Practice Essentials
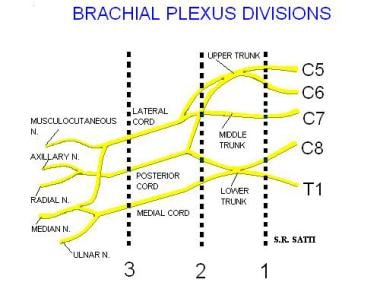
The brachial plexus represents a complex network of nerves formed from the ventral rami of the lower cervical nerves (C5-C8) and the greater portion of the ventral ramus of the first thoracic nerve (T1). The ventral rami or roots coalesce to form trunks, divisions, cords, and branches, which provide motor and sensory innervation to the upper limb and thorax. Brachial plexus injuries are classified on the basis of location, with a preganglionic injury occurring proximal to the dorsal root ganglion, and a postganglionic injury occurring distal to the dorsal root ganglion. [1, 2, 3]
A preganglionic injury, or root avulsion, disrupts the connection between the spinal nerve and the spinal cord, whereas a postganglionic injury is located within the peripheral nervous system and therefore does not affect the connection with the CNS. Patients with a postganglionic injury may regain useful function without surgery, whereas spontaneous recovery is not possible with root avulsion. [4]
Pathology of the brachial plexus is widely varied, but it tends to be due to similar mechanisms based on age. In neonates, the most common pathology of the brachial plexus is related to birth trauma. Perinatal brachial plexus palsy has a wide array of clinical symptoms ranging from incomplete paresis of an extremity to flaccid arm paralysis. [5] In adolescents and young adults, pathology is often due to high-speed trauma, such as motor vehicle accidents. In adults, neoplasm (intrinsic or extrinsic masses) or postradiation injury is frequently the cause. Traumatic injuries to the brachial plexus are associated with weakness and paresthesias of the upper extremity on the affected side. Thorough neurologic examination can be performed to localize the injury and to help pinpoint the location of pathology.
Approximately 75% of cases involve total rupture of roots C5-Th1, followed by C5-C6 injury (about 20%) and C8-Th1 (about 3%). Obstetric brachial plexus palsy caused by a traction injury to the nerves of the upper extremity occurs in 1.5 to 5.1 per 1000 births. [4, 6, 7]
(See the image below.)
Clinically, brachial plexopathy commonly mimics the symptoms and signs of cervical spondylosis-related radiculopathy, and it is important to differentiate these pathologies, as the management strategies can differ. The deep location of the brachial plexus and its complex architecture make it difficult to diagnose, characterize, and treat brachial plexus lesions, often leading to inconclusive electrodiagnostic (ED) testing. [8]
Indications for brachial plexus MRI include symptomology, pain, neural deficit, or muscular atrophy that may be due to brachial plexus pathology, postradiation treatment evaluation, or preoperative evaluation of known intrinsic or extrinsic lesions within the neck, clavicular region, or axilla.
