Practice Essentials
Athletic foot injuries can be difficult to properly diagnose and treat. Bearing the weight of the entire body, the foot is under tremendous stress. In many sports, the foot absorbs tremendous shearing and loading forces, sometimes reaching over 20 times the person's body weight. Physicians who treat these disorders must have a good understanding of the anatomy and kinesiology of the foot.
See the following images.
Although foot injuries can occur from a variety of causes, the most common cause is trauma. Other etiologies include (1) rapid or improper warm-up, (2) overuse, (3) intense workouts, (4) improper footwear, and (5) playing on hard surfaces. [1, 2, 3, 4, 5, 6]
Physicians who evaluate and treat common foot problems should have a working knowledge of the individual sports and the injuries that are commonly associated with them. An understanding of the basic treatment approaches for these injuries also is imperative.
Etiology
Sesamoiditis is usually caused by overuse of the foot in a plantar flexed position. Cleats with little insole padding can focus excess stress on the first MTP or sesamoid and thus can trigger this condition. A depressed first ray, forefoot valgus, or pes cavus deformity can lead to sesamoiditis as well.
Turf toe is caused by hyperextension of the first MTP joint beyond the normal 60° of dorsiflexion. The incidence of the injury has increased with the widespread use of artificial surfaces. Lightweight, poorly supported, flexible shoes can predispose the athlete to injury.
Sever disease is caused by excessive traction on the calcaneal apophysis by the Achilles tendon, particularly during running and jumping. Inflexibility of the gastrocnemius, hamstring, quadriceps, and hip flexor muscles can exacerbate this condition.
Posterior tibial tendinitis is caused by repetitive trauma during the pronation phase of cutting, jumping, or running. Pes planus is a risk factor.
Peroneal tendon subluxation/dislocation most commonly occurs with powerful contraction of the peroneal muscles, usually in maximal dorsiflexion. The peroneal tendons are retained in place by the superior and inferior peroneal retinaculum. If enough stress is applied, these may rupture, resulting in subluxation or dislocation of the peroneal tendons.
Peroneal tendinitis may be related to acute inversion injury or chronic overuse secondary to hindfoot varus. Iliotibial band restriction increases force on the peroneal tendons.
FHL tenosynovitis is typically associated with repeated push-off maneuvers, such as those executed by ballet dancers or sprinters.
A Jones fracture usually occurs when a load is applied to the lateral forefoot in the absence of inversion. A Jones fracture can also occur with an acute inversion injury. Jones injuries usually occur in sports involving running and jumping. Fifth metatarsal proximal diaphyseal fractures can occur with chronic overuse and poor biomechanics. Fifth metatarsal base avulsion fractures commonly occur via inversion sprain mechanisms.
Morton (intermetatarsal) neuroma is a biomechanically induced neuropathy of the common digital nerve of the foot. Repetitive microdamage to the nerve fibers produces degeneration and reparative fibrosis, significantly increasing the nerve diameter. Restrictive toe boxes combined with overuse can cause this condition.
Stress fractures
Stress fractures are defined as spontaneous fractures of normal bone that result from the summation of stresses, any of which by themselves would be harmless. [6, 7, 8, 9, 10] Stress fractures of the foot were first described by Breihaupt in 1855. Serving as a physician in the Prussian army, Breihaupt observed fractures of the metatarsals in otherwise healthy military recruits after long marches. These became know as march fractures.
Of all sports-related injuries, it is estimated that 5-10% involve stress fractures. Nine of the 24 members of the 1994 United States National World Cup Soccer Team were diagnosed with stress fractures. The incidence of stress fractures is increasing for the following reasons: (1) increasing numbers of persons participating in sporting activities, (2) increasing awareness and suspicion of stress fractures, and (3) change in the nature and type of sporting activities (ie, rollerblading). Stress fractures of the second, third, and fourth metatarsals account for 90% of metatarsal injuries
Lisfranc fracture dislocation
The transverse ligaments connect the second, third, fourth, and fifth metatarsal bases. The second metatarsal is recessed and bound to the medial and intermediate cuneiform bones by ligaments. The Lisfranc ligament joins the first (medial) cuneiform bone to the base of the second metatarsal. The base of the second metatarsal, recessed tightly into the mortise formed by the cuneiform bones and attached by multiple ligaments, forms the keystone of the midfoot and, thus, is the primary stabilizing structure of the TMT joint complex.
