Practice Essentials
The routine use of ultrasonography has created a safe, reliable, and repeatable method of measuring amniotic fluid volume (AFV). The 2 most commonly used objective methods of determining AFV include measurement of the single deepest pocket (SDP) and the summation of the SDPs in each quadrant, or the amniotic fluid index (AFI). Amniotic fluid is necessary for the proper growth and development of the fetus, cushioning it from physical trauma, allowing fetal lung growth, and providing a barrier against infection. An inadequate volume of amniotic fluid, called oligohydramnios, results in poor development of the lung tissue and can lead to fetal death. [1, 2, 3, 4, 5, 6]
Normally, the volume of amniotic fluid changes over the course of gestation, increasing up until 34 to 36 weeks and then leveling off, at approximately 400mL, and remaining constant until term. After 40 weeks, the AFV begins to decrease steadily. [5, 6]
The earlier in pregnancy that oligohydramnios occurs, the poorer the prognosis. Fetal mortality rates as high as 80-90% have been reported with oligohydramnios diagnosed in the second trimester. Most of this mortality is a result of major congenital malformations and pulmonary hypoplasia secondary to PROM (premature rupture of membranes) before 22 weeks' gestation. Midtrimester PROM often leads to pulmonary hypoplasia, fetal compression syndrome, and amniotic band syndrome. The inspiration of amniotic fluid at regular intervals is probably needed for terminal alveolar development. [1, 7, 8, 9] Maternal diabetes mellitus increases the risk for oligohydramnios (P = 0.005). [10, 11]
Oligohydramnios is characterized by the following features:
-
Diminished amniotic fluid volume (AFV)
-
Amniotic fluid volume of less than 500 mL at 32-36 weeks' gestation: Amniotic fluid volume depends on the gestational age; therefore, the best definition may be AFI less than the fifth percentile.
-
Single deepest pocket (SDP) of less than 2 cm
-
Amniotic fluid index (AFI) of less than 5 cm or less than the fifth percentile
(See the images below.)
 Sonogram obtained before second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
Sonogram obtained before second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
 Sonogram obtained after second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
Sonogram obtained after second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
The assessment of amniotic fluid volume is important in pregnancies complicated by abnormal fetal growth or intrauterine growth restriction (IUGR). AFV has been shown to be predictive in discriminating normal from decreased growth. Oligohydramnios is a frequent finding in pregnancies involving IUGR and is most likely secondary to decreased fetal blood volume, renal blood flow, and, subsequently, fetal urine output. Pregnancies complicated by severe oligohydramnios have been shown to be at increased risk for fetal morbidity. [12, 13]
AFV is an important predictor of fetal well-being in pregnancies beyond 40 weeks' gestation. AFV must be closely monitored, with measurements obtained at least once per week. The diagnosis of oligohydramnios may help in identifying postterm fetuses in jeopardy.
AFV is a predictor of the fetal tolerance of labor, and it is associated with an increased risk of abnormal heart rate, meconium-stained amniotic fluid, and cesarean delivery. An increased incidence of cord compression is associated with oligohydramnios; this can lead to variable decelerations, with cord occlusion as the proximate cause of fetal distress.
According to one study, pregnancies with decreased AFI between 24 and 34 weeks, including borderline AFI and oligohydramnios, were significantly more likely to be associated with major fetal malformations and, in the absence of malformations, to be complicated by fetal growth restriction and preterm birth. Major malformations were more common in pregnancies with oligohydramnios (25%) and borderline AFI (10%) than in those with normal fluid (2%). [14]
Long-term neurologic morbidity is more common in children of oligohydramnios-complicated pregnancies. Higher rates of pervasive developmental disorder, movement disorders, developmental disorders, and degenerative and demyelization disorders have been reported. [15]
Hydration (intravenous and oral) has been found to significantly improve the volume of amniotic fluid in third-trimester pregnancies with isolated oligohydramnios. [16] For more information, see Polyhydramnios and Oligohydramnios.
Workup
Ultrasonography
The diagnosis of oligohydramnios is confirmed by means of ultrasonography (see the images below). Oligohydramnios may be discovered incidentally during routine ultrasonography and noted during antepartum surveillance for other conditions. The diagnosis may be prompted by a lag in sequential fundal height measurements (size less than that expected for the dates) or by fetal parts that are easily palpated through the maternal abdomen. [17, 18, 19, 20, 21, 22]
During ultrasonography of the fetal anatomy, normal-appearing fetal kidneys and fluid-filled bladder may be observed to rule out renal agenesis (see the following 2 images), cystic dysplasia, and ureteral obstruction. Check fetal growth to rule out intrauterine growth restriction (IUGR) leading to oliguria.