Evaluation
MRI, CT, and radiography
Clinical evaluation of the brachial plexus can be challenging or impossible without good imaging correlation. Although the physical examination has traditionally been a mainstay in evaluating and localizing pathology involving the brachial plexus, physical examination is especially difficult in patients with scarring and fibrosis secondary to surgery or irradiation. Electrophysiologic studies can also be used to detect abnormalities in nerve conduction, but they are poor for localizing a lesion. [9] The American College of Radiology (ACR) recommends MRI for the initial evaluation of brachial plexopathy. [10] Correlation of imaging results with electrophysiologic findings increases overall specificity and sensitivity. [11, 12, 13] Large multicenter trials performed at 1.5 Tesla and 3 Tesla have demonstrated sensitivity and specificity of MRI alone at 81% and 90%, respectively. [14, 15, 16, 17]
In a study by Patel et al of MRI and electrodiagnostic studies for detection of brachial plexus injury, MRI had a sensitivity of 93.88% versus 99.32% for electrodiagnostic studies. Both, however, showed low specificity (18.28% and 20.43%, respectively). Sensitivity was 100% when both studies were used. [18] A multicenter study by Tagliafico et al that evaluated MRI accuracy reported an MRI specificity of 91.4%. [14] In a retrospective study of 35 patients who underwent MRI to detect root avulsion, Doi et al observed a sensitivity of 92.9% and a specificity of 81.3%. [19]
High-resolution 3-Tesla MR neurography (MRN) and advances in 3-dimensional techniques have resulted in improved visualization and evaluation of the brachial plexus. [20] In a study by Hilgenfeld and colleagues, results of MRN in 36 patients with clinical symptoms of brachial plexopathy were compared with those of 36 age- and sex-matched control subjects, and all patients were found to have been correctly rated as affected, whereas 34 of 36 controls were correctly rated as unaffected. Plexopathy with a compressive etiology (n = 12) was correctly distinguished from noncompressive plexopathy with inflammatory origin (n = 24). Pathoanatomic contiguity of lesion from trunk into cord level allowed recognition of distinct somatotopical patterns of fascicular involvement, which correlated closely with the spatial distribution of clinical symptoms and electrophysiologic data. [21] In a review of 43 cases of diagnosed brachial plexopathy, MRN sensitivity ranged from 41.2 to 70.6%, and specificity from 97.7 to 100%. [22]
Plain radiography can depict large lesions affecting the brachial plexus or the presence of fractures in the setting of trauma. However, radiographs are far less sensitive than other studies. Computed tomography (CT) scanning has increased sensitivity for depicting extrinsic masses that compress the nerves, as compared with radiographs, but CT offers poor soft tissue contrast for direct evaluation of the nerves of the brachial plexus.
Although conventional and CT myelography can be used to evaluate the nerve roots of the brachial plexus and to assess for pseudomeningocele formation, MRI has become increasingly important in the evaluation of brachial plexus pathology because of improved soft tissue resolution. With MRI, not only can the nerve roots of the brachial plexus be visualized, but also the trunks, divisions, and cords can be better seen, and characteristics such as course, caliber, signal intensity, fascicular pattern, and size can be better evaluated. Conventional MRI is useful for the diagnosis of mass lesions, gross nerve root avulsions, or postradiation changes. [8] Additionally, improved soft tissue differentiation allows for improved detection of intrinsic and extrinsic pathology. MRI also has the additional benefit of multiplanar imaging. The tissue resolution of MRI is constantly improving with new pulse sequences and coil designs. [9, 23, 24, 25, 26, 19, 27]
Compared with radiography and CT scanning, with which changes in the shape or position of the brachial plexus have been used to assess pathology, [28] MRI can directly visualize the nerve. Sequences such as fat-saturated T2-weighted spin-echo, short-tau inversion recovery (STIR), and gadolinium-enhanced T1-weighted spin-echo sequences help depict subtle changes in the signal intensity of the nerves or enhancement and aid in refining the differential diagnosis. In addition, maximum-intensity projections can make localization and visualization of the pathology most understandable for referring clinicians and surgeons. [29, 30]
Studies of MRI with 3D T2 STIR SPACE sequence and compressed sensing (CS) have shown increased visibility of images and image boundaries, signal-to-noise ratio (SNR), and contrast-to-noise ratio (CNR). SPACE (Sampling Perfection with Application optimized Contrast using different flip angle Evolution) is a spin echo sequence that creates high-spatial-resolution 3D datasets. [31, 32, 33]
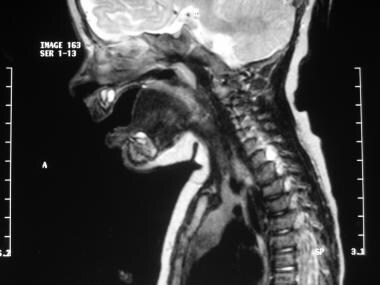
(See the images below.)
