Practice Essentials
Low back pain (LBP) is ubiquitous. An estimated 30-45% of persons aged 18-55 years have some form of back pain in their lifetime. LBP most commonly involves one of the following conditions: sciatic nerve entrapment, herniated nucleus pulposus, direct trauma, muscle spasm due to chronic or overuse injury, or piriformis syndrome.
Piriformis syndrome (see the image below) is characterized by pain and instability. The location of the pain is often imprecise, but it is often present in the hip, coccyx, buttock, groin, or distal part of the leg. The history and physical findings are key elements in differentiating the more common forms of LBP and piriformis syndrome. The literature and general knowledge on piriformis syndrome is limited, compared with that of sciatica or disc herniation. However, the common findings associated with piriformis syndrome are agreed upon.
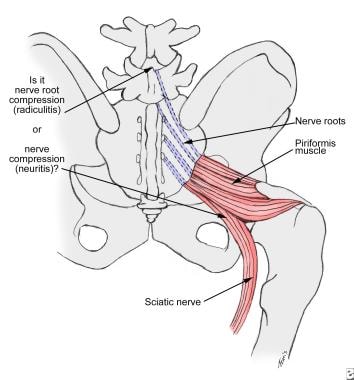 Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).
Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).
Yeoman first described piriformis syndrome in 1928 as periarthritis of the anterior sacroiliac joint. The history of this condition stems from one of many causes of lower back and leg pain. Many patients who underwent unsuccessful surgery in the lumbosacral region were later found to have piriformis syndrome.
Epidemiology
United States statistics
The female-to-male incidence ratio of piriformis syndrome is 6:1. In one study at a regional hospital, 45 of 750 patients with LBP were found to have piriformis syndrome. Another author estimated that the incidence of piriformis syndrome in patients with sciatica is 6%. The overall incidence of piriformis syndrome has been estimated at 2.4 million per year. Most cases occur in middle-aged patients. [1]
Functional Anatomy
The function of the piriformis muscle is to externally rotate and abduct the thigh. The sacral plexus is closely associated with the anterior surface of the piriformis muscle. The lumbosacral trunk and the ventral rami of the first 3 sacral nerves form the sacral plexus. The sciatic nerve passes inferior to the piriformis muscle.
The sciatic nerve exits the pelvis via 4 routes: (1) The nerve passes anteriorly to the piriformis between the rims of the greater sciatic foramen. (2) The peroneal portion of the sciatic nerve passes through the piriformis; the tibial portion passes anterior to the piriformis muscle. (3) The peroneal branch of the sciatic nerve loops above and posterior to the piriformis muscle, whereas the tibial branch passes anterior to the piriformis muscle. (4) The undivided sciatic nerve penetrates the piriformis muscle.
Dysfunction of the piriformis muscle can cause signs and symptoms of pain in the sciatic nerve distribution, that is, in the gluteal area, posterior thigh, posterior leg, and lateral aspect of the foot. [2]
Sport-Specific Biomechanics
Gait mechanics help in demonstrating the physiologic features of piriformis hypertrophy. When a person takes a step forward, the extremity moves from external rotation to internal rotation, and the piriformis muscle lengthens. This stretching is followed by reflex contraction. A second contraction in the initially stretched piriformis muscle occurs when the opposite foot swings forward. This gait pattern leads to hypertrophy, and the dual contraction is further exacerbated by the stretching of the piriformis muscle on the side of a shortened leg.
More commonly, piriformis syndrome is secondary to inflammation due to gluteal trauma or spasm. The effect of this inflammatory process on the sciatic nerve is chemical rather than mechanical. Several theories suggest that the following are key factors in the muscle hyperfunction or spasm that leads to an interstitial myofibrositis: extravasation of blood; release of serotonin from platelets; and prostaglandin E, serotonin, bradykinin, and histamine release.
Although no general consensus about the etiology and pathophysiology of piriformis syndrome exists, many physicians and physical therapists attribute this syndrome to a specific mechanism involving the sciatic nerve. For example, Benson and Schutzer attributed the syndrome to blunt trauma to the buttocks that results in hematoma formation and subsequent scarring between the sciatic nerve and the short external rotators. [3] Entrapment of the sciatic nerve at the sciatic trunk (where it leaves the pelvis and crosses the greater sciatic notch) is an infrequent cause. This entrapment can also occur as a result of an enlarged hypertrophic piriformis, an inflamed piriformis muscle, tumors, cysts, and pseudoaneurysms.
Etiology
Trauma to the buttocks or gluteal region is the most common cause of piriformis syndrome.
Skiers, truck drivers, tennis players, and long-distance bikers are at high risk.
In Morton foot, the prominent head of the second metatarsal causes foot instability and a reactive contraction of the external rotators of the hip during gait.
Spinal stenosis can lead to bilateral piriformis tenderness.
Anatomic variations of the divisions of the sciatic nerve above, below, and through the belly of the piriformis muscle may be causative factors. [4]
Prognosis
Most patients with piriformis syndrome progress well after a local trigger-point injection. Recurrences are uncommon after 6 weeks of therapy. After surgery, patients treated with piriformis release return to their activities in an average of 2-3 months.
Patient Education
Patients with piriformis syndrome should modify their activity habits. For example, patients are recommended to adhere to the following: avoid prolonged sitting, perform the suggested stretching exercises 2 or 3 times a day and before participating in a sports activity, and avoid direct trauma to the gluteal region.
Patient education should be an ongoing process throughout the course of rehabilitation. Physical therapists and occupational therapists are valuable members of the team for teaching the patient strategies used to recover from this syndrome and also to prevent recurrences. Patients should be informed of the importance of their routine compliance with an individualized home exercise program.
-
Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).








