Practice Essentials
The role of interventional radiologists in trauma cases has evolved from that of making the initial diagnosis of vascular and solid organ injuries to that of temporizing or definitive treatment. The American College of Surgeons Committee on Trauma has recommended that an interventional radiologist be available within 30 minutes to perform procedures in all level I and level II trauma centers. [1] The Society of Interventional Radiology (SIR) has published the following recommendations [2] :
-
Emergent thoracic endovascular aortic repair (TEVAR) should be used in anatomically favorable grade 3 and grade 4 aortic injuries, with nonoperative management (antihypertensive and antiimpulse medication with close symptomatic and/or radiographic follow-up) favored for grade 1 and grade 2 injuries.
-
For pelvic trauma, embolization should be first-line therapy. When the clinical condition permits, contrast-enhanced CT should be pursued because it is the most sensitive and specific test to identify the source of arterial bleeding in the pelvis.
-
Nonoperative management is becoming the treatment of choice for patients with blunt hepatic injury who are hemodynamically stable, resulting in decreased abdominal infections, transfusions, and length of hospital stay. Embolization should be considered in cases of ongoing bleeding, to identify an arterial source of bleeding on imaging, or when there is suspicion of a persistent source of arterial bleeding despite operative intervention.
-
Splenic artery embolization should be considered in hemodynamically stable patients with grade IV/V blunt splenic trauma or with any grade injury who have imaging or clinical evidence of splenic hemorrhage.
-
Angiography and embolization should be considered in patients with grade III/IV renal injuries when surgical exploration is not warranted.
Many technical innovations in imaging and angiographic equipment, as well as new developments in transcatheter therapy, have paved the way for this trend in nonoperative management, including the following [3, 4, 5, 6, 7, 8, 9, 10, 11] :
-
State-of-the-art digital subtraction angiography
-
Helical CT
-
Microcatheters, steerable and hydrophilic guidewires, and coaxial guiding catheters and sheaths
-
Novel embolization materials and delivery systems
-
Stents and covered stents (stent-grafts)
(Images of vascular and solid organ trauma are shown below.)
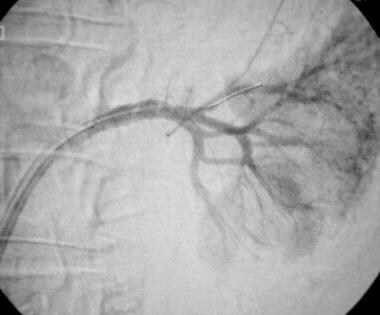
 Digital subtraction catheter aortogram (late phase) of a typical acute traumatic aortic injury (same patient as in the previous image).
Digital subtraction catheter aortogram (late phase) of a typical acute traumatic aortic injury (same patient as in the previous image).
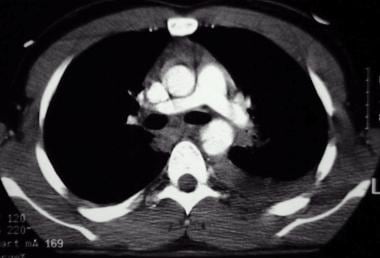
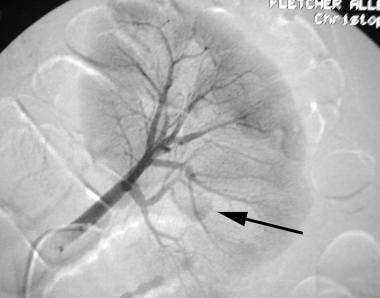
 Vascular and solid organ trauma. Contrast-enhanced CT of the abdomen in a hemodynamically stable patient with evidence of persistent hemorrhage following a motor vehicle accident. Arrow points to contrast extravasation in a lacerated spleen (Courtesy of the Society of Cardiovascular and Interventional Radiology).
Vascular and solid organ trauma. Contrast-enhanced CT of the abdomen in a hemodynamically stable patient with evidence of persistent hemorrhage following a motor vehicle accident. Arrow points to contrast extravasation in a lacerated spleen (Courtesy of the Society of Cardiovascular and Interventional Radiology).
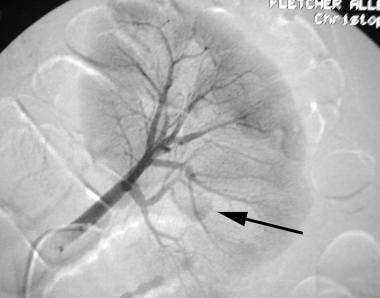
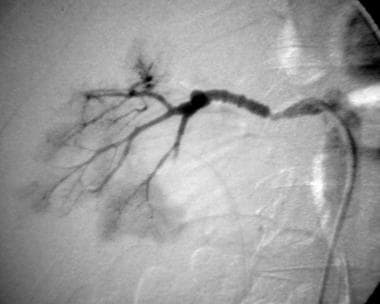
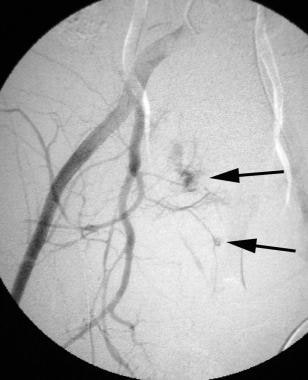
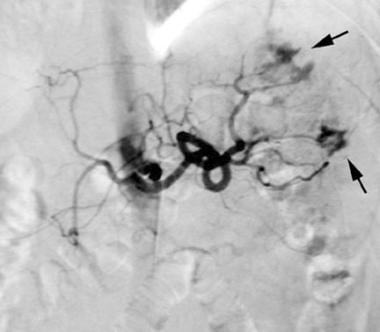 Vascular and solid organ trauma. Celiac angiogram (same patient as in the previous image) showing 3 foci of extravasation in spleen, 2 in the upper pole (arrow) and 1 in the lateral aspect of the mid spleen (arrow; courtesy of the Society of Cardiovascular and Interventional Radiology).
Vascular and solid organ trauma. Celiac angiogram (same patient as in the previous image) showing 3 foci of extravasation in spleen, 2 in the upper pole (arrow) and 1 in the lateral aspect of the mid spleen (arrow; courtesy of the Society of Cardiovascular and Interventional Radiology).
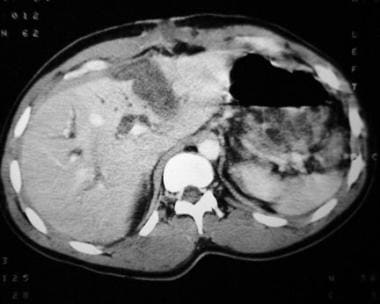
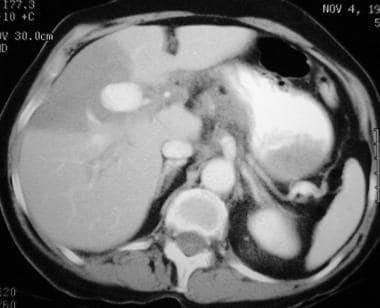 Contrast-enhanced CT of a 65-year-old woman with a remote history of blunt abdominal trauma and severe abdominal pain. A large pseudoaneurysm is present and is associated with an infarcted segment of the liver.
Contrast-enhanced CT of a 65-year-old woman with a remote history of blunt abdominal trauma and severe abdominal pain. A large pseudoaneurysm is present and is associated with an infarcted segment of the liver.
Indications for interventional radiology in hemodynamically unstable patients with severe trauma remains unclear. In an attempt to address this issue, Otsuka et al retrospectively evaluated 16 severe trauma patients (collectively, 10 pelvic fractures; 5 live injuries; 1 splenic; and 1 renal; 1 transection each of the external carotid, vertebral, axillosubclavian, intercostal, and lumbar arteries) whose systolic blood pressure was ≤90 mmHg, without improvement following primary resuscitation, and whose first intervention was interventional radiology. They found that systolic blood pressure, pulse rate, base excess/deficit, serum-lactate levels, and D-dimer values were significantly improved after interventional radiology. Mortality was 25%, and no preventable deaths were noted. Eight patients showed unexpected survival. [12]
In a study by Garg et al, 25 patients who presented with either persistent hematuria or hemodynamic instability after traumatic or iatrogenic renal injuries underwent angiographic embolization with coils, glue, or Gelfoam to address the vascular injuries. Coiling alone had a 79.16% technical success rate, and additional use of glue in 4 cases resulted in a 95.83% technical success rate. The ultimate technical and clinical success rate of interventional radiology in renal trauma management was 100%. [13]
Computed tomography
CT usually is the imaging modality of choice; it is widely used in trauma cases, for the following reasons:
-
It may be used to grade solid organ injuries.
