Practice Essentials
Voluntary, or skeletal, muscle is the largest single organ of the human body and accounts for nearly 50% of the body's weight. The number of muscles in the body depends on the degree of subdivision that is considered and on the number of variable muscles that are included. Not counting heads, bellies, and other divisions of muscles, the Nomina Anatomica reported by the International Anatomical Nomenclature Committee under the Berne Convention lists 200 paired muscles, or a total of 400 muscles.
Any one of these muscles can develop myofascial trigger points (MTrPs). [1, 2] MTrPs are hyperirritable tender spots in palpable tense bands of skeletal muscle that refer pain and motor dysfunction, often to another location. [3, 4] See the image below.
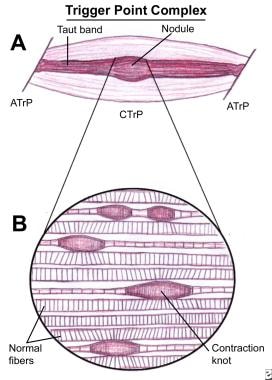 Myofascial pain in athletes. Schematic of a trigger point complex of a muscle in longitudinal section.A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP).B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of one sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
Myofascial pain in athletes. Schematic of a trigger point complex of a muscle in longitudinal section.A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP).B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of one sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
Signs and symptoms
Active trigger points (TrPs) produce a clinical complaint, usually pain, that the patient recognizes when the TrP is compressed digitally. The patient is aware of the pain caused by an active TrP, but he or she may or may not be aware of the dysfunction it causes.
Latent TrPs characteristically cause increased muscle tension and limit the stretch range of motion, which often escapes the patient's attention or is simply accepted.
See Presentation for more detail.
Diagnosis
No laboratory test or imaging technique is generally established as useful in the diagnosis of TrPs.
Surface electromyography (EMG) and ultrasonography have much potential for clinical application in the diagnosis and treatment of TrPs.
See Workup for more detail.
Management
Effective treatment of a myofascial pain syndrome caused by TrPs usually involves more than simply applying a procedure to TrPs. Often, it is necessary to consider and deal with the cause that activated the TrPs, to identify and correct any perpetuating factors (which often are different than what activated the TrPs), and to help the patient restore and maintain normal muscle function.
See Treatment and Medication for more detail.
Background
The myofascial pain syndromes (MPS) owe their ever-widening acceptance to the pioneering work of Travell and her later collaboration with Simons. [3, 4] In 1983, they combined their clinical experience in a detailed description of the multiple pain syndromes attributed to this disorder. In doing so, they further defined the major clinical components that are characteristic of myofascial pain, the most important being the TrP, the taut band, and the local twitch response. See the image below.
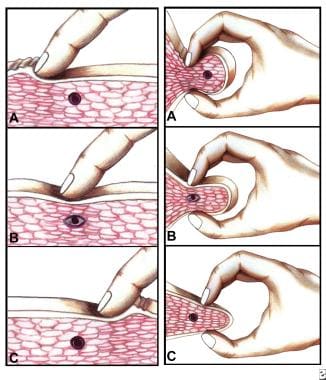 Myofascial pain in athletes. Cross-sectional drawing shows flat palpation of a taut band and its trigger point.Left: Skin pushed to one side to begin palpation (A). The fingertip slides across muscle fibers to feel the cord-line texture of the taut band rolling beneath it (B). The skin is pushed to other side at completion of movement. This same movement performed vigorously is snapping palpation (C).Right: Muscle fibers surrounded by the thumb and fingers in a pincer grip (A). The hardness of the taut band is felt clearly as it is rolled between the digits (B). The palpable edge of the taut band is sharply defined as it escapes from between the fingertips, often with a local twitch response (C).
