Practice Essentials
Cervical intervertebral disc disease accounts for 36% of all spinal intervertebral disc disease, second only to lumbar disc disease, which accounts for 62% of all spinal intervertebral disc disease. (See the image below.) Cervical problems tend to be less debilitating than lumbar problems, and they do not cause individuals to miss work as often as lumbar spine problems do. [1, 2]
One of 5 visits to an orthopedic practice is for cervical discogenic pain (CDP), with C5-6 and C6-7 accounting for approximately 75% of visits. C7 is the most common nerve root involved. [3, 4] Cervical discogenic pain syndrome (CDPS) presents with proximal symptoms first, and, later, it can progress to brachialgia.
Epidemiology
United States statistics
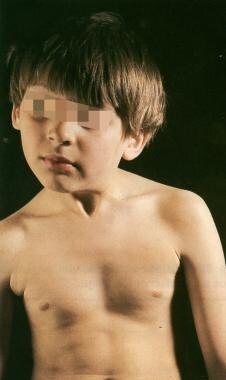
Cervical intervertebral disc disease accounts for 36% of all spinal intervertebral disc disease. This condition is somewhat more common in women. Although acute attacks may start at a very young age with episodes of acute torticollis or "wry neck," the incidence peaks when persons are aged 45-50 years (see image below).
Of all sports-related injuries, 2-3% are spinal injuries and the majority of these happened during unsupervised activities such as football, soccer, wrestling, diving, surfing, skiing and sandlot games. [5] The majority of the available literature, however, is found for football and this group is the most likely to sustain cervical trauma.
Statistical estimates of the incidence of cervical injury for football players varies ranging from 1 quadriplegic injury per 7,000 to 1 injury per 58,000. [6] Another review reported that since 1977, there has been an annual incidence of fewer than 10 cases of permanent injury to the cervical spinal cord among football players. [7] In 1976, the National Collegiate Athletic Association football rules committee disallowed the technique of spear tackling or the technique of using the helmet to butt or ram an opponent. This resulted in a remarkable decrease in the incidence of catastrophic neck injuries over the next 9 years. [8]
International statistics
A systematic review by Mansfield et al found that the prevalence of cervical spine radiculopathy was 1.14% among males and 1.31% among females. [9]
Functional Anatomy
The cervical spine permits a wide range of motion (ROM) of the head in relation to the trunk. A degree of stability and flexibility is required to control the motion and dissipate the forces applied to the spine. Great differences in anatomy and function exist between the occiput-C1, the C1-2 (upper complex), and C3-C7 (lower complex) levels. Eight motion segments occur between the occiput and T1. No disc exists between C1 and C2; therefore, the first intervertebral disc is between C2 and C3.
The intervertebral disc consists of an outer annulus fibrosus and an inner nucleus pulposus. The intervertebral disc is thicker anteriorly, contributing to the normal cervical lordosis. The C6-7 disc is the thickest disc of the cervical spine. The nucleus pulposus and the inner one half of the annulus fibrosus are avascular and receive nutrition through diffusion, compression, dehydration, and imbibition of fluids. [10]
The annulus fibrosus, particularly the outer one third, has been found to be innervated by the sinuvertebral nerve and the vertebral nerve. The sinuvertebral nerve arises from the ventral ramus (somatic root), whereas the vertebral nerve (autonomic root) is derived primarily from the sympathetic nervous system. However, the vertebral nerve has connections with the cervical ventral rami, which suggests the possibility of the vertebral nerve also conveying somatic afferents from the disc. [11, 12, 13]
The nociceptors and mechanoreceptors in the annulus fibrosus mediate pain transmission from structural disruption of the intervertebral disc itself or from the chemically mediated inflammatory effect of phospholipase A2. [12, 14] Pacinian corpuscles and Golgi tendon organs present in the posterolateral region of the outer one third of the annulus transmit proprioceptive information from the intervertebral disc. [10, 14, 15, 16, 17]
The adult cervical disc has a crescentic shape anteriorly, with the apex of the crescent at the uncovertebral joints on each side. The posterior annulus has multiple vertical fissures allowing for a very degenerative appearance during discography and on gross examination. In addition, the nucleus of the cervical disc tends to be poorly centralized when compared with the lumbar disc. In the lumbar disc, the nucleus tends to be well localized in the center of the disc, and the posterior annulus tends to remain relatively intact when compared with the cervical disc. Annular fissures in the lumbar disc tend to be circumferential and/or radial in nature.
Sport-Specific Biomechanics
Biomechanics is the study of the changes in the anatomic structures occurring during body movements. The movements of the cervical spine include flexion and extension in the sagittal plane, lateral flexion in the coronal plane, and rotation in the horizontal plane. Lateral flexion and rotation occur as coupled movements. Other movements of the cervical spine include protrusion (ie, the head is moved as far forward as possible with the neck outstretched and maintaining forward-facing position) and retraction (ie, the head is moved as far backward as possible and maintaining a forward-facing position).