-
It can detect hemorrhage. On contrast-enhanced scans, extravasation (representing active bleeding) may be represented by a high attenuation focus caused by contrast media leak from a vessel. On non–contrast-enhanced scans, active or recent bleeding may be represented by high attenuation clot or blood (ie, the sentinel clot sign implies ongoing hemorrhage).
-
It may be used to detect vascular abnormalities, such as pseudoaneurysm, intimal dissection, arteriovenous fistula, and vascular occlusion.
-
It is useful in predicting which hemodynamically stable patients may benefit from nonoperative management.
Catheter angiography
In the selected trauma patient with suspected vascular injury or hemorrhage, diagnostic catheter angiography usually is performed. Catheter angiography may be performed as a screening procedure or to plan definitive transcatheter or surgical therapy. It is used as follows:
-
A large-field nonselective study, such as an abdominal aortogram, is obtained first.
-
Angiography may detect bleeding and may help in planning further selective studies.
-
Selective studies are performed to detect more subtle hemorrhage and vascular injuries and to direct further treatment, such as transcatheter embolization.
-
Angiography should be obtained early and quickly to diagnose hemorrhage immediately and to exploit an intact clotting cascade should transcatheter embolization be needed.
-
Indications for emergency catheter angiography in the trauma patient include clinical signs or symptoms of hemorrhage or CT evidence of ongoing hemorrhage or vascular injury.
-
In penetrating abdominal trauma, abdominal angiography rarely is indicated, because emergency laparotomy usually is indicated.
Transcatheter embolization
Transcatheter embolization (embolotherapy) is the intentional occlusion of a vessel by deposition of thrombogenic materials directly into the vessel via an angiographic catheter under remote control. Transcatheter embolization is the mainstay of modern interventional trauma radiology.
The arteries to be treated must be expendable or nonessential, or they must supply a relatively infarction-resistant vascular bed. Alternatively, they must be associated with distal collateral vessels, such as selective hepatic arteries; alternatively, if they are true end arteries, they must have adequate parenchymal reserve, as with selective renal artery embolization. Usually, these arteries can be ligated surgically.
Transcatheter embolization of active hemorrhage or vascular injury often is considered preferable to surgical treatment; this is the case in the following circumstances:
-
When rapid occlusion is desired
-
When surgical access is difficult
-
When the patient is a poor operative risk
-
When selective transcatheter embolization may limit the amount of normal tissue or parenchyma necrotized
Metallic coils and gelatin sponge
In trauma, the 2 embolic agents of choice are metallic coils and gelatin sponge. Coils are made of various metals; they are usually fortified with soft fabric material to increase thrombogenicity.
Coils have are permanent occluding agents that remain at the site of deposition. They are best applied in single-vessel injuries; are placed quickly with a high degree of accuracy; and are available in a wide variety of sizes, diameters, lengths, and shapes. Detachable coils include mechanical and electrolytic mechanisms of detachment; they are ideal for occluding aneurysmal sac and may be retrieved if placement is suboptimal.
Gelatin sponges are a temporary occluding agent; the artery often recanalizes within weeks to months. They are best applied in cases involving single or multiple injuries of smaller arteries and are useful when more distal occlusion is necessary or when multiple collateral channels are present. They are administered as a slurry by mixing gelatin sponge powder with nonionic contrast material or as pledgets of various sizes.
Other embolic agents
Other embolic agents that are used less often in the trauma setting include polyvinyl alcoho l(PVA), microspheres, Onyx liquid embolic agent, and N-butyl cyanoacrylate (nBCA) or tissue glue.
PVA is a permanent occluding agent. It is available in small-size particles and is administered in a suspension with contrast material.
Microspheres are permanent embolic agents that are available in different particle sizes.
Onyx is a cohesive liquid agent, which is delivered with a special microcatheter. It causes a permanent occlusion.
Tissue glue is an injectable tissue adhesive. It polymerizes into a solid state when exposed to an ionized fluid, such as blood, and causes a permanent occlusion.
Stents
Stent-grafts or covered stents provide a means of salvaging injured or hemorrhaging arteries and increase the options for transcatheter treatment. Bare stents have been used successfully in the treatment of intimal dissection and pseudoaneurysm, as well as acute rupture. Stent grafts, either custom made or commercially available, are alternatives for treating arterial rupture or pseudoaneurysm in suitable vessels.
Stents are covered with vein or synthetic materials, such as polytetrafluoroethylene, polyethylene terephthalate (eg, Dacron), polycarbonate urethane compounds, or other proprietary materials. The stents may be expanded with balloons or are self-expandable. Stents exclude and effectively repair the injured arterial segment.
American College of Radiology recommendations
The ACR has provided imaging recommendations for major blunt trauma divided into 8 different vaiants [14] :
- Hemodynamically unstable. Radiography trauma series and ultrasound FAST (focused assessment with sonography in trauma) scan of the chest, abdomen, and pelvis are usually appropriate for initial imaging. These procedures are complementary (ie, more than one procedure is ordered as a set or simultaneously, where each procedure provides unique clinical information to effectively manage the patient’s care).
- Hemodynamically stable, not otherwise specified. Whole-body CT with IV contrast, radiography trauma series, and US FAST scan of the chest, abdomen, and pelvis are usually appropriate for initial imaging. These procedures are complementary (ie, more than one procedure is ordered as a set or simultaneously, where each procedure provides unique clinical information to effectively manage the patient’s care).
- Hemodynamically stable, suspected facial injury. Maxillofacial CT without IV contrast, head CT without IV contrast, or a radiography trauma series is usually appropriate for initial imaging. These procedures are complementary.
- Hemodynamically stable, suspected extremity trauma. US FAST scan of the chest, abdomen, and pelvis can be useful as a limited bedside adjunct to the physical examination and is primarily used for triage in these patients. Radiography of the extremity, whole-body CT with IV contrast, or a radiography trauma series is usually appropriate in addition to US FAST for the initial imaging of these patients. These procedures are equivalent alternatives.
- Hemodynamically stable, suspected bowel trauma. US FAST scan of the chest, abdomen, and pelvis can be useful as a limited bedside adjunct to the physical examination and is primarily used for triage in these patients. CT of the abdomen and pelvis with IV contrast, CT of the whole body with IV contrast, or a radiography trauma series is usually appropriate in addition to US FAST for the initial imaging of these patients. These procedures are equivalent alternatives
- Hemodynamically stable, suspected urinary system, including urethra trauma. US FAST scan of the chest, abdomen, and pelvis can be useful as a limited bedside adjunct to the physical examination and is primarily used for triage in these patients. Fluoroscopic retrograde urethrography, a radiography trauma series, CT of the abdomen and pelvis with IV contrast, CT of the whole body with IV contrast, or CT angiography of the abdomen and pelvis with IV contrast is usually appropriate in addition to US FAST for the initial imaging of these patients. These procedures are equivalent alternatives.
- Hemodynamically stable, suspected chest trauma. CT of the chest with IV contrast, CT of the whole body with IV contrast, CT angiography of the chest with IV contrast, or a radiography trauma series is usually appropriate for initial imaging. These procedures are equivalent alternatives.
- Hemodynamically stable, pregnant patient. US FAST scan of the chest, abdomen, and pelvis can be useful as a limited bedside adjunct to the physical examination and is primarily used for triage. US of the pelvis, CT of the abdomen and pelvis with IV contrast, CT of the whole body with IV contrast, or a radiography trauma series is usually appropriate in addition to US FAST for initial imaging. These procedures are equivalent alternatives.
Acute Thoracic Aortic Injury
Incidence and natural history
Synonyms for acute thoracic aortic injury (ATAI) include aortic transection, aortic traumatic pseudoaneurysm, aortic rupture, aortic laceration, and aortic tear. ATAIs are responsible for 10-20% of high-speed traffic accident fatalities. More than 8000 cases per year have been documented in the United States. Most ATAIs represent full-thickness tears; in most cases, ATAIs are fatal, with death occurring at the scene of the accident.
Of patients with ATAI, 10-23% survive long enough to present to the hospital. Among cases of ATAI in patients who survive, approximately 30% are fatal within 6 hours, and 40% are fatal within 24 hours if undiagnosed and left untreated. Only 2-10% of untreated patients survive longer than 6 months.