Myofascial pain in athletes. Cross-sectional drawing shows flat palpation of a taut band and its trigger point.Left: Skin pushed to one side to begin palpation (A). The fingertip slides across muscle fibers to feel the cord-line texture of the taut band rolling beneath it (B). The skin is pushed to other side at completion of movement. This same movement performed vigorously is snapping palpation (C).Right: Muscle fibers surrounded by the thumb and fingers in a pincer grip (A). The hardness of the taut band is felt clearly as it is rolled between the digits (B). The palpable edge of the taut band is sharply defined as it escapes from between the fingertips, often with a local twitch response (C).
Etiology
Causes of myofascial pain include or are related to the following:
-
The lack of motor unit action potentials due to the endogenous contracture of the contractile elements, rather than a nerve-initiated contraction of the muscle fibers
-
The frequency with which muscle overload activates TrPs, which may reflect the marked mechanical vulnerability of the synaptic cleft region of an endplate
-
The release of substances that could sensitize nociceptors in the region of the dysfunctional endplate of the TrP as a result of tissue distress caused by the energy crisis
-
The effectiveness of essentially any technique that elongates the TrP portion of the muscle to its full stretch length even briefly, which could break the cycle that includes energy-consuming contractile activity
-
Laborers who exercise their muscles heavily every day are less likely to develop active TrPs than sedentary workers who are prone to intermittent episodes of vigorous physical activity. This author's clinical experience supports this observation.
Epidemiology
United States data
MTrPs are extremely common and become a painful part of nearly everyone's life at one time or another. Latent TrPs, which often cause motor dysfunction (eg, stiffness, restricted range of motion) without pain, are far more common than active TrPs that cause pain.
Active TrPs are commonly found in postural muscles of the neck, shoulder, and pelvic girdles and in the masticatory muscles. In addition, the upper trapezius, scalene, sternocleidomastoid, levator scapulae, and quadratus lumborum muscles are commonly involved.
Reports of the prevalence of MTrPs in specific patient populations are available. The data indicate a high prevalence of this condition among individuals with a regional pain complaint, as shown in Table 1.
Table 1. Prevalence of Myofascial Pain (Open Table in a new window)
Region |
Practice |
Number Studied |
Prevalence of Myofascial Pain, % |
General |
Medical |
172 |
30 |
General |
Pain medical center |
96 |
93 |
General |
Comprehensive pain center |
283 |
85 |
Craniofacial |
Head and neck pain clinic |
164 |
55 |
Lumbogluteal |
Orthopedic clinic |
97 |
21 |
The wide range in the prevalences of myofascial pain caused by TrPs is likely due to differences in the patient populations examined and in the degree of chronicity, at least in part. Probably even more important are differences in the criteria used to diagnose MTrPs and, most important, differences in the training and skill of the examiners.
Functional Anatomy
Some isolated large round muscle fibers and some groups of these darkly staining, enlarged, round muscle fibers appear in cross-sections. In longitudinal sections, the corresponding feature is a number of contraction knots. An individual knot appears as a segment of muscle fiber with extremely contracted sarcomeres. This contractured segment has a corresponding increase in diameter of the muscle fiber.
The structural features of contraction knots presents a likely explanation for the palpable nodules and the taut bands associated with TrPs. Three single contraction knots can be seen scattered among normal muscle fibers. Beyond the thickened segment of the contractured muscle fiber at the contraction knot, the muscle fiber becomes markedly thinned and consists of stretched sarcomeres to compensate for the contractured ones in the knot segment. In addition, a pair of contraction knots separated by empty sarcolemma may represent one of the first irreversible complications that result from the continued presence of the contraction knot.
Sport Specific Biomechanics
The activation of a TrP is usually associated with some degree of mechanical abuse of the muscle in the form of muscle overload, which may be acute, sustained, and/or repetitive. In addition, leaving the muscle in a shortened position can convert a latent TrP to an active TrP; this process is greatly aggravated if the muscle is contracted while in the shortened position.
In paraspinal muscles (and likely other muscles, too), a degree of nerve compression that causes identifiable neuropathic electromyographic (EMG) changes is associated with an increase in the numbers of active TrPs. These TrPs may be activated by disturbed microtubular communication between the neuron and the endplate because the motor endplate is involved in the pathophysiologic process of the peripheral core TrP.