Lisfranc fracture dislocations are classified as homolateral or divergent. A homolateral dislocation involves displacement of 4 or 5 metatarsals in the same direction. A divergent dislocation involves a split between the first and second metatarsals.
Epidemiology
United States statistics
Estimates indicate that 15% of sports-related injuries affect the foot alone.
A study that evaluated rates of severe foot injuries (season- or career-ending injuries, injuries with >30-day time loss, or injuries requiring operative treatment) in US collegiate athletes found that 18.7% of all foot injuries that occurred during a 10-year period were severe. Men’s sports with the highest rates of severe foot injuries were basketball, indoor track, and football, whereas women’s sports with the highest rates were cross-country, gymnastics, and outdoor track. [11]
International statistics
Among professional ballet dancers, the most frequent sites of injury are the foot and ankle, which account for up to 62% of all injuries. [12]
Functional Anatomy
Foot and ankle
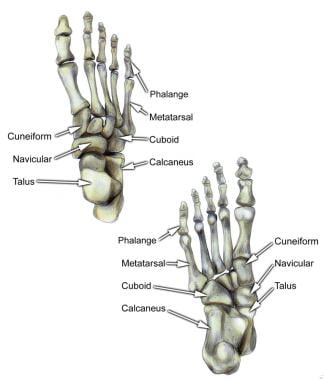
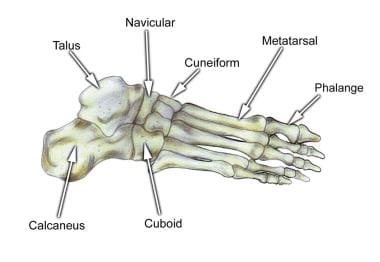
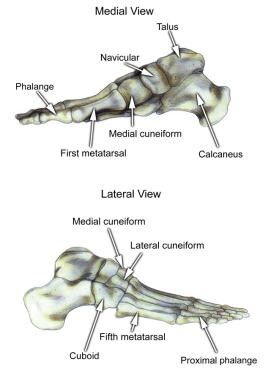
The foot is composed of 26 major bones, which can be divided into 3 regions: the forefoot, midfoot, and hindfoot. The forefoot is comprised of the 5 metatarsals and the 14 phalanges. The 3 cuneiforms (ie, lateral, intermediate, medial), the cuboid, and the navicular represent the midfoot. The hindfoot is composed of the talus and the calcaneus (see image below).
The talus is oriented to transmit forces from the foot through the ankle to the leg.
The calcaneus is the largest bone in the foot. The Achilles tendon inserts on the posterior aspect of the calcaneus.
The navicular lies anterior to the talus and medial to the cuboid.
The cuboid articulates with the calcaneus proximally, with the fourth and fifth metatarsals distally, and with the lateral cuneiform medially (see image below).
Each of the cuneiform bones is wedge-shaped. The medial, intermediate, and lateral cuneiform bones articulate with the first 3 metatarsals distally and the navicular proximally. The cuboid articulates with the lateral cuneiform.
The 5 metatarsals articulate with the proximal phalanges.
The great toe is composed of 2 phalanges, with 3 for each lesser toe.
Although variation exists in the number and location of the sesamoid bones, 2 constant sesamoids are present beneath the metatarsal head. The sesamoids are usually present within tendons juxtaposed to articulations.