ATAIs are caused by the rapid deceleration forces produced by high-speed motor vehicle accidents or falls from great heights. During acute deceleration, the thoracic aorta is relatively fixed in position at the aortic root, isthmus, and diaphragm. Movement of the aorta about these points of fixation causes stress and tethering, resulting in a tear at one or more of these locations.
Among patients who experience ATAI and who survive, the locations of the distribution of tears are as follows:
-
Aortic isthmus, 80-90%
-
Ascending aorta, 5-9%
-
Diaphragmatic aorta, 1-3%
Pathologically, a transverse tear of the aortic intima and media is found; in approximately 60% of patients, the adventitia is intact.
Of ATAI cases that are fatal at the scene, a higher percentage of lacerations involve the aortic root.
Multiple sites of ATAI occur in 6-20% of patients; aortic arch branch artery injuries occur in 4-10% of patients.
Imaging studies
Imaging of ATAIs consists of plain radiography, CT, conventional thoracic aortography, transesophageal echocardiography, intravascular ultrasound, MRI, and magnetic resonance angiography. Of these, the 3 most commonly used modalities in the assessment of ATAI are plain radiography, CT, and conventional thoracic aortography. [15, 16, 17, 18, 19, 20, 21, 22] According to the Society of Interventional Radiology, emergent thoracic endovascular aortic repair (TEVAR) should be used in anatomically favorable grade 3 and grade 4 aortic injuries, with nonoperative management (antihypertensive and antiimpulse medication with close symptomatic and/or radiographic follow-up) favored for grade 1 and grade 2 injuries. [2]
Radiography
Plain chest radiography has a negative predictive value of 98% and is nonspecific. Findings include the following:
-
Widened mediastinum
-
Obscured aortic knob or aortopulmonary window
-
Deviation of nasogastric tube or trachea
-
Depressed left mainstem bronchus
-
Apical pleural cap
-
Left hemothorax
-
Abnormal aortic contour
-
Wide paraspinal stripe
-
First and second rib fractures
-
Thick paratracheal stripe
Computed tomography
Computed tomography for detection of mediastinal hematoma is superior to chest radiography; it has a lower rate of false-positive results. Isolated aortic injuries without a mediastinal hematoma are rare. Screening for mediastinal hematoma by CT may increase the rate of positive findings on conventional thoracic aortography. It demonstrates a sensitivity of 100% in aortic injury and has a negative predictive value of 100%.
CT for detection of aortic injury (see the images below) has a sensitivity of 100% and specificity of 96% in aortic injury. The negative predictive value is 100%.
 A 3-dimensional reconstruction of contrast-enhanced CT of acute traumatic aortic injury (same patient as in the previous 2 images).
A 3-dimensional reconstruction of contrast-enhanced CT of acute traumatic aortic injury (same patient as in the previous 2 images).
Findings on CT include the following:
-
Intraluminal low-attenuation focus
-
Contour abnormality
-
Pseudoaneurysm
-
Intramural hematoma
-
Localized dissection
Catheter aortography
Conventional catheter aortography (see the images below) is the standard of reference to which all other imaging modalities are compared, with a sensitivity of almost 100% and a specificity of 98%. Advantages include good evaluation of ascending thoracic aorta and brachiocephalic arteries. Catheter aortography may be used in conjunction with intravascular ultrasound, and it may be necessary for endovascular (stent-graft) treatment planning. However, to detect a subtle injury, 2 or more views are required.
 Digital subtraction catheter aortogram (late phase) of a typical acute traumatic aortic injury (same patient as in the previous image).
Digital subtraction catheter aortogram (late phase) of a typical acute traumatic aortic injury (same patient as in the previous image).
Findings on catheter aortography include the following:
-
Intimal irregularity
-
Linear defect
-
Intimal flap
-
Contour abnormality
-
Pseudoaneurysm
-
Extravasation
-
Thickened wall
Pitfalls of catheter angiography include the following:
-
Anatomic variants
-
Atheromatous plaque
-
True aneurysm (ductus aneurysm)
-
Ductus diverticulum
-
Aortic spindle
-
Infundibulum of intercostal artery
-
Digital subtraction artifacts
Treatment
Treatment of ATAI should follow the diagnosis promptly. Most patients require surgical repair of the thoracic aorta, usually with an interposition graft. Some patients are not good operative candidates because of concomitant injuries or comorbidities.
In the past, patients who were poor operative risks were treated with medical control of blood pressure and observation in some centers. Currently, selected patients are treated with endovascular aortic stent-grafts; with this approach, the risk associated with a thoracotomy may be avoided. [23, 24, 25, 26, 27, 28, 29]
in cases of of thoracic endovascular aortic repair (TEVAR) long-term follow-up is recommended because endoleaks can develop. CT angiography is the imaging modality of choice, given its sensitivity for the detection of endoleaks, changes in aortic/aneurysm diameter, evaluation of false lumen thrombosis, assessment for device migration and integrity. [30]
Splenic Trauma
The traditional treatment of blunt splenic trauma was surgical splenectomy; however, a trend of splenic salvage through nonoperative management of splenic injury has emerged as traumatologists have come to recognize the important role the spleen plays in preventing overwhelming sepsis by encapsulated organisms such as pneumococcus. [31, 32, 33, 34, 35, 36]
Nonoperative management should be considered for patients with splenic injury who are hemodynamically stable and who have no associated abdominal or CNS injuries that may preclude an accurate assessment of the abdomen by physical examination. CT is the imaging modality of choice to make the diagnosis of splenic injury, and it may help in grading the degree of injury. Grading scales have been developed to categorize the degree of injury and to assess the likelihood of splenic salvage, but such scales do not have predictive power on an individual basis. [37, 38, 39]
Some studies have shown that as many as 70% of patients with blunt splenic injuries may be treated nonoperatively, with success rates of 71-97%. Nonoperative management of splenic injuries is effective in more than 95% of children.
The American Association for the Surgery of Trauma has developed scales for classifying the severity of organ injury. [40] The system for grading injury to the spleen is as follows:
-
Grade I — Small subcapsular hematoma (< 10% of surface area)
-
Grade II — Moderate subcapsular hematoma on 10-50% of surface area; intraparenchymal hematoma < 5 cm in diameter; capsular laceration < 1 cm deep
-
Grade III — Large or expanding subcapsular hematoma on more than 50% of surface area; intraparenchymal hematoma greater than 5 cm in diameter; capsular laceration 1-3 cm deep
-
Grade IV — Laceration more than 3 cm deep; laceration involving segmental or hilar vessels producing major devascularization (>25%)
-
Grade V — Shattered spleen; hilar injury that results in devascularization of the spleen
Imaging studies
Helical CT may be useful in predicting which hemodynamically stable patients may fail nonoperative management if extravasation or posttraumatic splenic vascular injury within the spleen is demonstrated. These patients should be referred for transcatheter embolization of the spleen (see the images below).
 Vascular and solid organ trauma. Contrast-enhanced CT of the abdomen in a hemodynamically stable patient with evidence of persistent hemorrhage following a motor vehicle accident. Arrow points to contrast extravasation in a lacerated spleen (Courtesy of the Society of Cardiovascular and Interventional Radiology).
Vascular and solid organ trauma. Contrast-enhanced CT of the abdomen in a hemodynamically stable patient with evidence of persistent hemorrhage following a motor vehicle accident. Arrow points to contrast extravasation in a lacerated spleen (Courtesy of the Society of Cardiovascular and Interventional Radiology).
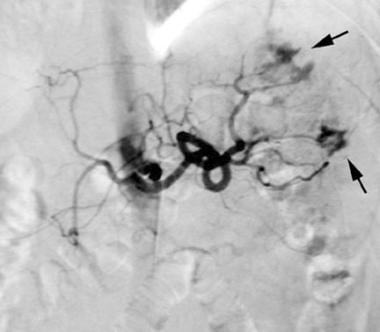 Vascular and solid organ trauma. Celiac angiogram (same patient as in the previous image) showing 3 foci of extravasation in spleen, 2 in the upper pole (arrow) and 1 in the lateral aspect of the mid spleen (arrow; courtesy of the Society of Cardiovascular and Interventional Radiology).
