum surrounds the entire circumference of the glenoid surface. Moseley and Overgaard [8] in 1962 and Detrisac and Johnson [9] in 1986 described the labrum as a redundant fold of capsular (fibrous) tissue. Superiorly, the labrum is contiguous with the tendon insertion of the LHB as it attaches to the supraglenoid tubercle. The anterior labrum fibers may insert into the middle glenohumeral ligament (joint capsule). The superior labrum is more meniscuslike in structure because its fibers are loosely attached to the glenoid rim and may overlap the superior glenoid surface, whereas the inferior labrum is attached more tightly to the glenoid rim and is typically round in appearance.
The entire labral complex is attached at all points to either the bony glenoid rim or joint capsule about the glenoid, except in the anterosuperior margin. A sublabral foramen is present in most individuals; this labral foramen may be confused on MRI or at arthroscopy with a labral tear.
The Buford complex represents another anatomic variant and is described as a cordlike thickening of the middle glenohumeral ligament and absence of the anterosuperior labrum. This anatomic finding must be recognized as a normal variant because attempts to repair or debride this region may result in abnormal capsular constraint, shoulder stiffness, or glenohumeral instability. Interestingly, a retrospective review suggested that the presence of a Buford complex may correlate with the presence of a SLAP lesion in patients. [10]
Histology
Cooper et al examined the anatomy and histology of the glenoid labrum. [11] The authors noted an existing fibrocartilaginous transition zone at the superior glenoid margin between the fibrocartilaginous labrum and the hyaline cartilage of the glenoid surface. This study also confirmed the gross observation that the superior labrum fibers insert directly into the fibers of the LHB, distal to the biceps insertion into the supraglenoid tubercle. Histologic examination also revealed that the labrum consists of densely packed collagen bundles and fibrochondrocytes.
The primary labrum vascular supply originates from the suprascapular, circumflex scapular, and posterior humeral circumflex arteries. Only the periphery of the labrum appears to be vascularized, and no contribution to the labral blood supply is derived from the underlying bone. Prodromos et al observed that fetal and newborn shoulders possess an extensive blood supply throughout the labrum, whereas adult specimens have only sparse peripheral vasculature. [12] Apparently, labral vascularity, much like the meniscus, recedes with advanced age.
As previously mentioned, the LHB brachii muscle is also anatomically important in the discussion of SLAP lesions (see Introduction, Background). This LHB tendon arises from the supraglenoid tubercle, and fibers from the superior labrum attach to the biceps tendon in this region. Following the examination of over 100 cadaver specimens, Vangsness et al estimated that approximately 50% of the biceps tendon originates from the superior labrum. [13] The most common labral origin of the biceps is the posterior-superior region.
Sport-Specific Biomechanics
Long before the advent of shoulder arthroscopy, labral tears were described in association with anterior shoulder subluxation and dislocation, suggesting a role for the labrum in glenohumeral stability maintenance. McGlynn and Caspari described the intra-articular findings of subluxating shoulders noted at the time of arthroscopy. [14] As suggested by previous studies, fraying, tearing, or detachment of the glenoid labrum was a common finding in this group of 19 unstable shoulders.
In defining the relevant factors contributing to anterior shoulder stability, Turkel et al noted that the inferior glenohumeral ligament, which attaches to the glenoid via the labrum, is essential in preventing anterior shoulder instability. [15] The glenoid labrum increases the area and depth of the glenoid cavity, contributing to articular stability of the glenohumeral joint. The labrum has been suggested to act as a chock block to the humeral head as it attempts to translate anteriorly or posteriorly upon the glenoid surface.
Andrews et al demonstrated that superior labrum lesions were observed in a group of overhead throwing athletes who underwent arthroscopic examination of the shoulder. [1] On the basis of observed lesions in this group of athletes, the authors suggested that the biceps tendon is subjected to large forces during the act of throwing. Intraoperative stimulation of the biceps during arthroscopic shoulder surgery also revealed that the LHB tends to pull the labrum off the superior glenoid rim (especially in the presence of a SLAP lesion). Therefore, excessive forces generated by the biceps tendon during overhead throwing activities may lead to the generation of superior labral tears.
