Practice Essentials
In 1840, Rayer first described the association between renal vein thrombosis (RVT) and nephrotic syndrome. Earlier reports, from postmortem examinations, had correctly cited infectious suppuration, malignancy, and trauma as likely causes of RVT. [1] However, since Rayer's time—as increased awareness and better radiographic techniques have helped physicians gain a greater understanding of the etiology, characteristics, and treatment of RVT—nephrotic syndrome has been identified as the most frequent cause. [2, 3, 4, 5, 6]
On the basis of early descriptions, researchers initially believed that RVT always produced such acute symptoms as flank pain, edema, and a lumbar mass. However, the classic presentations of the condition—nephrotic syndrome and lower abdominal and flank pain in adults and renal failure and a painful, palpable mass in infants—are only 2 extremes of RVT's clinical spectrum. [7] Currently, most patients with RVT present only with nephrotic syndrome in the absence of other symptoms. In addition, although the incidence of RVT is relatively high, most patients remain asymptomatic for it, and spontaneous recovery occurs more frequently than is suggested clinically. [8]
Cases of renal vein thrombosis and pulmonary embolism have been reported in patients with COVID-19. [9, 10]
Ultrasonography (US), computed tomography (CT) scanning, and magnetic resonance imaging (MRI) have varying levels of sensitivity and specificity. [11] US is often the initial noninvasive study of choice to exclude the presence of RVT. [2] Observations suggest that when US findings are equivocal, magnetic resonance angiography (MRA) is a useful and accurate alternative test for RVT before venography. [12, 13] CT angiography can demonstrate thrombus in the renal vein and, at times, in the vena cava. [3] Renal venography remains the diagnostic gold standard but is an invasive procedure.
(Radiologic characteristics of RVT are demonstrated in the images below.)
 Inferior cavography demonstrates thrombus extending from the left renal vein into the inferior vena cava.
Inferior cavography demonstrates thrombus extending from the left renal vein into the inferior vena cava.
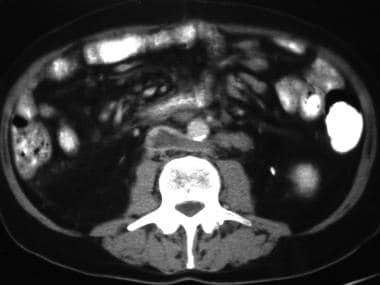 CT reveals thrombus extending from the left renal vein into the inferior vena cava. Note that the left renal vein is retroaortic.
CT reveals thrombus extending from the left renal vein into the inferior vena cava. Note that the left renal vein is retroaortic.
Diagnosis
Because the classic presentation of hematuria, flank pain, and a lumbar mass is rarely seen in RVT, a high index of suspicion is essential for the condition's diagnosis. Ultrasonography (US), computed tomography (CT) scanning, and magnetic resonance imaging (MRI) have varying levels of sensitivity and specificity. [14, 15, 16, 17]
Ultrasonography
US is the initial study of choice to exclude the presence of RVT. In an acute setting, US may reveal an edematous and enlarged kidney with decreased echogenicity caused by diffuse edema, as well as focal or diffuse disruption of parenchymal architecture and/or thrombus in the renal veins. [18, 11]
Duplex Doppler US demonstrates peaked, abruptly decreasing systolic-frequency shifts and retrograde plateaulike shifts during diastole at the level of the main renal artery and its proximal branches, with an absent venous signal. [19] Doppler US may reveal increased blood velocity and turbulence in narrowed sections of the renal vein or cessation of blood flow if the lumen is completely obstructed. Power Doppler US has increased confidence in the diagnosis of RVT and in the assessment of caval tumor thrombus. [20]
In one study, color Doppler US was found to be useful for diagnosis of large renal infarcts caused by thrombosis or embolism in the main renal artery; however, small infarcts could be missed by color Doppler US, necessitating other imaging modalities for confirmation. [15]
Computed tomography
CT findings include decreased nephrographic attenuation, loss of corticomedullary differentiation, a low-attenuating thrombus in the renal vein, renal enlargement with persistent parenchymal opacification, and renal vein enlargement. [21, 22] In the acute stage of RVT, capsular venous collaterals, thickening of the Gerota fascia, and pericapsular whiskering also are often observed. [23]
(See the image below.)
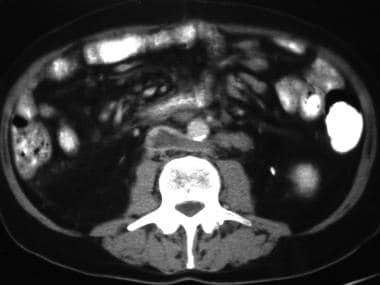 CT reveals thrombus extending from the left renal vein into the inferior vena cava. Note that the left renal vein is retroaortic.
CT reveals thrombus extending from the left renal vein into the inferior vena cava. Note that the left renal vein is retroaortic.
Magnetic resonance angiography
Observations suggest that when US findings are equivocal, magnetic resonance angiography (MRA) is a useful and accurate alternative test for RVT before venography. MRA provides high contrast between flowing blood, vascular walls, and surrounding tissues. Other advantages include the avoidance of contrast material, noninvasiveness, and the ability to image the arterial and venous phases. Preliminary observations indicate that MRI and/or MRA may be the diagnostic procedures of choice for RVT detection. [12, 13]
Renal venography and renal arteriography
Currently, renal venography remains the diagnostic criterion standard. Assessing the venous phase of renal arteriography also aids in diagnosis. However, both are invasive procedures and, unlike US and MRA, require the use of potentially nephrotoxic contrast agents even in patients with existing renal compromise.
In a study of patients with nephrotic syndrome, CT venography found that RVT was present in 112 of 505 patients (22%). The authors noted that a high index of suspicion and a low threshold for diagnostic workup is warranted in these patients. Membranous nephropathy, age greater than 60 years, high hemoglobin level, long prothrombin time, and high creatinine level were independent predictors. [23]
Radionuclide renography
Radionuclide renography using technetium-99m–diethylenetriaminepentaacetic acid has proven to be useful in the assessment of renal perfusion. Organ damage in acute RVT results primarily from arterial compromise caused by venous pressure elevations. In such cases, scintigraphy reveals delayed or absent perfusion to the kidney. When a scan indicates perfusion arrest, an aggressive therapeutic approach may be warranted. [24]
-
Inferior cavography demonstrates thrombus extending from the left renal vein into the inferior vena cava.
-
CT reveals thrombus extending from the left renal vein into the inferior vena cava. Note that the left renal vein is retroaortic.