Vascular and solid organ trauma. Celiac angiogram (same patient as in the previous image) showing 3 foci of extravasation in spleen, 2 in the upper pole (arrow) and 1 in the lateral aspect of the mid spleen (arrow; courtesy of the Society of Cardiovascular and Interventional Radiology).
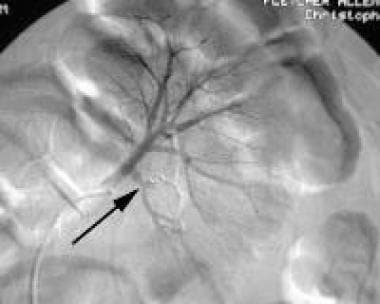
 Vascular and solid organ trauma. Post—super-selective embolization splenic angiogram demonstrating microcoils in good position and no evidence of further extravasation (same patient as in the previous 2 images; courtesy of the Society of Cardiovascular and Interventional Radiology).
Vascular and solid organ trauma. Post—super-selective embolization splenic angiogram demonstrating microcoils in good position and no evidence of further extravasation (same patient as in the previous 2 images; courtesy of the Society of Cardiovascular and Interventional Radiology).
The absence of extravasation on conventional angiography may be used to identify patients who may be managed successfully nonoperatively. Some investigators have recommended the liberal use of conventional angiography and transcatheter splenic artery embolization to increase the number of patients successfully managed nonoperatively.
If CT evidence of splenic injury is seen in a hemodynamically stable patient, celiac and splenic angiography is employed. If intrasplenic extravasation is documented, the splenic artery is embolized to occlusion using coils just distal to the dorsal pancreatic artery. If extrasplenic extravasation is documented, a more distal embolization of the splenic artery branches is performed with gelatin sponge pledgets until extravasation resolves; this is followed by coil embolization of the main splenic artery. This may result in a large percentage of patients being treated nonoperatively with a high success rate.
Treatment
Transcatheter embolization is used for blunt splenic trauma. The indication is extravasation or vascular injury. Techniques include the following:
-
Proximal coil embolization just distal to the dorsal pancreatic artery and proximal to the pancreatic magna artery to decrease the head of pressure and to preserve distal collateral flow
-
Nonselective distal embolization using smaller particles such as Gelfoam pledgets
-
Superselective distal embolization using a microcatheter and microcoils, polyvinyl alcohol particles, or microspheres at the bleeding site
-
Combination of proximal and distal embolization
For grade IV splenic injuries, Sclafani et al reported an 84% salvage rate, [41] and Shanmuganathan et al reported a 94% salvage rate when using splenic embolization. [42] In comparison, Brasel et al reported only a 4% salvage rate using only nonoperative treatment. [43]
According to the Society of Interventional Radiology, splenic artery embolization should be considered in hemodynamically stable patients with grade IV/V blunt splenic trauma or with any grade injury who have imaging or clinical evidence of splenic hemorrhage. [2]
Complications of splenic embolization include inadvertent embolization, splenic infarction and/or abscess, and splenic artery dissection.
Hepatic Trauma
Analogous to splenic injury, the trend in blunt hepatic trauma is nonoperative management of the hemodynamically stable patient. The traditional treatment of liver trauma was exploration and surgical packing, but the nontherapeutic laparotomy rate was as high as 67%, largely because in most cases of liver injury, hemorrhage resolves spontaneously before laparotomy can be performed (see the images below). [44, 45, 46, 47, 48, 49, 50]
According to the Society of Interventional Radiology, nonoperative management is becoming the treatment of choice for patients with blunt hepatic injury who are hemodynamically stable, resulting in decreased abdominal infections, transfusions, and length of hospital stay. They recommend that embolization be considered in cases of ongoing bleeding, to identify an arterial source of bleeding on imaging, or when there is suspicion of a persistent source of arterial bleeding despite operative intervention. [2]
 Contrast-enhanced CT demonstrating a liver laceration in a patient who sustained blunt abdominal trauma (Courtesy of Dr Robert D'Agostino).
Contrast-enhanced CT demonstrating a liver laceration in a patient who sustained blunt abdominal trauma (Courtesy of Dr Robert D'Agostino).
 Vascular and solid organ trauma. Hepatic angiogram (same patient as in the previous image) showing a pseudoaneurysm of a branch of the left hepatic artery (arrow) located in the region of the hepatic laceration (Courtesy of Dr Robert D'Agostino).
Vascular and solid organ trauma. Hepatic angiogram (same patient as in the previous image) showing a pseudoaneurysm of a branch of the left hepatic artery (arrow) located in the region of the hepatic laceration (Courtesy of Dr Robert D'Agostino).
 Vascular and solid organ trauma. Postembolization angiogram of left hepatic branch artery pseudoaneurysm. The coil (arrow) is in satisfactory position and is occluding the pseudoaneurysm (same patient as in the previous 2 images; courtesy of Dr Robert D'Agostino).
Vascular and solid organ trauma. Postembolization angiogram of left hepatic branch artery pseudoaneurysm. The coil (arrow) is in satisfactory position and is occluding the pseudoaneurysm (same patient as in the previous 2 images; courtesy of Dr Robert D'Agostino).
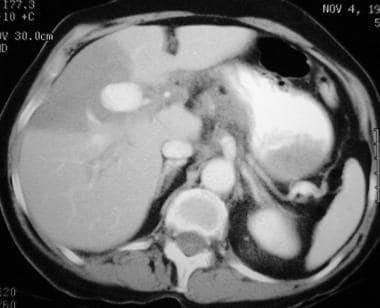 Contrast-enhanced CT of a 65-year-old woman with a remote history of blunt abdominal trauma and severe abdominal pain. A large pseudoaneurysm is present and is associated with an infarcted segment of the liver.
Contrast-enhanced CT of a 65-year-old woman with a remote history of blunt abdominal trauma and severe abdominal pain. A large pseudoaneurysm is present and is associated with an infarcted segment of the liver.
 Vascular and solid organ trauma. Hepatic angiogram (same patient as in the previous image) demonstrates large bilobed pseudoaneurysm of right hepatic artery. Notice the "jet effect" of contrast material extending from the lower to the upper pseudoaneurysm sac. In addition, an aneurysm of the proper hepatic artery and diffuse ectasia of the proximal right hepatic artery are apparent.
Vascular and solid organ trauma. Hepatic angiogram (same patient as in the previous image) demonstrates large bilobed pseudoaneurysm of right hepatic artery. Notice the "jet effect" of contrast material extending from the lower to the upper pseudoaneurysm sac. In addition, an aneurysm of the proper hepatic artery and diffuse ectasia of the proximal right hepatic artery are apparent.
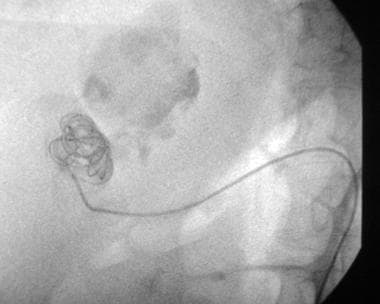 Vascular and solid organ trauma. Fluoroscopic control image (same patient as in the previous 2 images) showing a catheter in the lower component of the bilobed pseudoaneurysm. Multiple stainless steel embolization coils have been deposited into the pseudoaneurysm.
Vascular and solid organ trauma. Fluoroscopic control image (same patient as in the previous 2 images) showing a catheter in the lower component of the bilobed pseudoaneurysm. Multiple stainless steel embolization coils have been deposited into the pseudoaneurysm.
 Vascular and solid organ trauma. Immediate postembolization hepatic angiogram demonstrating occlusion of the complex right hepatic artery, pseudoaneurysm, and back thrombosis of the entire right hepatic artery (same patient as in the previous 3 images).
Vascular and solid organ trauma. Immediate postembolization hepatic angiogram demonstrating occlusion of the complex right hepatic artery, pseudoaneurysm, and back thrombosis of the entire right hepatic artery (same patient as in the previous 3 images).
 Vascular and solid organ trauma. Contrast-enhanced 5-month follow-up CT (same patient as in the previous 4 images) demonstrating coils in shrunken pseudoaneurysm sac and scarring in region of previous hepatic infarction.
Vascular and solid organ trauma. Contrast-enhanced 5-month follow-up CT (same patient as in the previous 4 images) demonstrating coils in shrunken pseudoaneurysm sac and scarring in region of previous hepatic infarction.