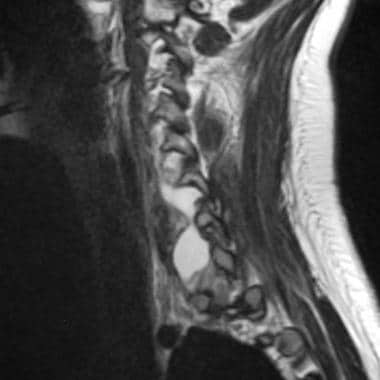
 Brachial plexus injury. Birth trauma. Sagittal image of the brachial plexus shows an area of increased signal intensity in the C6 neural foramen. This is an area of particular concern in cases of birth trauma, and the finding is consistent with traumatic injury of the nerve root.
Brachial plexus injury. Birth trauma. Sagittal image of the brachial plexus shows an area of increased signal intensity in the C6 neural foramen. This is an area of particular concern in cases of birth trauma, and the finding is consistent with traumatic injury of the nerve root.
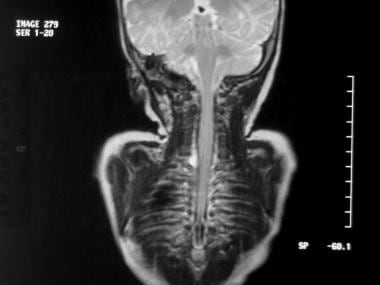 Brachial plexus injury. Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.
Brachial plexus injury. Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.
 Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Oblique cervical myelogram shows extravasation of contrast material from torn right lower nerve-root sheaths.
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Oblique cervical myelogram shows extravasation of contrast material from torn right lower nerve-root sheaths.
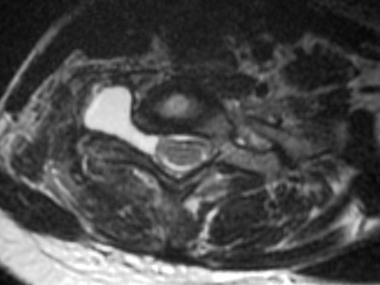
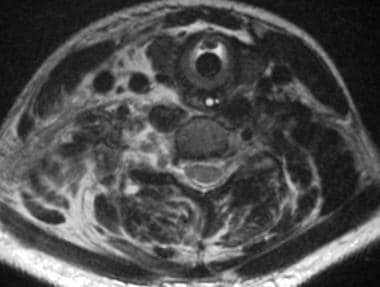 Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Axial image obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive injuries to the right paraspinal soft tissues. The 3 images immediately following this one were obtained 3 months after this image was produced.
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Axial image obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive injuries to the right paraspinal soft tissues. The 3 images immediately following this one were obtained 3 months after this image was produced.
 Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Coronal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve-root sheaths and avulsed nerve roots.
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Coronal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve-root sheaths and avulsed nerve roots.
 Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Sagittal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve-root sheaths and avulsed nerve roots.
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Sagittal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve-root sheaths and avulsed nerve roots.
 Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Axial image obtained with a long repetition time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve root sheaths and avulsed nerve roots.
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Axial image obtained with a long repetition time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve root sheaths and avulsed nerve roots.
Technique and Imaging Parameters
The brachial plexus can be identified on MRI by first identifying the anterior scalene muscle. The brachial plexus and subclavian artery (relationship outlined above) are deep to the anterior scalene. The roots are best seen on axial images, whereas the remaining components are seen well on coronal and sagittal images.
Normal components of the brachial plexus have intermediate-to-low signal intensity on images obtained with all sequences and are surrounded by fat. Conversely, abnormal nerves may demonstrate focal or diffuse enlargement, deviation, discontinuity, elevated T2-weighted signal, and/or effacement of the perineural fat planes. Segmental or confluent postcontrast enhancement of the brachial plexus can also be visualized in the setting of infiltrative tumor or infection. [14, 34, 35]
(See the images below.)