 Sonogram obtained before second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
Sonogram obtained before second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
 Sonogram obtained after second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
Sonogram obtained after second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
Sterile speculum examination
Sterile speculum examination may be performed to check for range of motion (ROM). Amniotic fluid may pool in the vagina, and an arborization or ferning pattern may be observed when dried posterior vault fluid is examined microscopically. Cervical mucous may cause false-positive results, as can semen and blood. Nitrazine paper turns blue. The amniotic fluid is more basic (pH 6.5-7.0) than normal vaginal discharge (pH 4.5).
Measurement of amniotic fluid volume
Initial studies to objectively measure amniotic fluid volume (AFV) involved dye dilution techniques. The techniques were accurate, although they required amniocentesis, an invasive procedure that increased the risk of perinatal morbidity. The routine use of ultrasonography has created a safe, reliable, and repeatable method of measuring AFV. Early methods of assessing AFV with ultrasonography involved nonquantitative assessments, including sonographers' subjective impression of AFV.
Subjective oligohydramnios criteria have included the following:
-
The absence of fluid pockets throughout the uterine cavity
-
Crowding of the fetal limbs
-
The absence of pockets surrounding the fetal legs
-
Overlapping of the fetal ribs (in severe cases)
The 2 most commonly used objective methods of determining AFV include measurement of the single deepest pocket (SDP) and the summation of the SDPs in each quadrant, or the amniotic fluid index (AFI). [4] These tests are routinely performed with the patient in the supine or semi-Fowler position, although studies have demonstrated accuracy in the lateral decubitus position as well. [13, 23, 24, 25, 26, 27]
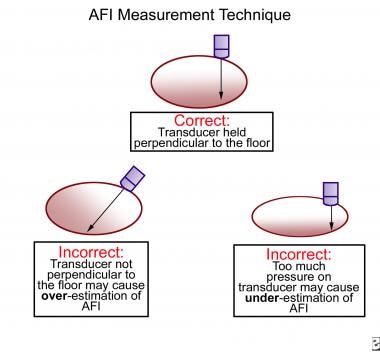
The ultrasound transducer is held along the maternal longitudinal axis and maintained perpendicular to the floor while the SDP of the amniotic fluid is measured. Pockets should be free of fetal limbs and the umbilical cord, although some authors allow for a single loop of cord to be within the fluid pocket. AFV may be artificially increased if the transducer is not maintained perpendicular to the floor. Excessive pressure on the maternal abdomen with the transducer may lead to an artificially reduced measurement (see the image below).
Phelan et al described the AFI as a quantitative measurement to predict a poor pregnancy outcome and the success of external cephalic versions. [28] The pregnant abdomen is divided into 4 quadrants by using the umbilicus as a reference point to divide the uterus into upper and lower halves and by using the linea nigra to divide the uterus into left and right halves. The 4 measurements are summed to obtain the AFI in centimeters. [24, 25]
In gestations earlier than 20 weeks, measurements from the 2 halves are divided by the linea nigra to obtain the AFI. Tables of the normal limits for AFI, based on the gestational age (see the Gestational Age from Estimated Date of Delivery calculator), have been published for singleton and multiple pregnancies (see an example below). The mean AFI for normal pregnancies is 11-16 cm.
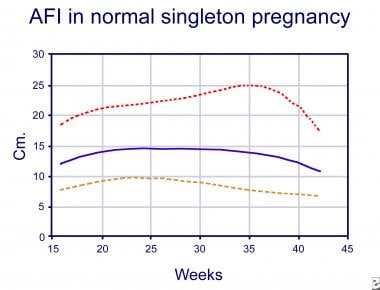 Amniotic fluid index (AFI) during a normal human singleton pregnancy. The solid line is the mean AFI, the lower dotted line is the 5th percentile value, and the upper dotted line is the 95th percentile value (data adapted from Moore, 1990). Image courtesy of Christopher L. Sistrom, MD.