 Vascular and solid organ trauma. Celiac angiogram 5-month follow-up image (same patient as in the previous 5 images) showing occlusion of pseudoaneurysm and entire right hepatic, left hepatic, and common hepatic arteries.
Vascular and solid organ trauma. Celiac angiogram 5-month follow-up image (same patient as in the previous 5 images) showing occlusion of pseudoaneurysm and entire right hepatic, left hepatic, and common hepatic arteries.
The grade of hepatic injury does not necessarily correlate with the rate of success of nonoperative treatment. In grade III and IV liver injuries, reported success rates for nonoperative management range widely. Overall, the nonoperative success rate in patients with liver trauma has been reported to be as high as 89-98%. Patients who are hemodynamically stable but show ongoing signs of hemorrhage (which occurs in 3% of patients) or who have documented extravasation on CT of the liver should undergo conventional angiography of the liver. If these patients have angiographic extravasation, pseudoaneurysm, arteriovenous fistula, or arteriobiliary fistula, transcatheter embolization of the abnormal site should be performed. [51]
The American Association for the Surgery of Trauma's scale for grading the severity of injury to the liver is as follows [40] :
-
Grade I — Capsular avulsion; periportal blood tracking; superficial laceration less than 1 cm deep; subcapsular hematoma less than 1 cm thick
-
Grade II — Laceration 1-3 cm deep; subcapsular/central hematoma 1-3 cm in diameter
-
Grade III — Laceration greater than 3 cm deep; subcapsular/central hematoma greater than 3 cm in diameter
-
Grade IV — Massive central or subcapsular hematoma greater than 10 cm; lobar tissue maceration or devascularization
-
Grade V — Bilobar tissue maceration or devascularization
Treatment
Features of transcatheter embolization of the liver are as follows:
-
The dual blood supply of the liver makes postembolization infarction less likely
-
An occluded portal vein is a relative contraindication
-
Superselective embolization with Gelfoam pledgets or coils/microcoils is desirable
-
PVA and tissue glue have been used successfully as embolic agents in the hepatic arteries
-
The complication rate is low
-
Penetrating injuries of the liver from stab and gunshot wounds have been managed successfully with transcatheter embolization using criteria similar to those used in cases of blunt hepatic injury.
Renal Trauma
The management of blunt trauma of the kidneys has become increasingly conservative over the past 10 years, with many grade I and grade II injuries treated nonoperatively with observation. As with splenic and hepatic injuries, transcatheter embolization may be used to treat hemodynamically stable patients in the following settings: there is evidence of ongoing hemorrhage; there is CT evidence of extravasation or vascular injury; there is persistent or recurrent hematuria; or large retroperitoneal hematomas are present (see the images below). [52, 53, 54, 55, 56, 57, 58, 59] According to the Society of Interventional Radiology, angiography and embolization should be considered in patients with grade III/IV renal injuries when surgical exploration is not warranted. [2]
 Contrast-enhanced CT in a 9-year-old boy who sustained blunt abdominal injury after falling onto the handle bar of his bicycle. He presented with exsanguinating hematuria caused by a fractured left kidney. CT demonstrates a pseudoaneurysm (arrow) off of an intrarenal artery branch.
Contrast-enhanced CT in a 9-year-old boy who sustained blunt abdominal injury after falling onto the handle bar of his bicycle. He presented with exsanguinating hematuria caused by a fractured left kidney. CT demonstrates a pseudoaneurysm (arrow) off of an intrarenal artery branch.
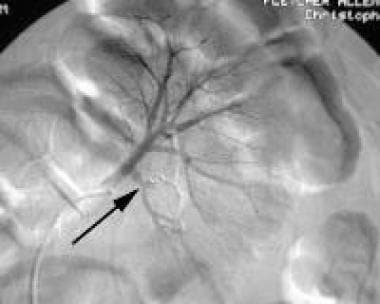
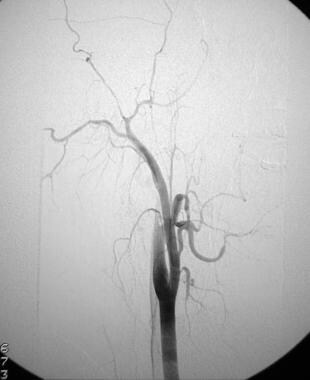
 Left renal angiogram (early phase; same patient as in the previous image shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
Left renal angiogram (early phase; same patient as in the previous image shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
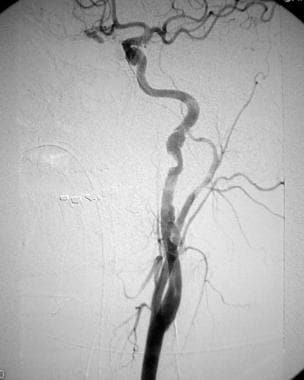
 Left renal angiogram (late phase; same patient as in the previous 2 images) shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
Left renal angiogram (late phase; same patient as in the previous 2 images) shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
 Postembolization left renal angiogram (same patient as in the previous 3 images) shows stainless steel embolization coil (arrow) completely occluding the renal artery branch previously containing the pseudoaneurysm.
Postembolization left renal angiogram (same patient as in the previous 3 images) shows stainless steel embolization coil (arrow) completely occluding the renal artery branch previously containing the pseudoaneurysm.
 A 30-year-old woman who sustained blunt abdominal trauma. Contrast-enhanced CT demonstrates a large perirenal hematoma and a fractured right kidney. CT evidence of acute extravasation is present.
A 30-year-old woman who sustained blunt abdominal trauma. Contrast-enhanced CT demonstrates a large perirenal hematoma and a fractured right kidney. CT evidence of acute extravasation is present.
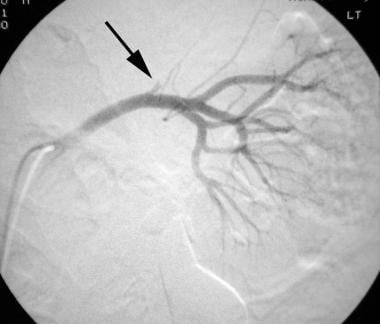
 Selective renal angiogram (same patient as in the previous image) reveals a vascular pedicle injury with an avulsed renal artery branch, multiple renal artery branch occlusions, and an inhomogeneous nephrogram but no active extravasation. Major devascularization is present. The patient had signs of persistent hemorrhage and was hypotensive.
Selective renal angiogram (same patient as in the previous image) reveals a vascular pedicle injury with an avulsed renal artery branch, multiple renal artery branch occlusions, and an inhomogeneous nephrogram but no active extravasation. Major devascularization is present. The patient had signs of persistent hemorrhage and was hypotensive.
 Immediate postembolization renal angiogram demonstrates a satisfactory position of stainless steel coils effectively occluding the main right renal artery. A surgical nephrectomy was planned (same patient as in the previous 2 images).
Immediate postembolization renal angiogram demonstrates a satisfactory position of stainless steel coils effectively occluding the main right renal artery. A surgical nephrectomy was planned (same patient as in the previous 2 images).
 Contrast-enhanced CT in a 9-year-old boy who sustained blunt abdominal injury after falling onto the handle bar of his bicycle. He presented with exsanguinating hematuria caused by a fractured left kidney. CT demonstrates a pseudoaneurysm (arrow) off of an intrarenal artery branch.
Contrast-enhanced CT in a 9-year-old boy who sustained blunt abdominal injury after falling onto the handle bar of his bicycle. He presented with exsanguinating hematuria caused by a fractured left kidney. CT demonstrates a pseudoaneurysm (arrow) off of an intrarenal artery branch.
 Left renal angiogram (early phase; same patient as in the previous image shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
Left renal angiogram (early phase; same patient as in the previous image shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
 Left renal angiogram (late phase; same patient as in the previous 2 images) shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
Left renal angiogram (late phase; same patient as in the previous 2 images) shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
 Postembolization left renal angiogram (same patient as in the previous 3 images) shows stainless steel embolization coil (arrow) completely occluding the renal artery branch previously containing the pseudoaneurysm.
Postembolization left renal angiogram (same patient as in the previous 3 images) shows stainless steel embolization coil (arrow) completely occluding the renal artery branch previously containing the pseudoaneurysm.
Although the treatment of more severe grade III renal injuries is more controversial, there is a trend to treat these injuries nonoperatively as well. In more severe kidney injuries, surgery results in nephrectomy in as many as one third of patients. A perinephric hematoma usually is contained partly by the Gerota fascia. When this is opened with surgery, significant blood loss may occur if vascular control is not obtained promptly. Thus, the physician may elect to perform a trial of transcatheter embolization of the bleeding sites or vascular abnormalities.