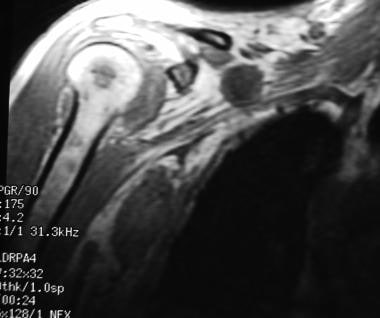 Brachial plexus injury. Non-Hodgkin lymphoma in a 58-year-old man. Coronal spoiled gradient-echo image (repetition time [TR]/echo time [TE], 175/4.2 ms; flip angle, 90°) shows lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
Brachial plexus injury. Non-Hodgkin lymphoma in a 58-year-old man. Coronal spoiled gradient-echo image (repetition time [TR]/echo time [TE], 175/4.2 ms; flip angle, 90°) shows lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
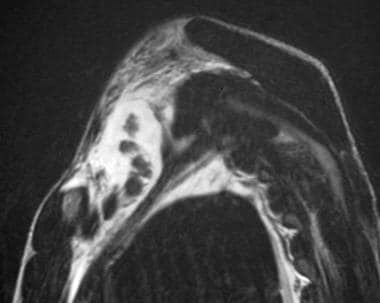
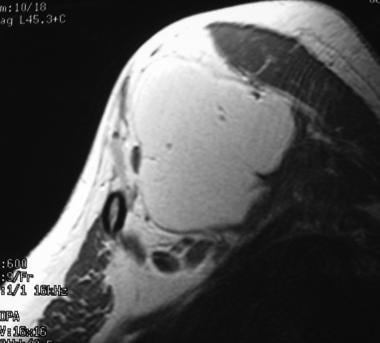
 Brachial plexus injury. Non-Hodgkin lymphoma. Axial image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 550/9 ms) shows lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
Brachial plexus injury. Non-Hodgkin lymphoma. Axial image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 550/9 ms) shows lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
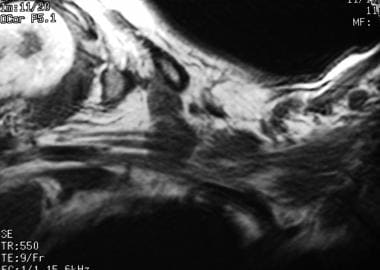
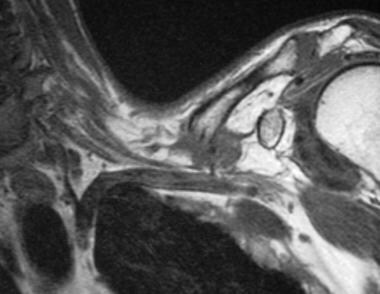
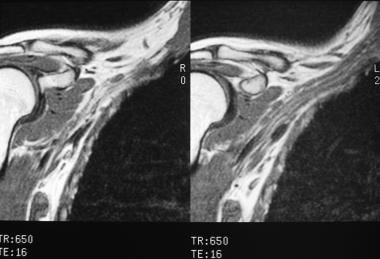
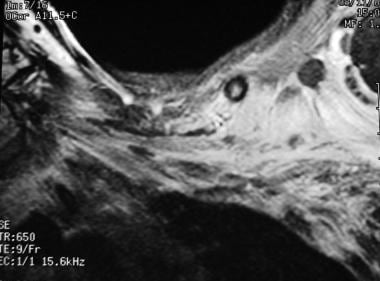
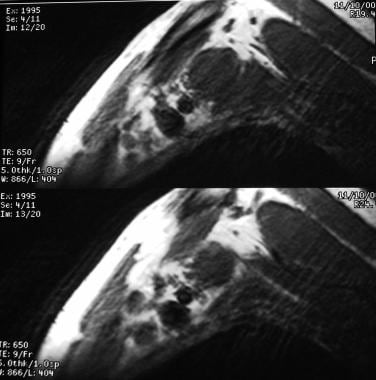 Brachial plexus injury. Non-Hodgkin lymphoma in a 58-year-old man. Sagittal images obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) show lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
Brachial plexus injury. Non-Hodgkin lymphoma in a 58-year-old man. Sagittal images obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) show lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
A variety of MRI protocols and techniques have been described in the evaluation of the brachial plexus. Described are the general protocols used at the authors’ institution to best satisfy the needs of patients and clinicians; these protocols are tailored as needed.