In a study from the University of Pittsburgh, Rodosky et al analyzed the role of the LHB and superior labrum in anterior shoulder instability. [16] A dynamic cadaveric shoulder model was used to simulate the forces of the late-cocking phase of the throwing motion. Strain gauges were placed in the inferior glenohumeral ligaments of 7 nonembalmed cadaver shoulders. Tests of anterior glenohumeral translation were made with and without the presence of superior labral lesions (analogous type II lesions). Varying forces were applied to the biceps tendon (0-100% extrapolated maximum force) in all tested specimens.
In normal shoulders (ie, no SLAP lesion), peak torque increased 22% and peak torsional rigidity increased 32% in shoulders with maximal biceps (loading versus unloaded shoulders). [16] In shoulders with a simulated SLAP lesion and no biceps loading, the observed peak torque was 12% lower than that of normal specimens, and a 120% increase in inferior glenohumeral ligament strain was observed. In shoulders with simulated SLAP lesions and 100% biceps loading, the observed peak torque was 7% lower than that of normal specimens. Torsional rigidity was also decreased by the creation of a SLAP lesion with and without biceps loading. In this study, torsional rigidity represented a measure of the tested shoulder to resist rotational forces.
In another study, Pagnani et al examined the effect of superior glenoid labrum lesions on glenohumeral translation. [17] In this cadaveric study, the investigators applied sequential anterior, posterior, superior, and inferior forces of 50 Newtons (N) to the proximal humerus. A 22-N compressive force was also applied. During the application of the described loads, a 55-N force was applied to the LHB tendon. The shoulders were tested in 7 positions of glenohumeral elevation and rotation. Each specimen was tested with a normal superior labral complex, a partial superior labral tear, and a complete tear (including the biceps insertion on the supraglenoid tubercle).
The authors found that a partial tear of the superior labrum had no significant effect upon superoinferior or anteroposterior translation [17] ; however, the creation of a complete SLAP lesion resulted in significant increases in anterior and inferior translation at all arm elevations. Increased glenohumeral translation persisted even after the application of a 55-N force to the biceps tendon. Pagnani et al suggested that the LHB tends to stabilize the joint by generating joint compressive forces and by acting as a physical restraint to translation.
These data suggest that in external rotation and abduction, the forces generated by the biceps muscle result in an increase in torsional rigidity. These findings suggest that increased loads applied to the biceps tendon may protect the shoulder from anterior subluxation during the throwing motion.
Related Medscape Reference topics:
Elbow and Forearm Overuse Injuries
Related Medscape topic:
Resource Center Exercise and Sports Medicine
Etiology
In a series, Snyder et al reported that a compressive force or traction injury to the affected extremity was the most common mechanism of injury. [2] However, in 21% of these patients, the etiology of the SLAP lesion was insidious. Moreover, most throwing athletes examined by Andrews et al did not report a distinct traumatic event. [1] Thus, although an isolated injury may cause a labral injury, SLAP lesions may also occur as a result of the repetitive microtrauma that is associated with the overhead throwing motion.
Numerous authors have described a peel-back method for the development of SLAP II lesions. When the shoulder is in an abducted and externally rotated position, the biceps tendon is thought to assume a more vertical and posteriorly directed posture, which transmits a force to the superior labrum and causes it to peel off of the glenoid. Grossman et al supported this hypothesis in a cadaveric model. [18] A contracted posterior capsule and resulting internal rotation deficiency, which is commonly observed in overhead throwing athletes, may translate the humeral head anteriorly, further aggravating the patient's symptoms.
Related Medscape Reference topics:
-
Upper left - Type I superior labrum anterior posterior lesion. Lower right - Type II superior labrum anterior posterior lesion.
-
Upper left - Type III superior labrum anterior posterior lesion. Lower left - Type IV superior labrum anterior posterior lesion.
-
Coronal magnetic resonance arthrogram. This image demonstrates detachment of the superior glenoid labrum.
-
Arthroscopic appearance of a type II superior labrum anterior posterior (SLAP) lesion.
-
Arthroscopic placement of a suture anchor in the superior glenoid.
-
Arthroscopic suture placement for superior labrum anterior posterior (SLAP) lesion repair.
-
Arthroscopic appearance of a superior labrum anterior posterior (SLAP) lesion after repair with a suture anchor.
-
Simple mattress suture configuration with a single anchor. (Arthroscopy. 2007 Feb;23(2):135-40.)