Grade IV or V blunt renal injuries usually require surgery for definitive treatment, which also may result in nephrectomy; however, some of these injuries may be managed nonoperatively.
In cases of penetrating renal trauma, surgical exploration is commonly employed, particularly if the peritoneum has been transgressed. Conventional angiography may delineate precisely the status of the renal vasculature preoperatively; it may be a prelude to transcatheter embolization in a limited number of cases (see the images below).
 Selective left renal angiogram in an older man with an expanding retroperitoneal hematoma. This was secondary to penetrating trauma to the flank following an encounter with an angry bull. The arrow delineates the avulsed left renal artery branch to the upper pole of the left kidney (Courtesy of Dr Kenneth E Najarian).
Selective left renal angiogram in an older man with an expanding retroperitoneal hematoma. This was secondary to penetrating trauma to the flank following an encounter with an angry bull. The arrow delineates the avulsed left renal artery branch to the upper pole of the left kidney (Courtesy of Dr Kenneth E Najarian).
 Control angiogram (same patient as in the previous image) obtained immediately before deployment of a custom-made stent -graft across the origin of the avulsed left renal artery branch. The balloon-mounted stent-graft is in a good position and is ready to be deployed (Courtesy of Dr Kenneth E Najarian).
Control angiogram (same patient as in the previous image) obtained immediately before deployment of a custom-made stent -graft across the origin of the avulsed left renal artery branch. The balloon-mounted stent-graft is in a good position and is ready to be deployed (Courtesy of Dr Kenneth E Najarian).
 Post–stent-graft deployment left renal angiogram (same patient as in the previous 2 images). The avulsed branch artery has been excluded effectively (Courtesy of Dr Kenneth E Najarian).
Post–stent-graft deployment left renal angiogram (same patient as in the previous 2 images). The avulsed branch artery has been excluded effectively (Courtesy of Dr Kenneth E Najarian).
Nonvascular percutaneous intervention may be applied to urinoma, urine leak, ureteral laceration, and transection injuries. These interventions include percutaneous nephrostomy for urine diversion, ureteral stent placement for ureteral injuries, and drainage tube placement for urinoma formation. [60, 61, 62, 63, 64, 65]
The American Association for the Surgery of Trauma's system for grading injury to the kidney is as follows:
-
Grade I — Contusion or contained and nonexpanding subcapsular hematoma, without parenchymal laceration; hematuria
-
Grade II — Nonexpanding, confined, perirenal hematoma or cortical laceration less than 1 cm deep; no urinary extravasation
-
Grade III — Parenchymal laceration extending more than 1 cm into cortex; no collecting system rupture or urinary extravasation
-
Grade IV — Parenchymal laceration extending through the renal cortex, medulla, and collecting system
-
Grade V — Pedicle injury or avulsion of renal hilum that devascularizes the kidney; completely shattered kidney; thrombosis of the main renal artery
The Genitourinary Trauma Study, a multicenter study including high-grade renal trauma (HGRT) patients from 14 level I trauma centers, categorized admission CT scans based on multiple variables, including vascular contrast extravasation (VCE). The presence of VCE was associated with a 5.9-fold increased risk of interventions. [66]
In a study by Garg et al, 25 patients who presented with either persistent hematuria or hemodynamic instability after traumatic or iatrogenic renal injuries underwent angiographic embolization with coils, glue, or Gelfoam to address the vascular injuries. Coiling alone had a 79.16% technical success rate, and additional use of glue in 4 cases resulted in a 95.83% technical success rate. The ultimate technical and clinical success rate of interventional radiology in renal trauma management was 100%. [13]
Pelvic Trauma
Because of the extensive collateral supply and the limitations of surgery for pelvic hematomas, angiographic treatment is at the forefront of pelvic trauma management. The American College of Surgeons Committee on Trauma has recommended that an interventional radiologist be available within 30 minutes to perform procedures in all level I and level II trauma centers. [67, 68, 1, 69, 70, 71] The Society of Interventional Radiology has recommended that for pelvic trauma, embolization should be first-line therapy. They also note that when the clinical condition permits, contrast-enhanced CT should be pursued because it is the most sensitive and specific test to identify the source of arterial bleeding in the pelvis. [2, 72, 73, 74]
Hemorrhage associated with pelvic trauma, with or without pelvic fracture, is common and may arise from venous, osseous, or arterial sources or any combination of the above. Typically, pelvic hemorrhage is treated first with the use of external fixation; external fixation is usually successful in treating venous and osseous bleeding, through a tamponade effect. External fixation may reduce a fracture and/or dislocation, thus decreasing the pelvic space and increasing the tamponade effect. [75, 76, 77]
Continued bleeding may indicate an arterial source; such bleeding is associated with high morbidity and mortality rates. Intractable hemorrhage associated with pelvic fracture is a large contributor to the overall mortality rate of approximately 10%. Surgical exploration and intervention of a pelvic hematoma often is complex, owing to the difficulties in visualizing the hemorrhaging artery or arteries within the extraperitoneal hematoma and in gaining arterial control. In addition, an operation exposes the patient to the added risk of increased blood loss through surgical disruption of the pelvic fascia; this may be important in the tamponade of the hematoma.
Conventional angiography and, potentially, transcatheter embolization may be employed for patients with pelvic trauma who have already undergone abdominal exploration and are known to have an associated solid organ injury and who continue to hemorrhage despite external fixation. [78, 79] Angiography may be obtained before external fixation or surgical abdominal exploration if significant hemorrhage is present, even in unstable patients. [80]
Transcatheter embolization of pelvic trauma that is performed early (within 3 hours of presentation) has been shown to lower the mortality rate. When angiography is performed, extravasation is documented in approximately one half of patients; in such cases, transcatheter embolization is warranted.
As with other injuries, Cerva et al and Stephen et al showed that CT is indispensable in diagnosing and monitoring pelvic hemorrhage. [81, 82] CT also is necessary in making the diagnosis of and classifying pelvic fractures and/or dislocations. CT evidence of extravasation in the pelvis is an indication for transcatheter embolization.
In pelvic trauma, arterial bleeding most frequently occurs from superior gluteal and internal pudendal arteries. The fascia of the piriformis muscle may lacerate the superior gluteal artery, even in the absence of fracture. All branches of the hypogastric artery are at risk for bleeding.
Knowledge of the relationship of branch arteries of the hypogastric artery to the surrounding and adjacent musculotendinous and ligamentous structures is helpful in predicting arterial injuries and in directing selective catheterization for angiography. Pelvic and retroperitoneal hemorrhage also may arise from the lumbar, inferior epigastric, deep circumflex iliac, and middle sacral arteries.
Imaging studies
For pelvic angiography, access from the common femoral artery contralateral to the pelvic hematoma, fracture, or extravasation is demonstrated on CT (see the images below). Initially, nonselective pelvic angiography is performed from a catheter in the lower abdominal aorta. The hypogastric artery of interest is selected, and selective hypogastric angiography is performed. Microcatheters are needed for superselective angiography and embolization. Brisk hemorrhage may be evident on nonselective pelvic angiogram, but subtle extravasation may require selective or subselective angiography for detection.
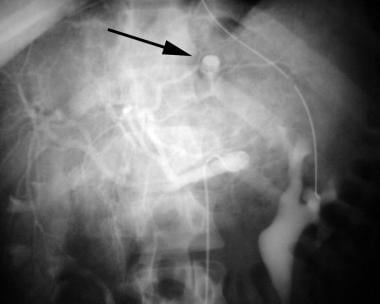
 Unsubtracted right iliac angiogram in a young woman who had evidence of continued hemorrhage from a pelvic fracture and/or dislocation following a motor vehicle accident. Mass effect from a large right-sided pelvic hematoma is identified compressing and displacing the urinary bladder to the left.
Unsubtracted right iliac angiogram in a young woman who had evidence of continued hemorrhage from a pelvic fracture and/or dislocation following a motor vehicle accident. Mass effect from a large right-sided pelvic hematoma is identified compressing and displacing the urinary bladder to the left.