Fifty percent of rotation of the cervical spine occurs in the upper cervical complex with the atlas rotating ipsilaterally around the odontoid. Protrusion causes upper cervical spine extension and lower cervical spine flexion, whereas retraction causes upper cervical spine flexion and lower cervical spine extension. At the occiput-C1 and C1-2 levels, ROM is greater with the protruded and retracted position than with full-length flexion and full-length extension positions. [18] See the image below.
The annular fibers are made up of collagenous lamellae with alternating directions of inclination oriented 35° from the horizontal. The annulus is more susceptible to injury with rotation and translation movements due to resistance offered only by the lamella oriented in the direction of movement. In the cervical spine, as in the lumbar spine, the intervertebral disc dissipates the transmission of compressive loads throughout the ROM by slowing the rate at which these forces are transmitted through the spine. By diverting the load via temporarily stretching the annular fibers, the disc protects the vertebra from taking the entire load at once.
In asymmetric loading, the nucleus pulposus migrates toward the area with less load. Thus, in flexion movements of the cervical spine, anterior offset loading of the intervertebral disc occurs, in which the nucleus pulposus moves posteriorly and the posterior annular wall is stretched. In addition, the cervical lordosis reduces, the vertebral canal lengthens, and the intervertebral foramina open. [2]
In extension movements of the cervical spine, posterior offset loading of the intervertebral disc occurs, in which the nucleus moves anteriorly and the anterior annular wall is stretched. Shortening of the vertebral canal and closing of the intervertebral foramen also occur. [2] In lateral flexion and rotation (coupling movement) of the cervical spine, there is offset loading of the intervertebral disc on the side of flexion and rotation, with nuclear material moving to the opposite side (site of the convexity), and the posterolateral annular wall is stretched. [2]
The intervertebral foramina house the exiting cervical nerves. The largest cervical spine foramen is at the C2-3 level, and the smallest foramen is at the C6-7 level. [19] The cervical foramina become very dynamic during cervical spine ROM. The intervertebral foramina enlarge with flexion and decrease with extension. In rotation, the ipsilateral side becomes smaller, and the contralateral side enlarges. The extreme changes of the foramina occur with coupled movements (ie, flexion-rotation and extension-rotation-lateral flexion). [20]
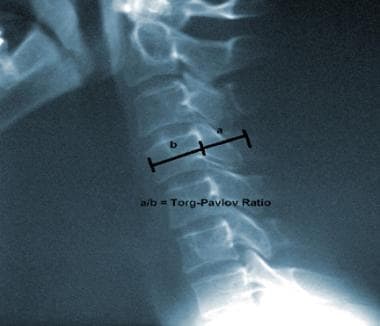
In addition to the above biomechanical concerns, cervical spinal stenosis has been evaluated with regard to catastrophic cervical sports injuries. The Torg/Pavlov ratio (measured by dividing the sagittal diameter of the spinal canal by the sagittal diameter of the vertebral body) when less than 0.8 was thought to subject the football player to high risk of cervical cord injury due to suspected cervical stenosis (see image below). However, subsequent studies found that this ratio may be erroneously low in players that have wide vertebral bodies. A study by Cantu suggested that functional stenosis as documented by myelogram or magnetic resonance imaging (MRI) may be a more appropriate measure of stenosis. [7]
Classification of athletic cervical spine injuries
A review by Bailes and Maroon classified athletes with cervical injuries into 3 types [5] :
-
Type I injuries were those that caused permanent spinal cord damage, including conditions such as anterior cord syndrome, Brown-Sequard syndrome, central cord syndrome, and mixed incomplete syndrome.
-
Type II injuries were classified as those that occur transiently after athletic trauma with normal neurologic examination and normal radiologic evaluation. Type II injuries included spinal concussion neurapraxia, and "burning hands" syndrome. The burning hands syndrome was described as suspected injury to the spinothalamic and corticospinal tracts, resulting in arm and hand weakness with burning dysesthesias. [21] This is distinct from the burner or stinger injury that is a common cervical injury in football players and is thought to be due to traction on the upper trunk of the brachial plexus. In this condition, athletes typically have a burning, dysesthetic pain that begins in the shoulder region and radiates unilaterally into the arm and hand, with C5-C6 distribution numbness or weakness.
-
Type III injuries were classified in athletes with only radiologic abnormalities but without neurologic deficit. These included congenital spinal stenosis, acquired spinal stenosis, herniated cervical disc, an unstable fracture, fracture/dislocation, ligamentous injury, and spear-tackler’s spine. Spear tackler’s spine was described by Torg et al described athletes that were at high risk for quadriplegic injury. These athletes had developmental cervical canal stenosis, reversal of the cervical lordosis, preexisting posttraumatic cervical radiographic abnormalities, and documentation of using spear-tackling techniques.