The histopathologic complications that could contribute to the chronicity of the condition and make treatment more difficult include the following:
-
Distortion of the striations (sarcomere arrangement) in adjacent muscle fibers for some distance beyond the contraction knot (see the image below). This produces unnatural shear forces between fibers that could seriously and chronically stress the sarcolemma of the adjacent muscle fibers. If the membrane were stressed to the point at which it became pervious to the relatively high concentration of calcium in the extracellular space, it could induce massive contracture that could compound the shear forces.
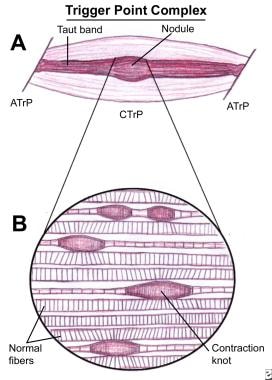 Myofascial pain in athletes. Schematic of a trigger point complex of a muscle in longitudinal section.A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP).B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of one sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
Myofascial pain in athletes. Schematic of a trigger point complex of a muscle in longitudinal section.A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP).B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of one sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
-
The occasional finding of a segment of an empty sarcolemmal tube between 2 contractions knots may represent an additional irreversible complication of a contraction knot.
Latent TrPs can produce other effects characteristic of a TrP, including increased muscle tension and muscle shortening; but these do not produce spontaneous pain. Both active and latent TrPs can cause significant motor dysfunction. The same factors that are responsible for the development of an active TrP can, to a lesser extent, cause a latent TrP. An active key TrP in one muscle can induce an active satellite TrP in another. Inactivation of the key TrP often inactivates its satellite TrP without treatment of the satellite TrP itself.
The intensity and extent of the pattern of referred pain depends on the degree of irritability in the TrP, not on the size of the muscle. MTrPs in small, obscure, or variable muscles can be as troublesome to the patient as TrPs in large familiar muscles.
TrPs are activated directly by acute overload, overwork fatigue, direct impact trauma, and radiculopathy. TrPs can be activated indirectly by other existing TrPs, visceral disease, arthritic joints, joint dysfunctions, and emotional distress. Satellite TrPs are prone to develop in muscles that lie within the pain reference zone of key MTrPs or within the zone of pain referred from a diseased viscus, such as the pain due to myocardial infarction, gastric ulcer, cholelithiasis, or renal colic. A perpetuating factor increases the likelihood of overload stress that can convert a latent TrP to an active TrP.
With adequate rest and in the absence of perpetuating factors, an active TrP may spontaneously revert to a latent state. Pain symptoms disappear; however, occasional reactivation of the TrP by exceeding that muscle’s stress tolerance can account for a history of recurrent episodes of the same pain over a period of years.
Prognosis
Complications
The single muscle MPSs usually are acute and follow an episode of muscle overload. In some cases, the pain persists and spreads to other, usually synergistic, muscles. This is referred to as a chronic regional myofascial syndrome.
Many perpetuating factors encourage transformation to a more widespread muscle pain problem. Mechanical factors include postural stress, muscle imbalances, and skeletal asymmetries. These can put additional stress on surrounding muscles, leading to spread of dysfunction and pain. Systemic perpetuating factors purportedly include anything jeopardizing the energy supply to muscle (ie, anemia, endocrine imbalances, low thyroid function, vitamin deficiencies). Advise patients to avoid these mechanical and systemic factors if possible.
Chronic regional myofascial syndromes are conceptually close to the malignant, metastasizing fibromyalgia referred to by Bennett.
Return to play
Athletes should avoid strenuous activity during sports, and they should always use stretching techniques prior to competitions or practice.