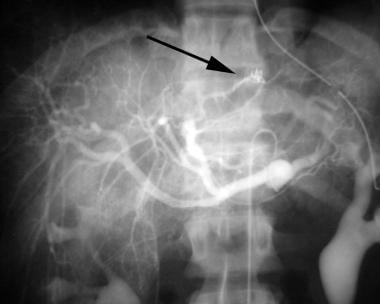
 Digital subtraction right iliac angiogram (same patient as in the previous image) demonstrating acute extravasation (arrows) from the right superior and inferior lateral sacral arteries, arising off of the posterior division of the right hypogastric artery.
Digital subtraction right iliac angiogram (same patient as in the previous image) demonstrating acute extravasation (arrows) from the right superior and inferior lateral sacral arteries, arising off of the posterior division of the right hypogastric artery.
 Right iliac artery angiogram (early phase) following transcatheter embolization of lateral sacral arteries showing no further extravasation from these vessels. Some inadvertent embolic occlusion of the posterior division of the right hypogastric artery also is evident (same patient as in the previous 2 images).
Right iliac artery angiogram (early phase) following transcatheter embolization of lateral sacral arteries showing no further extravasation from these vessels. Some inadvertent embolic occlusion of the posterior division of the right hypogastric artery also is evident (same patient as in the previous 2 images).
 Right iliac artery angiogram (late phase) following transcatheter embolization of lateral sacral arteries, showing no further extravasation from these vessels. An acute extravasation now is identified from the right internal pudendal artery (arrow; same patient as in the previous 3 images).
Right iliac artery angiogram (late phase) following transcatheter embolization of lateral sacral arteries, showing no further extravasation from these vessels. An acute extravasation now is identified from the right internal pudendal artery (arrow; same patient as in the previous 3 images).
 Final postembolization right iliac study showing occlusion of much of the posterior division and internal pudendal artery of the right hypogastric artery. No extravasation is evident (same patient as in the previous 4 images).
Final postembolization right iliac study showing occlusion of much of the posterior division and internal pudendal artery of the right hypogastric artery. No extravasation is evident (same patient as in the previous 4 images).
 Final postembolization right iliac study showing occlusion of much of the posterior division and internal pudendal artery of the right hypogastric artery. No extravasation is evident (same patient as in the previous 5 images).
Final postembolization right iliac study showing occlusion of much of the posterior division and internal pudendal artery of the right hypogastric artery. No extravasation is evident (same patient as in the previous 5 images).
Pelvic transcatheter embolization technique is as follows:
-
If possible, and when the source of extravasation is defined, superselective embolization with gelatin sponge pledgets of 1-2 mm in diameter or slurry is optimal.
-
Proximal coil embolization is less attractive for distal extravasation because it makes future access difficult (should it be needed) and because the exuberant distal collateralization of the pelvic vasculature renders this technique ineffective.
-
Proximal coil embolization for proximal hypogastric artery injury should be performed; it may be performed after embolization with distal gelatin sponge pledgets.
-
In patients with massive hemorrhage, nonselective embolization using gelatin sponge pledgets from the hypogastric artery position is acceptable; with this approach, bleeding may be quickly arrested.
-
Empirical embolization of both hypogastric arteries may be performed if no bleeding site is identified on angiography but there is clinical or CT evidence of hemorrhage.
-
A postembolization nonselective angiogram should be performed to exclude additional extravasation sites and to ensure that collateral vessels are not causing retrograde (backfill) hemorrhage; in such cases, further embolization is required.
Pelvic transcatheter embolization complications include the following:
-
Inadvertent embolization — Occurs only rarely, provided catheter position is satisfactory and the embolization procedure is terminated once occlusion is established.
-
Ischemic tissue necrosis or infarction — Occurs only rarely, provided particle sizes remain larger than 500 microns, in cases involving extensive distal collateralization of the pelvic vasculature
-
Impotence in men — Difficult to differentiate from impotence of neurogenic etiology related to injuries to the lumbosacral plexus
Peripheral Vascular Trauma
Peripheral vascular trauma is relatively common with penetrating injuries. In nonpenetrating peripheral vascular injuries (such as those that occur with blunt trauma), crush injuries, injuries associated with displaced skeletal fractures and joint dislocations, and degloving injuries are seen more often (see the images below). [83, 84, 85, 86, 87]
 Cut-film angiogram of a young man with an expanding hematoma following a stab wound to the right thigh. Extravasation (arrow) is identified from a medial muscular branch of the right profunda femoral artery (Courtesy of Dr Robert D'Agostino).
Cut-film angiogram of a young man with an expanding hematoma following a stab wound to the right thigh. Extravasation (arrow) is identified from a medial muscular branch of the right profunda femoral artery (Courtesy of Dr Robert D'Agostino).
 Postembolization angiogram of descending right profunda femoral artery branch demonstrating successful embolic occlusion of the medial muscular branch with a microcoil (arrow). The contrast material extravasation occurred prior to the embolic occlusion (same patient as in the previous image; courtesy of Dr Robert D'Agostino).
Postembolization angiogram of descending right profunda femoral artery branch demonstrating successful embolic occlusion of the medial muscular branch with a microcoil (arrow). The contrast material extravasation occurred prior to the embolic occlusion (same patient as in the previous image; courtesy of Dr Robert D'Agostino).
 Digital subtraction left lower extremity angiogram of a young man who presented with continuous hemorrhage from open wounds of his left calf. He had previously been treated with a fasciotomy after sustaining trauma to his left leg following a pedestrian-vs-automobile encounter. Extravasation (arrow) from the proximal left peroneal artery is present. The peroneal artery provides the only arterial runoff down the leg.
Digital subtraction left lower extremity angiogram of a young man who presented with continuous hemorrhage from open wounds of his left calf. He had previously been treated with a fasciotomy after sustaining trauma to his left leg following a pedestrian-vs-automobile encounter. Extravasation (arrow) from the proximal left peroneal artery is present. The peroneal artery provides the only arterial runoff down the leg.
 Unsubtracted left lower extremity angiogram (same patient as in the previous image) demonstrating the extravasation from the left peroneal artery (arrow) and the extension into the calf
Unsubtracted left lower extremity angiogram (same patient as in the previous image) demonstrating the extravasation from the left peroneal artery (arrow) and the extension into the calf
 Final postembolization left lower extremity angiogram following placement of a detachable microcoil (arrow) within the rent of the left peroneal artery, which preserved flow down the left leg. No further extravasation is identified (same patient as in the previous 2 images).
Final postembolization left lower extremity angiogram following placement of a detachable microcoil (arrow) within the rent of the left peroneal artery, which preserved flow down the left leg. No further extravasation is identified (same patient as in the previous 2 images).
Catheter angiography is indicated in cases of known or suspected peripheral vascular injury when the location of the injury is not certain, when multiple injury sites may be present, when the diagnosis requires confirmation, or when transcatheter treatment may be the therapy of choice.
The mechanisms of injury differ for penetrating trauma and blunt trauma. In penetrating trauma, the vascular injury may be produced by the direct penetration of the object through the vessel, with resulting disruption, or by dissipation of kinetic energy within the tissues adjacent to the vessel. In the case of low-velocity objects such as knives, the object must traverse the vessel, and the object must penetrate it to cause injury.
In injuries caused by high-velocity weapons such as hunting rifles and assault weapons, the object does not need to penetrate the vessel to cause damage. With high-velocity objects, kinetic energy is expelled and dissipated within the surrounding tissues as the object decelerates. This causes shock waves and cavitation, which produce injury within the local soft tissues. High-power penetrating objects may produce injury to vessels within a 10 cm radius of the trajectory. These are termed proximity injuries. Any of these mechanisms may cause laceration, pseudoaneurysm formation, transection, arteriovenous fistula, or thrombosis of the vessel. [88]
In blunt trauma, shearing and direct compression forces are involved. A direct compression or crushing force may produce an injury such as a mural contusion. The shearing mechanism, which occurs with stretching or traction forces, produces complete transection or intimal or medial dissection, which may result in the formation of a pseudoaneurysm. In addition, severe extrinsic compression from such entities as an adjacent hematoma, a fracture fragment, a dislocation, or edema, may cause severe narrowing of the vessel, which in turn may result in thrombosis. Vasospasm may occur as an isolated injury or in association with the above-mentioned vascular insults.
