Practice Essentials
The posterior cruciate ligament (PCL) is described as the primary stabilizer of the knee by many authors. PCL injuries are less common than anterior cruciate ligament (ACL) injuries, and they often go unrecognized. The PCL is broader and stronger than the ACL and has a tensile strength of 2000 N. Injury most often occurs when a force is applied to the anterior aspect of the proximal tibia when the knee is flexed. Hyperextension and rotational or varus/valgus stress mechanisms also may be responsible for PCL tears. Injuries may be isolated or combined with other ligamentous injuries. A PCL tear can result in varying degrees of disability, from no impairment to severe impairment. PCL injury has been overly simplified, and the functional disability of PCL injury may be underestimated. [1] The radiographs below demonstrate the results of such injuries, comparing a normal knee with one that has a damaged PCL.
 A normal lateral radiograph of a knee. In a normal knee, a line drawn along the posterior femoral condyle will not intersect the posterior tibial condyle.
A normal lateral radiograph of a knee. In a normal knee, a line drawn along the posterior femoral condyle will not intersect the posterior tibial condyle.
 A lateral radiograph of a knee with a posterior cruciate ligament injury. Note that the same line as in the above image will bisect the posterior tibial condyle due to a posterior sag and an incompetent posterior cruciate ligament.
A lateral radiograph of a knee with a posterior cruciate ligament injury. Note that the same line as in the above image will bisect the posterior tibial condyle due to a posterior sag and an incompetent posterior cruciate ligament.
The primary function of the PCL is to prevent posterior translation of the tibia on the femur. The PCL also plays a role as a central axis controlling and imparting rotational stability to the knee. This injury has received little attention in the past, compared with the ACL; however, this emphasis on the ACL has stimulated increased interest in the treatment of PCL injuries. Controversy regarding treatment of isolated PCL injuries exists in the literature, with recommendations supporting both operative and nonoperative therapy. Current management of PCL injuries unfortunately can yield relatively poor clinical outcomes, whether surgically or conservatively treated. [2]
Epidemiology
United States statistics
True incidence in the United States is unknown. In National Football League predraft physical examinations, a 2% incidence of isolated, asymptomatic, and unknown PCL injuries was found; operated, isolated, and combined PCL injuries were reported at an incidence of 3.5-20%. On the KT-1000 stress test examination, a 7% incidence of PCL injuries was found, of which 40% were isolated and unidirectional and 60% were multidirectional. A retrospective study by Sanders et al determined the that the age- and sex-adjusted annual incidence of isolated, complete PCL tears was 1.8 per 100,000. [3]
Functional Anatomy and Etiology
Functional anatomy
As demonstrated in the images below, the PCL originates from the intercondylar notch of the femur on the roof of the medial femoral condyle. The insertion is central on the posterior aspect of the tibial plateau, on a depression between the tibial plateaus, extending 1 cm below the articular surface. [4] The ligament is composed of a larger anterolateral bundle and a smaller posteromedial bundle. The anterior component is tightest in the midarc of flexion and the posterior fibers are tight in extension and deep flexion.
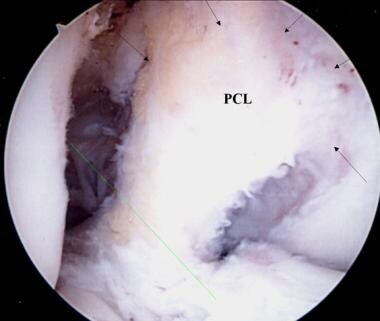 A view of the broad origin of the posterior cruciate ligament (PCL) on the medial femoral condyle of a left knee. The anterior cruciate ligament has been removed for surgical reconstruction.
A view of the broad origin of the posterior cruciate ligament (PCL) on the medial femoral condyle of a left knee. The anterior cruciate ligament has been removed for surgical reconstruction.
 An additional view of the posterior cruciate ligament broad origin and insertion in a knee pending anterior cruciate ligament reconstruction.
An additional view of the posterior cruciate ligament broad origin and insertion in a knee pending anterior cruciate ligament reconstruction.
In addition, variable anterior and posterior meniscofemoral ligaments of Humphrey and Wrisberg attach distally and proximally to the PCL, respectively. The meniscofemoral ligaments attach distally to the posterior horn of the lateral meniscus, in a slanting orientation, providing resistance to the tibial posterior drawer. [5] The PCL is an extrasynovial structure that lies behind the intra-articular portion of the knee. The primary function of the PCL is to resist posterior displacement of the tibia in relation to the femur; its secondary function is to prevent hyperextension and limit internal and varus/valgus rotation.
