Practice Essentials
Cervical radiculopathy is a dysfunction of a nerve root of the cervical spine. The seventh (C7; 60%) and sixth (C6; 25%) cervical nerve roots are the most commonly affected. [1, 2, 3, 4, 5, 6, 7] See the images below.
 Sagittal magnetic resonance image of the cervical spine. This image reveals a C6-C7 herniated nucleus pulposus.
Sagittal magnetic resonance image of the cervical spine. This image reveals a C6-C7 herniated nucleus pulposus.
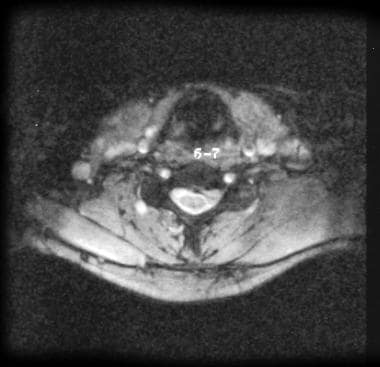 Axial magnetic resonance image of the cervical spine. This image reveals a C6-C7 herniated nucleus pulposus.
Axial magnetic resonance image of the cervical spine. This image reveals a C6-C7 herniated nucleus pulposus.
Signs and symptoms
The typical patient with cervical radiculopathy may present with motor, reflex, and/or sensory changes. [8] Sensory changes can include neck and arm discomfort, paresthesias, or numbness. The discomfort can range from a dull ache to a severe burning pain. Symptoms may be provoked by neck movements/positioning. Typically, patients tilt their head away from the side of injury and hold their neck stiffly. Active range of motion (ROM) is usually reduced.
Specifically in younger athletes, an acute traumatic event rather than insidious onset was linked to the onset of radicular symptoms. When a single traumatic event is present in the mechanism of injury, a cervical disc herniation is usually the underlying cause. [9]
See Presentation for more detail.
Diagnosis
Imaging studies
Radiography of the cervical spine is usually the first diagnostic test ordered in patients who present with neck and limb symptoms, and more often than not, this study is diagnostic of cervical disc disease as the cause of the radiculopathy.
CT scanning provides good visualization of bony elements and can be helpful in the assessment of acute fractures.
MRI has become the method of choice for imaging the neck to detect significant soft-tissue pathology, such as disc herniation.
Other tests
Electrodiagnostic studies are important in identifying physiologic abnormalities of the nerve root and in ruling out other neurologic causes for the athlete's complaints.
See Workup for more detail.
Management
Initial treatment should be directed at reducing pain and inflammation. Once pain and inflammation are controlled, the patient's therapy should be progressed to the restoration of full ROM and flexibility of the neck and shoulder girdle muscles.
Cervical epidural steroids have been used in patients whose conditions have not had satisfactory responses to medications, traction, and a well-designed physical therapy program.
Patients whose condition fails to improve with a comprehensive rehabilitation program and selective injections should be offered a surgical evaluation.
See Treatment and Medication for more detail.
Background
In the younger population, cervical radiculopathy is a result of a disc herniation or an acute injury causing foraminal impingement of an exiting nerve. [10] Disc herniation accounts for 20-25% of all cases of cervical radiculopathy with a higher incidence when symptoms started after single traumatic event.
In the older patient, cervical radiculopathy is often a result of foraminal narrowing from osteophyte formation, decreased disc height, or degenerative changes of the uncovertebral joints anteriorly and of the facet joints posteriorly.
Factors associated with increased risk include heavy manual labor requiring the lifting of more than 25 pounds, smoking, and driving or operating vibrating equipment. Other, less frequent causes include tumors of the spine, an expanding cervical synovial cyst, synovial chondromatosis in the cervical facet joint, giant cell arteritis of the cervical radicular vessels, and spinal infections. [11, 12] The purpose of this article is to provide information on the presentation, evaluation, differential diagnosis, and treatment of cervical radiculopathy.
Etiology
Little is known about the natural history of cervical radiculopathy. The pathogenesis of radiculopathy involves an inflammatory process initiated by nerve root compression. Evidence exists that inflammatory mediators, including nitric oxide, prostaglandin E2, interleukin-6, and matrix metalloproteinases, are released by herniated intervertebral discs. [13, 14] This results in nerve root swelling. The compression may be from a disc herniation, degenerative changes about the neural foramen, or a combination of the two.