Radiofrequency coil
A surface coil provides resolution higher than that of a body coil, but it increases artifact due to respiratory motion. A combination of each may be used in sequences for the brachial plexus. As such, the surface coil is used for the spinal cord and exiting spinal nerve roots, whereas the body coil is used to image the plexus lateral to the interscalene triangle.
Field of view
Examination of the brachial plexus begins with the roots and trucks in the proximal aspects within the supraclavicular region and continues to the origin of the terminal branches at the lateral margin of the pectoralis minor muscle in the infraclavicular region.
The field of view (FOV) is 17-22 cm for the direct coronal orientation and 14-17 cm for sagittal or oblique sagittal orientations.
Matrix
A matrix of 512 X 256 or 512 X 512 is used.
Section thickness
The recommended section thickness is 3-4 mm, with an intersection gap of 0-0.5 mm for direct coronal imaging and 4-5 mm with an intersection gap of 1-2 mm for sagittal or oblique sagittal imaging. If axial images are obtained, 4-mm thickness with a 1- to 1.5-mm intersection gap may be performed.
Orientation
Images should be obtained in at least 2 planes. Direct coronal plane imaging is preferred over oblique coronal imaging, because the brachial plexus has a shallow obliquity relative to the true coronal plane and because it can be imaged on 1 or 2 coronal sections.
Cross-sectional imaging of the nerve components of the plexus may be performed by using either the true sagittal or the oblique sagittal plane on the side of interest. True sagittal imaging allows for comparison with the standard cross-sectional anatomy, which some find helpful in the recognition of appropriate anatomic landmarks. However, oblique sagittal imaging more accurately represents the true cross-section of the brachial plexus than true sagittal imaging and thus allows for increased sensitivity to pathology, including changes in caliber, alteration in signal intensity, or presence of a fascicular pattern to the nerve components.
Contrast
Thin-section axial, coronal, and sagittal contrast-enhanced T1-weighted sequences with or without fat suppression can be helpful in the evaluation of tumor, infection, or stretch injury. Some institutions include a contrast-enhanced T1-weighted axial sequence as part of their routine evaluation of the brachial plexus.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MR angiography scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Pulse sequences
T1- and T2-weighted images are obtained with identical parameters in terms of FOV, matrix, section thickness, and imaging plane.
STIR or frequency-selective fat-saturation methods may be used for T2-weighted MRI to increase the conspicuity of abnormal signal intensity from the signal intensity of adjacent fat. Each has its advantages and disadvantages. STIR has been described as being more reliable than the other method because of its uniform and consistent fat suppression and excellent T2-like contrast when long repetition times are used.
The STIR method has several disadvantages. For example, it has a relatively low signal-to-noise ratio, it offers relatively low tissue contrast, and it is more susceptible to flow artifacts than other methods.
In contrast, frequency-selective fat-saturation methods have the advantage of an improved signal-to-noise ratio, T1-weighted imaging, and reduced flow-related artifacts. The major disadvantage of this type of fat suppression is the nonuniformity of fat suppression with the FOV primarily from inhomogeneity of B0. This variability in fat suppression is exacerbated by the nonuniformity in B1.
When radiation injury, neoplasm, stretch injury, infection, or inflammatory etiologies are present or suspected, contrast-enhanced fat-suppressed T1-weighted MRI should be performed. The suggested protocol is summarized in the images below.
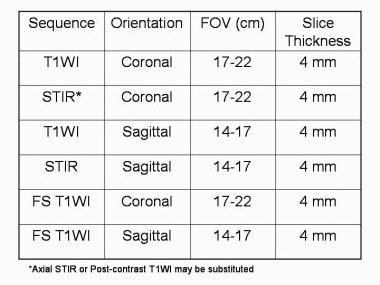 Brachial plexus injury. Summary of suggested MRI techniques. FOV = field of view; T1WI = T1-weighted imaging; STIR = short-tau inversion recovery; FS = fast spin echo.