Etiology
Degenerative changes
Degenerative changes appear early in the lower cervical spine, with the most severe changes occurring at the C5-6 and C6-7 levels. According to Kramer, this is due to the mechanical influence on the cervical intervertebral discs by the extensive movement carried out in the cervical spine in relation to the rigid thoracic spine. [4] Therefore, the comparative loading per squared centimeter by the head on the cervical discs exceeds that of the thoracic and lumbar spine. [4] Cervical spine degenerative changes appear first in the intervertebral discs during the third, fourth, and fifth decades of life.
Degenerative disc changes are appreciated by loss of intervertebral disc height and osteophyte development at the origins of the vertebral endplates. These changes lead to loss of shock-absorbing capacity, resulting in abnormal force transmission and increased load to the zygapophyseal joints. Therefore, cervical zygapophyseal joint degenerative changes commonly follow intervertebral disc degeneration. [2, 4] The combination of decreased intervertebral disc space and facet joint degeneration with hypertrophy causes narrowing of the intervertebral foramina, with potential compression of the exiting nerves and associated radicular symptoms.
Creep is the further detectable movement that occurs after maximal ROM is attained and a constant force is continued on a collagenous structure. [22] Creep is believed to be due to gradual rearrangement of collagen fibers, proteoglycans, and water content in the ligament or capsule being stressed. As the water content of the nucleus pulposus decreases with disc degeneration and aging, the ability to imbibe water and distribute compressive loads also decreases, [23] resulting in increased creep under compression, which can cause incompetence of the annulus. Hickey and Hukins reported that if ligaments were stretched more than 4% of their resting length, irreversible damage would follow. [24]
As disc degeneration continues, the distinction between the margins of the nucleus and annulus becomes obscured. The negatively charged proteoglycan side chains decrease with subsequent loss of their imbibing capabilities. During this process, the overall collagen content within the disc increases. Primary annular disruption initially may occur in the periphery and is referred to as a rim lesion. As the process continues to progress and the margins of the annulus and nucleus coalesce with infiltration of type III collagen, the gelatinous nucleus becomes replaced and the disc essentially becomes fibrotic. [25, 26, 27, 28]
A study by Abdalkader et al found that in 100 athletes who underwent spinal MRI during the 2016 Olympic Summer Games, 126 cervical discs fell into one of the Pfirrmann disc degeneration grades, I through V. That included 55 discs (43.6%) with mild degenerative changes, 17 discs (13.5%) with moderate degenerative changes, and 1 disc (0.8%) with severe degenerative changes. Cervical degenerative changes were most common among athletes who competed in athletics, boxing, or swimming. [29]
Predisposing and precipitating factors for cervical discogenic pain syndrome
Predisposing and precipitating factors for cervical discogenic pain syndrome (CDPS) include prolonged sitting with poor posture (eg, protruded head posture), frequent of flexion, sudden unexpected movements, and trauma.
Harms-Ringdahl was able to provoke pain in individuals who were asymptomatic by maintaining a protruded sitting posture. [30] All subjects in the study reported neck pain within 2-15 minutes.
Static loading with poor sitting or lying postures eventually lead to problems within the cervical spine. Poor posture can also enhance or perpetuate an already existing cervical pain from trauma or whiplash injury.
Kramer reported that most patients in his practice developed pain for no apparent reason. [4]
Frequent flexion of the cervical spine is another predisposing factor in the production of symptoms from the cervical spine.
Sudden unexpected movements, particularly those that involve lateral flexion and rotation of the head and neck with the neck in a protruded position, can cause or precipitate neck pain. Trauma to the cervical spine is commonly seen as a result of whiplash forces occurring during significant motor vehicle accidents or in sports-related cervical spine injuries.
Patient Education
Inform patients that the natural history of an acute radiculopathy suggests that most patients recover within several weeks to months and that surgery is generally not necessary. Educate patients with cervical discogenic pain syndrome (CDPS) regarding home program activities, which may be performed on a routine basis to help strengthen their spine and associated muscle groups, which may help prevent injury in the future.
-
Appearance of torticollis as a result of sternomastoid fibrosis in a young child.
-
Lateral cervical spine plain radiograph illustrating the Torg/Pavlov ratio.
-
Axial computed tomography scan of cervical herniated nucleus pulposus.
-
T1-weighted magnetic resonance image of a cervical disk herniation.
-
T2-weighted magnetic resonance image of a cervical disk herniation.
-
Myelogram of cervical herniated disk. A filling defect is shown.
-
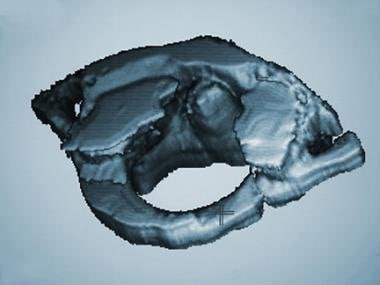
Three-dimensional computed tomography scan of C1.
-
Lateral view of a C2 fracture dislocation.