Amniotic fluid index (AFI) during a normal human singleton pregnancy. The solid line is the mean AFI, the lower dotted line is the 5th percentile value, and the upper dotted line is the 95th percentile value (data adapted from Moore, 1990). Image courtesy of Christopher L. Sistrom, MD.
The test is reproducible, with interobserver and intraobserver variations of about 10-15% or 1-2 cm in pregnancies with normal AFVs. The margin of error is less in patients with decreased amounts of amniotic fluid.
Oligohydramnios has been defined as an amniotic fluid index (AFI) less than 5 cm, although 8 cm has occasionally been used as a cut-off threshold. Because the AFV depends on the gestational age, oligohydramnios has been defined as an AFI less than the fifth percentile (corresponding to an AFI of < 6.8 cm at term).
Oligohydramnios has been defined as an SDP less than 2 cm. Perinatal morbidity rates have been shown to increase sharply with SDPs below this value. Some have suggested that an SDP of 2.5-3.0 cm is a better lower limit for separating normal SDPs from those consistent with oligohydramnios.
Many studies have shown that the SDP and the AFI methods have equal diagnostic accuracies, with reported sensitivity greater than 90%. [2] The SDP technique may be a better means of assessing the AFV in twin gestations and in pregnancies at an early gestational age. Some study results have shown that the AFI has greater sensitivity and a higher predictive value than the SDP in diagnosing abnormally high and low AFVs. Most obstetricians prefer to assess a broader area of the uterine cavity by using the AFI because the single measurement of the SDP does not allow for an asymmetric fetal position in the uterus.
According to a survey of members of the Society of Maternal-Fetal Medicine, deepest vertical pocket is considered to be the most accurate method of evaluating amniotic fluid in the second trimester, and amniotic fluid index is considered to be the most accurate method of evaluating fluid in the third trimester. Over 50% of respondents felt that oligohydramnios is overdiagnosed when using amniotic fluid index compared with deepest vertical pocket. [29]
Other examinations
MRI and 3-dimensional (3D) ultrasonography are newer (and more expensive) modalities for accurately assessing the AFV. [30, 31, 3]
Fetal MRI can complement ultrasonography by providing better visualization in the fetus when ultrasound may be limited, in cases such as severe maternal obesity. Although MRI may offer a larger field of view and better tissue contrast and not be limited by shadowing from osseous structures, it has a limited resolution when compared with ultrasonography and is less readily available and is more expensive. [3]
In 35 women with healthy singleton pregnancies, rapid MRI-based projection hydrography (PH) measurement was found to be a better predictor of amniotic fluid volume than ultrasonography (in utero at 28-32 weeks’ gestation). For the ultrasound measurements, single deepest vertical pocket (SDVP) measurement related most closely to amniotic fluid volume, with amniotic fluid index (AFI) demonstrating a weaker relationship. Manual multisection planimetry (MSP)-based measurement of AFV was used as a proxy reference standard. [31]
Amniotic wrinkle
Finberg reported a possible pitfall in the sonographic analysis of amniotic fluid in twin pregnancies, the "amniotic wrinkle," which may give the misleading impression of adequate amniotic fluid for both twins when one twin actually has little to none.
The author reevaluated sonograms of twin pregnancies in which an initial sonographer's assessment was adequate fluid for each twin but which the author's own imaging assessment on the same day showed oligohydramnios in one twin. He found either of the following may occur when oligohydramnios of one twin is present:
-
The intertwin membrane may fold in on itself, creating an amniotic wrinkle (a short linear structure that extends perpendicularly away from the twin with decreased amniotic fluid in toward the amniotic space of the other twin)
-
An intrauterine sling or "cocoon" may be present, in which a fetus appears to be suspended within the amniotic space of the other twin
Finberg recommended showing the intertwin membrane in all images used to document each twin's amniotic fluid, with additional right-angle images to identify amniotic wrinkles. [32]
-
Sonogram obtained before second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
-
Sonogram obtained after second-trimester amnioinfusion. This fetus has bilaterally absent kidneys consistent with a diagnosis of Potter syndrome. The cystic structures in the renal fossae are most likely the adrenal glands.
-
Amniotic fluid index (AFI) during a normal human singleton pregnancy. The solid line is the mean AFI, the lower dotted line is the 5th percentile value, and the upper dotted line is the 95th percentile value (data adapted from Moore, 1990). Image courtesy of Christopher L. Sistrom, MD.
-
Amniotic fluid index (AFI) measurement technique.