Brachial plexus injury. Summary of suggested MRI techniques. FOV = field of view; T1WI = T1-weighted imaging; STIR = short-tau inversion recovery; FS = fast spin echo.
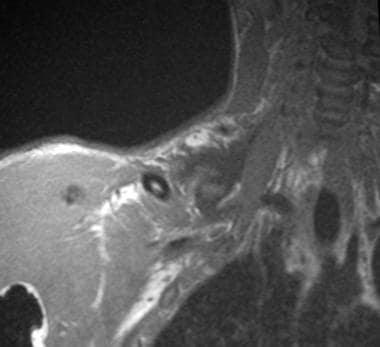 Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Coronal image obtain with a short repetition time (TR) and a short echo time (TE) (TR/TE, 600/8 ms) shows a poorly defined zone of low signal intensity in the region of the right brachial plexus.
Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Coronal image obtain with a short repetition time (TR) and a short echo time (TE) (TR/TE, 600/8 ms) shows a poorly defined zone of low signal intensity in the region of the right brachial plexus.
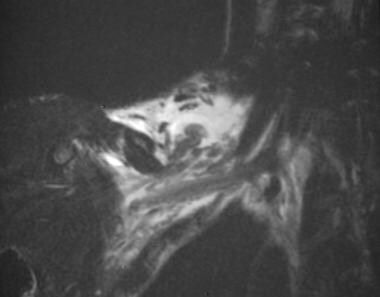 Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Coronal image obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 7058/98 ms) shows a traumatic fluid collection containing several retracted nerves of the right brachial plexus.
Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Coronal image obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 7058/98 ms) shows a traumatic fluid collection containing several retracted nerves of the right brachial plexus.
 Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Sagittal image obtained a long repetition time (TR) and long echo time (TE) (TR/TE, 10,588/98 ms) shows a traumatic fluid collection containing several retracted nerves of the right brachial plexus.
Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Sagittal image obtained a long repetition time (TR) and long echo time (TE) (TR/TE, 10,588/98 ms) shows a traumatic fluid collection containing several retracted nerves of the right brachial plexus.
 Brachial plexus injury. Clavicular fracture in a 57-year-old man with a traumatic comminuted fracture of the left clavicle. Coronal image obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 600/9 ms) shows the fracture mildly impressing on the left brachial plexus.
Brachial plexus injury. Clavicular fracture in a 57-year-old man with a traumatic comminuted fracture of the left clavicle. Coronal image obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 600/9 ms) shows the fracture mildly impressing on the left brachial plexus.
 Brachial plexus injury. Clavicular fracture in a 57-year-old man with a traumatic comminuted fracture of the left clavicle. Sagittal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 2000/83 ms) shows the fracture mildly impressing on the left brachial plexus.
Brachial plexus injury. Clavicular fracture in a 57-year-old man with a traumatic comminuted fracture of the left clavicle. Sagittal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 2000/83 ms) shows the fracture mildly impressing on the left brachial plexus.
 Brachial plexus injury. Lipoma in a 38-year-old woman with a lipoma above the left brachial plexus. Coronal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left brachial plexus.
Brachial plexus injury. Lipoma in a 38-year-old woman with a lipoma above the left brachial plexus. Coronal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left brachial plexus.
 Brachial plexus injury. Lipoma in a 38-year-old woman with a lipoma above the left brachial plexus. Sagittal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left brachial plexus.
Brachial plexus injury. Lipoma in a 38-year-old woman with a lipoma above the left brachial plexus. Sagittal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left brachial plexus.
