Background
Several types of quadriceps injuries can occur, the most common being the quadriceps contusion, which is painful and disabling. The usual cause of the quadriceps contusion is a direct blow to the anterior thigh from an object or another person (eg, helmet, knee). Very rarely, this injury can be severe enough to progress to an acute compartment syndrome.
Because the quadriceps is in contact with the femur throughout its length, it is susceptible to compression forces. The rectus femoris is the most commonly injured portion of the muscle because of its anterior location. Minimally, impact causes cellular edema of the muscle, but complete capillary disruption with localized hemorrhage leading to a tense anterior compartment can occur. The muscle is more resistant to injury if it is struck while in a contracted nonfatigued state. Other quadriceps injuries range from simple strains to more complex and disabling muscle ruptures. See the image below.
Other types of quadriceps injuries include strains of the quadriceps tendon, complete and partial tears of the quadriceps tendon, and fascial rupture of the quadriceps muscle. Specific areas of the quadriceps are affected for each of these diagnoses. The classic quadriceps strain occurs at the conjoined muscle tendon junction (jumper's knee). The partial tear of the quadriceps most commonly affects the indirect (distal) head of the rectus femoris. Fascial rupture usually occurs anteriorly at the mid thigh and causes a muscle hernia.
Causes of quadriceps injury are as follows:
-
Quadriceps contusion or compartment syndrome - Direct blow to anterior aspect of thigh
-
Quadriceps strain or rupture - Acute stretch or repeated eccentric muscle contractions with immediate or delayed (1-3 d) presentation of pain, stiffness, and decreased function
For patient education resources from eMedicineHealth, see Avoiding Sports Injuries, as well as Muscle Strain.
Epidemiology
United States statistics
Although quadriceps strains are common, minimal information about the frequency with respect to specific sports is available. As for quadriceps contusions, the most detailed frequency data came from the US Military Academy at West Point, [1] and the distribution per year was reported as follows: rugby 4.7%, karate and judo 2.3%, football 1.6%, and all other sports fewer than 1%. Quadriceps muscle hernias are believed to be more common in soccer, basketball, and rugby.
A study by Eckard et al that analyzed data from the NCAA Injury Surveillance Program from 2009 to 2015 found that the on quadriceps strain injury rate was 1.07/10 000 athlete-exposures. Almost 78% of quadriceps strains were sustained during practice, however, the rate was higher during competition than during practice (approximately 1.3 versus 1.0/10 000 Athlete-exposures). The sports with the highest injury rates were women's soccer (5.61/10 000 AEs), men's soccer (2.52/10 000 AEs), women's indoor track (2.24/10 000 AEs), and women's softball (2.15/10 000 AEs). Overall, women had a higher rate of quadriceps strains than men. [2]
The incidence of jumper's knee at the quadriceps insertion onto the patella is less common than patellar tendinitis. One study reported that of all tendinopathies affecting the extensor mechanism, the frequency of patellar tendinitis at its insertion was 65%, quadriceps tendinitis was 25%, and patellar tendinitis at its insertion into the tibial tuberosity was 10%.
The estimated incidence of quadriceps tendon rupture is 1.37 cases per 100,000 persons per year. [3] Rupture of the quadriceps tendon is more common in both older patients and younger athletes. Several studies show that the mean age of patients with quadriceps rupture is about 65 years. However, in athletes, the mean age cited ranges from 15 to 30 years. Sports associated with quadriceps rupture are high jump, basketball, and weight lifting. Rupture is also not uncommon in patients with renal failure.
Functional Anatomy
The quadriceps femoris acts as a hip flexor and knee extender. The quadriceps femoris is composed of the following:
-
Rectus femoris
-
Vastus lateralis
-
Vastus medialis
-
Vastus interomedialis
Origins/insertions of quadriceps components include the following:
-
Rectus femoris - Ilium/tibial tuberosity
-
Vastus lateralis - Femur/tibial tuberosity
-
Vastus medialis - Femur/tibial tuberosity
-
Vastus interomedialis - Femur/tibial tuberosity
The 3 thigh compartments are as follows:
-
Anterior - Quadriceps muscles, femoral nerve and artery
-
Posterior - Hamstring muscles, sciatic nerve
-
Medial - Adductor muscles, cutaneous branch of obturator nerve
Sport-Specific Biomechanics
The function of the quadriceps is primarily that of tibial (knee) extension. One electromyography (EMG) study showed that the maximum extension moment and maximum quadriceps EMG activity were early in the kicking action, as the initial flexion changes to extension. This moment occurs before the foot makes contact with the ball. The peak activity of the hamstring occurs after the quadriceps peak, shortly before the ball is struck. The largest extension moment in this study was 260 Nm; this corresponds to a calculated tensile force in the patellar tendon of 7 times body weight.
The mechanical properties of the quadriceps have been studied. The central aspect of 10-mm wide sections of the quadriceps was subjected to tensile loading and compared to a similar patellar tendon section. The ultimate load to failure of the unconditioned patellar tendon was higher (53.4 N/mm2) than the unconditioned quadriceps tendon (33.6 N/mm2). Strain at failure was also higher for the preconditioned patellar tendon (14.4%) than for the quadriceps tendon (11.2%).
Microscopic sections of human quadriceps tendon as it inserts into the patella show no crimping and no cement line. This is unlike other tendon insertion sites. The interdigitation between collagen fibers and the distinction between tendon and bone was least distinct along the anterior third of the patella.
A discussion of the biomechanics of specific injuries is as follows:
-
Strains, overuse, and rupture: The most common sites of injury correlate to the muscle tendon junctions both proximally and distally and to the muscle belly itself. Muscle strains are usually due to repetitive functional overload. Not surprisingly, quadriceps strains most commonly affect athletes who subject their knees to high levels of repeated loading of the extensor mechanism. The overuse trauma may range from microscopic failure of soft tissue with its associated inflammation or gross rupture. Gross rupture may be partial or complete. A large sudden load may cause the entire insertion to be compromised, leading to complete rupture. Repetitive loading, particularly eccentric loads, causes microfailure, usually at the muscle tendon junction. This microfailure can result in partial tears.
-
Contusion: Direct trauma to the quadriceps may cause muscle fiber and connective tissue rupture and formation of a hematoma. Trauma to the quadriceps causes muscle fiber rupture, disruption of connective tissue, and hematoma formation. Inflammatory cells and macrophages enter the site of injury and begin clearing necrotic muscle cells. This process occurs over 2-3 days. Then, muscle cells attempt to regenerate at the same time scar tissue is being formed. A severe thigh contusion can lead to a compartment syndrome.
-
Muscle hernia: The cause of this is not clear. It is usually associated with a sudden forceful kick, but it may be associated with a weakened or previously injured quadriceps fascia.
Prognosis
If treated properly, a full recovery is expected, although recovery times vary from days to months.
Complications
Myositis ossificans may occur at 3 or more months postinjury.
-
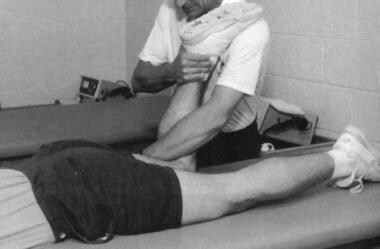
Place knee passively in 120º of flexion and immobilize with a double elastic wrap in a figure-8 fashion. This should occur within minutes of the injury. Used with permission courtesy of John Aronen, MD.
-
Modified treatment of quadriceps contusion. Used with permission courtesy of John Aronen, MD.