Etiology
Possible causes of PCL injuries include the following:
-
Football injuries
-
Running injuries
-
Motor vehicle accidents
-
Falls onto a flexed knee
Studies show that differences in the shape of the knee are associated with PCL rupture after an injury. A smaller and more sharply angled intercondylar notch and a more flattened tibial eminence are related to rupture. This suggests that knee morphology affects the risk of sustaining a PCL rupture. [6]
Sport Specific Biomechanics
Through various experimental designs, the biomechanical role of the PCL has been elucidated. The PCL has its most well-defined role as a primary restraint/stabilizer to posterior stress, and it seems this role is greatest at higher degrees of knee flexion. [7]
Disruption may occur with forced hyperextension while the foot is planted in dorsiflexion. A force applied to the anteromedial aspect of the knee, as during a football tackle, results in a posteriorly directed force and a varus hyperextension force, leading to PCL and posterolateral capsular ruptures.
Prognosis
Complications
Possible complications associated with PCL injury include the following:
-
Initial stiffness
-
Instability
-
Progressive arthritis
-
Postoperative complications
Patient Education
Patient education is very important throughout the rehabilitation process for individuals with PCL injuries. Athletes should be informed of the benefits and risks of possible treatments and be involved in the decision-making process. To achieve their goals and be able to return to play, patients need to be compliant with their physician's instructions and physical therapy program as outlined by their therapist. As patients progress through their rehabilitation program, they should be instructed in a home exercise program for continued strengthening to decrease their risk for a recurrent injury.
For patient education resources, see Knee Injury and Knee Pain.
-
A normal lateral radiograph of a knee. In a normal knee, a line drawn along the posterior femoral condyle will not intersect the posterior tibial condyle.
-
A lateral radiograph of a knee with a posterior cruciate ligament injury. Note that the same line as in the above image will bisect the posterior tibial condyle due to a posterior sag and an incompetent posterior cruciate ligament.
-
The posterior tibial sag sign. The photo on the left demonstrates the clinical finding of the posterior tibial sag sign. A line drawn parallel to the patella accentuates the posterior tibial sag. The photo on the right demonstrates the quadriceps active drawer test described by Daniels. With the knee in 70-90° of flexion, the extensor mechanism is contracted, pulling the tibia anteriorly into a reduced position.
-
A close-up view of a posterior tibial sag with an incompetent posterior cruciate ligament.
-
This MRI of the knee shows a torn posterior cruciate ligament.
-
This MRI (coronal section) shows a posterior cruciate ligament tear.
-
This transverse MRI shows edema to the torn posterior cruciate ligament.
-
A view of the broad origin of the posterior cruciate ligament (PCL) on the medial femoral condyle of a left knee. The anterior cruciate ligament has been removed for surgical reconstruction.
-
An additional view of the posterior cruciate ligament broad origin and insertion in a knee pending anterior cruciate ligament reconstruction.
-
A right knee pending posterior cruciate ligament (PCL) reconstruction. A minimal notchplasty is completed. Two guide pins are advanced into the medial femoral condyle for tunnel placement to reconstruct the 2 bundles of the PCL.
-
The 2 tunnels are created by reaming from outside in; 8- to 9-mm tunnels are made depending on patient size and the graft that will be used.
-
Two red Robinson catheters are advanced through the femoral tunnels.
-
The catheters have premade holes, which are used for suture retrieval.
-
The catheters are advanced and threaded out the posterior knee. In this case, a posterior tibial onlay graft from an Achilles tendon allograft is used. The 2 bundles are secured to the catheters and advanced into the joint through the tunnels.
-
The 2 Achilles tendon bundles are secured with a baseball whipstitch, are threaded through the catheter holes, and are advanced into the femoral condyle tunnels.
-
Additional view of the placement and advancement of the Achilles allograft.
-
Completion and seating of the femoral allograft reconstruction. The 2 bundles are secured or stabilized by suturing over a post and washer. Note the reestablishment of the broad surface area for the reconstructed posterior cruciate ligament origin.
-
Completion of the tibial onlay, 2-bundle Achilles tendon allograft/posterior cruciate ligament (PCL) reconstruction. The bony calcaneus remnant is secured to the posterior tibia with 1 or 2 interfragmentary compression screws into a trough into the posterior tibia at the level of the PCL insertion. Care is taken to not penetrate the anterior tibial cortex with these screws. Note the intact original anterior cruciate ligament.