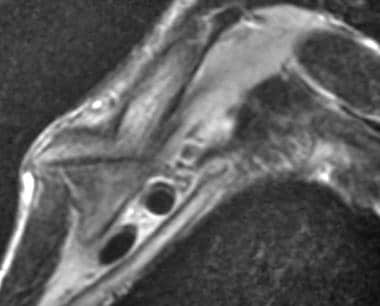
 Brachial plexus injury. Neurofibromatosis type 1 in a 26-year-old woman. Coronal images obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE 650/16 ms) show several circumscribed neurofibromas along the right brachial plexus.
Brachial plexus injury. Neurofibromatosis type 1 in a 26-year-old woman. Coronal images obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE 650/16 ms) show several circumscribed neurofibromas along the right brachial plexus.
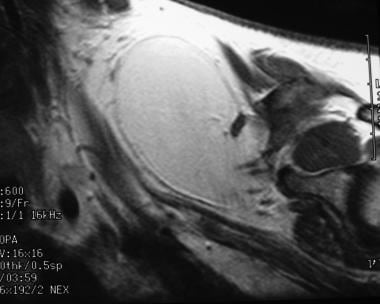
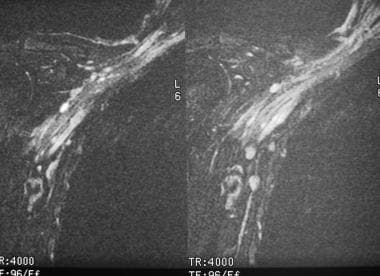 Brachial plexus injury. Neurofibromatosis type 1 in a 26-year-old woman. Coronal fat-suppressed images obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 4000/96 ms) show several circumscribed neurofibromas along the right brachial plexus. The neurofibromas have high signal intensity.
Brachial plexus injury. Neurofibromatosis type 1 in a 26-year-old woman. Coronal fat-suppressed images obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 4000/96 ms) show several circumscribed neurofibromas along the right brachial plexus. The neurofibromas have high signal intensity.
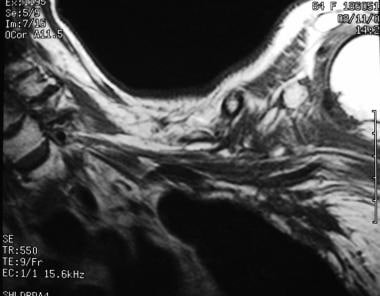 Brachial plexus injury. Postirradiation changes in an 84-year-old woman with a history of breast cancer. Coronal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 400/9 ms) shows irregular thickening of the left brachial plexus.
Brachial plexus injury. Postirradiation changes in an 84-year-old woman with a history of breast cancer. Coronal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 400/9 ms) shows irregular thickening of the left brachial plexus.
 Brachial plexus injury. Postirradiation changes in an 84-year-old with a history of breast cancer. Coronal contrast-enhanced fat-suppressed image obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) shows poorly defined zones of contrast enhancement in the region of the brachial plexus. These zones representing radiation-induced changes to infiltrating tumor.
Brachial plexus injury. Postirradiation changes in an 84-year-old with a history of breast cancer. Coronal contrast-enhanced fat-suppressed image obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) shows poorly defined zones of contrast enhancement in the region of the brachial plexus. These zones representing radiation-induced changes to infiltrating tumor.
-
Brachial plexus injury. Diagram of the brachial plexus.
-
Brachial plexus injury. Summary of suggested MRI techniques. FOV = field of view; T1WI = T1-weighted imaging; STIR = short-tau inversion recovery; FS = fast spin echo.
-
Brachial plexus injury. Birth trauma. Sagittal image of the brachial plexus shows an area of increased signal intensity in the C6 neural foramen. This is an area of particular concern in cases of birth trauma, and the finding is consistent with traumatic injury of the nerve root.
-
Brachial plexus injury. Birth trauma. Coronal image of the brachial plexus shows an area of increased signal intensity in the right C6 neural foramen.
-
Brachial plexus injury. Birth trauma.
-
Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Coronal image obtain with a short repetition time (TR) and a short echo time (TE) (TR/TE, 600/8 ms) shows a poorly defined zone of low signal intensity in the region of the right brachial plexus.