Patient Education
The ultimate goal is to educate patients and (1) to provide them with the means to manage their own muscle pain disorder, (2) to eliminate their dependence on healthcare providers, (3) to eliminate contributing factors, providing prolonged stretch of the affected muscle, and aerobic exercises. [5]
On performing a task, the patient must learn to keep the muscles mobilized, and not held fixed in a contracted position. Muscle fibers need to alternately contract and relax to provide blood flow and replenish their energy supply.
-
Myofascial pain in athletes. Schematic of a trigger point complex of a muscle in longitudinal section.A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP).B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of one sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
-
Myofascial pain in athletes. Cross-sectional drawing shows flat palpation of a taut band and its trigger point.Left: Skin pushed to one side to begin palpation (A). The fingertip slides across muscle fibers to feel the cord-line texture of the taut band rolling beneath it (B). The skin is pushed to other side at completion of movement. This same movement performed vigorously is snapping palpation (C).Right: Muscle fibers surrounded by the thumb and fingers in a pincer grip (A). The hardness of the taut band is felt clearly as it is rolled between the digits (B). The palpable edge of the taut band is sharply defined as it escapes from between the fingertips, often with a local twitch response (C).
-
Myofascial pain in athletes. Longitudinal schematic drawing of taut bands, myofascial trigger points, and a local twitch response. A: Palpation of a taut band (straight lines) among normally slack, relaxed muscle fibers (wavy lines). B: Rolling the band quickly under the fingertip (snapping palpation) at the trigger point often produces a local twitch response that usually is seen most clearly as skin movement between the trigger point and the attachment of the muscle fibers.
-
Myofascial pain in athletes. Sequence of steps to use when stretching and spraying any muscle for myofascial trigger points.
-
Myofascial pain in athletes. Schematic drawing showing how the jet stream of Vapo coolant is applied.
-
Myofascial pain in athletes. Cross-sectional schematic drawing shows flat palpation to localize and hold the trigger point for injection. A and B show use of alternate pressure between 2 fingers to confirm the location of the palpable module of the trigger point. C shows positioning the trigger point half way between the fingertips to keep it from sliding to one side during the injection.
-
Myofascial pain in athletes. Schematic top view of 2 approaches to the flat injection of a trigger point area in a palpable taut band. Injection away from the fingers (A) and injection toward the fingers (B).
-
Myofascial pain in athletes. C. Z. Hong's technique. Finger pressure beside the needle is used to indent the skin, subcutaneous, and fat tissues so that the needle can reach the trigger point in a muscle that would be inaccessible otherwise.
-
Myofascial pain in athletes. Diagrammatic representation of pre-injection sites (open circles) and injection sites (solid circles) of local anesthetic to the trigger point. The enclosed stippled area represents the taut band. This diagram distinguishes the central trigger point within the large broken circle from the attachment trigger points located at the myotendinous junction and at the attachment of the tendon to the bone. Each of these 3 trigger point regions can be identified by their individual spot tenderness and anatomical locations. No rationale is apparent for injecting the part of the taut band that lies between the central trigger point and the attachment trigger point (solid circles numbers 7-10).
-
Myofascial pain in athletes. Mechanism of botulinum toxin type A.
-
Myofascial pain in athletes. Binding of neuromuscular transmission with botulinum toxin type A, which binds the motor nerve terminal.
-
Myofascial pain in athletes. After botulinum toxin type A is internalized, the light chain of the toxin molecule is released into the cytoplasm of the nerve terminal.
-
Myofascial pain in athletes. Botulinum toxin type A blocks acetylcholine by cleaving a cytoplasmic protein on the cell membrane.
-
Myofascial pain in athletes. After the botulinum toxin type A exerts its clinical toxic effect, a nerve sprout eventually establishes a new neuromuscular junction, and muscle activity gradually returns. However, new research findings suggest that this new nerve sprout retracts and the original junction returns to functionality.
-
Myofascial pain in athletes. After the clinical toxic effect of botulinum toxin type A occurs, axon sprouting and muscle fiber reinnervation terminate the clinical effect of the toxin, which results in the reestablishment of neuromuscular transmission.