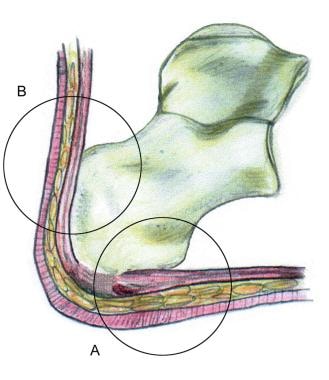
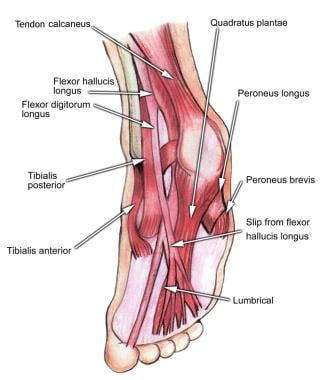
Select tendons of the foot (see image below)
The flexor hallucis longus (FHL) tendon is 1 of 3 structures that lie in the tarsal tunnel. Running behind the medial malleolus, the FHL is the most posterolateral. The FHL runs anterior to insert onto the distal phalanx of the great toe. The FHL acts as a flexor of the great toe, elevates the arch, and assists with plantar flexion of the ankle.
The flexor digitorum longus (FDL) tendon passes between the FHL and tibialis posterior tendon. The FDL inserts onto the distal phalanges of the 4 lateral digits and acts to flex the distal phalanges.
The tibialis posterior tendon is the most anteromedial of the tarsal tunnel tendons. This tendon inserts on the navicular tuberosity; the 3 cuneiforms; the cuboid; and the second, third, and fourth metatarsals. The tibialis posterior muscle flexes, inverts, and adducts the foot.
Laterally, the peroneus longus and peroneus brevis tendons share the common peroneal tunnel running behind and around the lateral malleolus. The peroneus longus plantar flexes the first metatarsal, flexes the ankle, and abducts the foot. The peroneus brevis flexes the ankle and everts the foot.
Other important structures
The plantar aponeurosis or fascia is a deep span of connective tissue extending from the anteromedial tubercle of the calcaneus to the proximal phalanges of each of the toes. Medial and lateral fibrous septa originate from the medial and lateral borders to attach to the first and fifth metatarsal bones.
Nerve innervation of the foot runs along the medial and lateral metatarsals and phalanges in a neurovascular bundle. These nerves are vulnerable to compressive forces that, in time, can generate the painful Morton neuroma, which most commonly affects the interspace between the third and fourth metatarsals. Four nerves supply the forefoot: the sural nerve (most lateral), branches of the superficial peroneal nerve, the deep peroneal nerve, and the saphenous nerve.
The joint between the forefoot and the midfoot, the tarsometatarsal (TMT) joint or Lisfranc joint, is formed by a mortise of the cuneiform bones surrounding the base of the second metatarsal. This joint is supported by the transverse ligaments, and the Lisfranc ligament joins the medial cuneiform and the base of the second metatarsal. Disruption of this ligament can result in a destabilization of the TMT joint complex of the foot, the result of which can be instability of the arch and the midfoot.
Sport-Specific Biomechanics
The 3 planes in which the foot and ankle function are the transverse, sagittal, and frontal. Movement is possible in all 3 planes.
-
Plantar flexion and dorsiflexion occur in the sagittal plane. Plantar flexion involves the foot moving from the anterior leg distally. Dorsiflexion is the opposite motion.
-
Inversion and eversion occur in the frontal plane of motion. Eversion occurs when the bottom of the foot turns away from the midline of the body. Inversion is the opposite action.
-
The 2 transverse plane motions are abduction and adduction. Adduction involves the foot moving toward the midline of the body, whereas abduction is the opposite action.
-
The hindfoot is composed of the talus and the calcaneus.
-
Select tendons of the foot.
-
Select bones of the foot (dorsal and plantar views).
-
Select bones of the foot (medial and lateral views).
-
Select bones of the foot (superolateral view).