-
Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Coronal image obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 7058/98 ms) shows a traumatic fluid collection containing several retracted nerves of the right brachial plexus.
-
Brachial plexus injury. Avulsion in a 15-year-old male adolescent with palsy of the right upper extremity due to trauma related to a snowmobile accident. Sagittal image obtained a long repetition time (TR) and long echo time (TE) (TR/TE, 10,588/98 ms) shows a traumatic fluid collection containing several retracted nerves of the right brachial plexus.
-
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Oblique cervical myelogram shows extravasation of contrast material from torn right lower nerve-root sheaths.
-
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Axial image obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 3800/98 ms) shows extensive injuries to the right paraspinal soft tissues. The 3 images immediately following this one were obtained 3 months after this image was produced.
-
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Coronal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 1800/71 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve-root sheaths and avulsed nerve roots.
-
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Sagittal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 1800/112 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve-root sheaths and avulsed nerve roots.
-
Brachial plexus injury. Avulsion in a 17-year-old female adolescent after she was ejected from an automobile in a collision. Axial image obtained with a long repetition time (TR) and long echo time TE (TR/TE, 4000/100 ms) shows circumscribed right paravertebral fluid collections at C6-7 and C7-T1. These represent pseudomeningoceles from torn nerve root sheaths and avulsed nerve roots.
-
Brachial plexus injury. Clavicular fracture in a 57-year-old man with a traumatic comminuted fracture of the left clavicle. Coronal image obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 600/9 ms) shows the fracture mildly impressing on the left brachial plexus.
-
Brachial plexus injury. Clavicular fracture in a 57-year-old man with a traumatic comminuted fracture of the left clavicle. Sagittal image obtained with a long repetition time (TR) and long echo time (TE) (TR/TE, 2000/83 ms) shows the fracture mildly impressing on the left brachial plexus.
-
Brachial plexus injury. Lipoma in a 38-year-old woman with a lipoma above the left brachial plexus. Coronal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left brachial plexus.
-
Brachial plexus injury. Lipoma in a 38-year-old woman with a lipoma above the left brachial plexus. Sagittal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 600/9 ms) shows a lipoma mildly impressing on the left brachial plexus.
-
Brachial plexus injury. Non-Hodgkin lymphoma in a 58-year-old man. Coronal spoiled gradient-echo image (repetition time [TR]/echo time [TE], 175/4.2 ms; flip angle, 90°) shows lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
-
Brachial plexus injury. Non-Hodgkin lymphoma. Axial image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 550/9 ms) shows lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
-
Brachial plexus injury. Non-Hodgkin lymphoma in a 58-year-old man. Sagittal images obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) show lymphomatous lesions in the right brachial plexus and in the marrow of the humerus.
-
Brachial plexus injury. Neurofibromatosis type 1 in a 26-year-old woman. Coronal images obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE 650/16 ms) show several circumscribed neurofibromas along the right brachial plexus.
-
Brachial plexus injury. Neurofibromatosis type 1 in a 26-year-old woman. Coronal fat-suppressed images obtained with a long repetition time (TR) and a long echo time (TE) (TR/TE, 4000/96 ms) show several circumscribed neurofibromas along the right brachial plexus. The neurofibromas have high signal intensity.
-
Brachial plexus injury. Postirradiation changes in an 84-year-old woman with a history of breast cancer. Coronal image obtained with a short repetition time (TR) and short echo time (TE) (TR/TE, 400/9 ms) shows irregular thickening of the left brachial plexus.
-
Brachial plexus injury. Postirradiation changes in an 84-year-old with a history of breast cancer. Coronal contrast-enhanced fat-suppressed image obtained with a short repetition time (TR) and a short echo time (TE) (TR/TE, 650/9 ms) shows poorly defined zones of contrast enhancement in the region of the brachial plexus. These zones representing radiation-induced changes to infiltrating tumor.