A study in patients with cervical disc disease found that compression of a nerve root produced limb pain, whereas pressure on the disc produced pain in the neck and medial border of the scapula. [15] Results from intradiscal injection and electrical stimulation of the disc have also suggested that neck pain is referred by a damaged outer annulus. [16, 17, 18, 19, 20, 21] Muscle spasms of the neck have also been found after electrical stimulation of the disc.
Epidemiology
United States statistics
Cervical radiculopathy occurs at a much lower frequency than radiculopathy of the lumbar spine. The annual incidence is approximately 85 cases per 100,000 population.
International statistics
A systematic review by Mansfield et al found that the prevalence of cervical spine radiculopathy was 1.14% among males and 1.31% among females. [22]
Functional Anatomy
Seven cervical vertebrae and 8 cervical nerve roots exist. The C1-2 (atlantoaxial) joint forms the upper cervical segment. [1, 3, 23, 24] This joint allows for 50% of all cervical rotation. The occipitoatlantal joint is responsible for 50% of flexion and extension. Below the C2-C3 level, lateral bending of the cervical spine is coupled with rotation in the same direction. This is due to the 45° inclination of the cervical facet joints.
The vertebral bodies of C3-C7 are similar in appearance and function. They articulate via the zygapophyseal or facet joints posteriorly. On the lateral aspect of the vertebral bodies are sharply defined margins, which articulate with the facet above. These articulations are called uncovertebral joints, or the joints of Luschka. These joints can develop osteophytic spurs, which can narrow the intervertebral foramina.
Intervertebral discs are located between the vertebral bodies of C2-C7. The discs are composed of an outer annular fibrosis and an inner nucleus pulposus and serve as force dissipators, transmitting compressive loads throughout a range of motion (ROM). The intervertebral discs are thicker anteriorly and therefore contribute to normal cervical lordosis.
The foramina are largest at C2-C3 and progressively decrease in size to the C6-C7 level. The nerve root occupies 25-33% of the foraminal space. The neural foramen is bordered anteromedially by the uncovertebral joints, posterolaterally by facet joints, superiorly by the pedicle of the vertebra above, and inferiorly by the pedicle of the lower vertebra. Medially, the foramina are formed by the edge of the end plates and the intervertebral discs. The nerve roots exit above their correspondingly numbered vertebral body from C2-C7. C1 exits between the occiput and atlas, and C8 exits below the C7 vertebral body. Degenerative changes of the structures that form the foramina can cause nerve root compression. This compression can occur from osteophyte formation, disc herniation, or a combination of both.
Sport-Specific Biomechanics
Cervical radiculopathy in athletes can occur from several mechanisms. These injuries can occur from an extension, lateral bending, or rotation mechanism, which closes the neural foramen and results in ipsilateral nerve root injury. Conversely, a traction injury can occur with a sudden flexion or extension, coupled with lateral bending away from the affected nerve root.
Additionally, cervical disc herniations can occur with a sudden load with the neck in either flexion or extension. In a study of professional football players, a single traumatic event leading to herniation of a cervical disc was the cause of radiculopathy in around 50% of cases. [9]
In elderly persons with osteophyte formation, repetitive neck extension and rotation in certain sports, such as swimming or tennis, may result in a more insidious injury.
Prognosis
The prognosis for patients with cervical radiculopathy is excellent, with proper treatment. Nonoperative treatment is effective in 80-90% of patients. Surgery is indicated when nonoperative treatment has failed. The time frame for this decision depends on the ability of the patient to progress through the various phases of rehabilitation (see Treatment, Acute Phase, Recovery Phase, and Maintenance Phase).
Complications
Complications include incomplete neurologic recovery, loss of full cervical ROM, and radiographic changes that indicate disc-space narrowing, persistent loss of normal cervical lordosis, and/or osteophyte formation.
Patient Education
Proper sport technique is usually of great importance in the prevention and rehabilitation of many cervical radiculopathies. This includes the following:
-
A proper ball toss in tennis
-
A proper body turn in swimming
-
Proper head positioning when tackling in football
-
Sagittal magnetic resonance image of the cervical spine. This image reveals a C6-C7 herniated nucleus pulposus.
-
Axial magnetic resonance image of the cervical spine. This image reveals a C6-C7 herniated nucleus pulposus.