Many peripheral vascular injuries may be treated by transcatheter embolization or with the placement of a stent or a stent-graft placement. [89, 90]
Imaging studies
Major indications for catheter angiography include the following:
-
Active arterial bleeding or expanding hematoma
-
Peripheral pulse deficit
-
Bruit over the site of injury
-
Isolated neurologic deficit
-
Hypotension or other sign of ongoing hemorrhage
Minor indications for catheter angiography include the following:
-
Proximity of a wound or trajectory to a major blood vessel
-
Nonexpanding hematoma
-
Posterior dislocation of the knee joint and anterior dislocation of the elbow joint
Catheter angiography technique is as follows:
-
As in the evaluation of atherosclerotic disease, the principles of interrogation of inflow and outflow should be followed
-
A minimum of 2 angiographic views centered on the region of injury usually is required
-
Outflow should be examined to exclude a distal embolization from a proximal injury site
-
In gunshot injuries, angiography or fluoroscopy of the entire extremity should be undertaken to exclude embolization of metallic gunshot, shrapnel, or fragments
Treatment
For transcatheter embolization, the artery to be embolized must be nonessential or expendable. This is an alternative to surgical ligation. It provides optimal treatment when surgical access is limited or difficult and requires ligation of additional collateral arteries.
Embolization may be performed for pseudoaneurysm and arteriovenous fistula. Embolization should be performed proximally and distally to the lesion to prevent backfilling through collateral vessels. Consideration should be given to embolizing the neck of a pseudoaneurysm or arteriovenous fistula to preserve the parent vessel.
For stents and stent-grafts, experience with stents in cases of trauma is limited. Stents have the potential to preserve injured arteries.
Vascular Trauma of the Neck
Most vascular injuries of the head and neck arise from penetrating trauma. Significant penetrating injuries usually require surgical exploration; however, patients with less accessible zone 1 and zone 3 penetrating neck injuries may benefit from angiographic screening and possible treatment, such as transcatheter embolization if the injury involves a branch of the external carotid artery (see the images below). [91, 92, 93, 94, 95, 96]
 Cut-film left subclavian angiogram in a young patient with a gunshot wound demonstrating a proximity injury of the left subclavian artery. A laceration causing extravasation is present. The projectile is located over the left shoulder joint (Courtesy of Dr Robert D'Agostino).
Cut-film left subclavian angiogram in a young patient with a gunshot wound demonstrating a proximity injury of the left subclavian artery. A laceration causing extravasation is present. The projectile is located over the left shoulder joint (Courtesy of Dr Robert D'Agostino).
 Digital subtraction angiogram of cervical right carotid arteries in a comatose 33-year-old man who sustained neck trauma in a snowmobile accident. Complete occlusion of the right internal carotid artery is present.
Digital subtraction angiogram of cervical right carotid arteries in a comatose 33-year-old man who sustained neck trauma in a snowmobile accident. Complete occlusion of the right internal carotid artery is present.
 Unsubtracted digital right cervical carotid angiogram (same patient as in the previous image) demonstrating occlusion of the right internal carotid artery
Unsubtracted digital right cervical carotid angiogram (same patient as in the previous image) demonstrating occlusion of the right internal carotid artery
 Digital subtraction left cervical carotid angiogram demonstrating traumatic injury of the left internal carotid artery, manifested by pseudoaneurysm formation and an intimal dissection (same patient as in the previous 2 images)
Digital subtraction left cervical carotid angiogram demonstrating traumatic injury of the left internal carotid artery, manifested by pseudoaneurysm formation and an intimal dissection (same patient as in the previous 2 images)
Early diagnosis and treatment of carotid and vertebral arteries improve neurologic outcome. Aggressive screening protocols may increase the diagnosis of these injuries; the failure to diagnose and treat these lesions may result in a devastating and permanent neurologic injury. The pathophysiology of blunt carotid and cervical injuries usually is dissection, which may result in a stenosis, pseudoaneurysm formation, or both. Extracranial internal carotid injuries are much more common than intracranial internal carotid injuries; they usually originate at the C2-C3 vertebral level and terminate at the base of the carotid canal.
Historically, treatment of blunt injuries of the carotid and vertebral arteries included anticoagulation and antiplatelet therapy, although some patients required surgical repair. Successful management and definitive treatment of blunt internal carotid artery injuries have been reported with endovascular stents. [97, 98] Unilateral injuries of the vertebral artery often are treated with transcatheter embolization; such treatment requires that the contralateral vertebral artery be patent and of normal appearance.
The grading scale for blunt carotid arterial injury is as follows:
-
Grade I — Luminal irregularity or dissection with less than 25% luminal narrowing
-
Grade II — Dissection or intramural hematoma with luminal narrowing of 25% or more; intramural thrombus; or raised intimal flap
-
Grade III — Pseudoaneurysm
-
Grade IV — Occlusion
-
Grade V — Transection with free extravasation
The findings associated with blunt carotid or vertebral injury are as follows:
-
Expanding cervical hematoma
-
Hemorrhage from mouth, nose, ears, or wounds
-
Massive facial fractures
-
Cervical bruit in patients younger than 50 years
-
Evidence of stroke on CT
-
Unexplained or incongruous central or lateralizing neurologic deficit, anisocoria, Horner syndrome, transient ischemic attack, or amaurosis fugax
-
Basilar skull fracture through or near the carotid canal
-
Fracture through the foramen transversarium
-
Severe flexion or extension fracture or subluxation of the cervical spine
Imaging studies
Conventional catheter angiography remains the standard of reference to which all other imaging modalities are compared. Advantages include accuracy and facilitation of treatment through transcatheter embolization or endovascular stent or stent-graft placement. Disadvantages include the fact that it is not universally available in a timely fashion; it is invasive, with a small risk of catheter-induced stroke; and it is expensive.
Ultrasonography requires less experience in the trauma setting; it can be quickly performed and is inexpensive; and it is portable and therefore can be used at the bedside. However, it is operator dependent and is less effective in zone 1 and zone 3 injuries and injuries of the vertebral artery.
Magnetic resonance angiography requires little experience in the acute trauma setting. It may be used in conjunction with imaging of the CNS and does not require administration of iodinated contrast material. However, it is susceptible to motion artifact; it requires MRI-compatible life-support devices; it is not universally available; and its efficacy is not yet proven.
CT angiography evaluation often is obtained in stable trauma patients. It provides fast imaging from aortic arch to intracerebral vasculature and may be used in conjunction with imaging of the CNS and spine. It does, however, require iodinated contrast material; it is not universally available; and its efficacy has not been proven.
-
Digital subtraction catheter aortogram (early phase) of a typical acute traumatic aortic injury.
-
Digital subtraction catheter aortogram (late phase) of a typical acute traumatic aortic injury (same patient as in the previous image).
-
Contrast-enhanced CT of acute traumatic aortic injury.
-
Contrast-enhanced CT of acute traumatic aortic injury (same patient as in the previous image).
-
A 3-dimensional reconstruction of contrast-enhanced CT of acute traumatic aortic injury (same patient as in the previous 2 images).
-
Digital subtraction catheter aortogram of acute traumatic aortic injury (same patient as in the previous 3 images).
-
Vascular and solid organ trauma. Contrast-enhanced CT of the abdomen in a hemodynamically stable patient with evidence of persistent hemorrhage following a motor vehicle accident. Arrow points to contrast extravasation in a lacerated spleen (Courtesy of the Society of Cardiovascular and Interventional Radiology).
-
Vascular and solid organ trauma. Celiac angiogram (same patient as in the previous image) showing 3 foci of extravasation in spleen, 2 in the upper pole (arrow) and 1 in the lateral aspect of the mid spleen (arrow; courtesy of the Society of Cardiovascular and Interventional Radiology).
-
Vascular and solid organ trauma. Post—super-selective embolization splenic angiogram demonstrating microcoils in good position and no evidence of further extravasation (same patient as in the previous 2 images; courtesy of the Society of Cardiovascular and Interventional Radiology).
-
Contrast-enhanced CT demonstrating a liver laceration in a patient who sustained blunt abdominal trauma (Courtesy of Dr Robert D'Agostino).
-
Vascular and solid organ trauma. Hepatic angiogram (same patient as in the previous image) showing a pseudoaneurysm of a branch of the left hepatic artery (arrow) located in the region of the hepatic laceration (Courtesy of Dr Robert D'Agostino).
-
Vascular and solid organ trauma. Postembolization angiogram of left hepatic branch artery pseudoaneurysm. The coil (arrow) is in satisfactory position and is occluding the pseudoaneurysm (same patient as in the previous 2 images; courtesy of Dr Robert D'Agostino).
-
Contrast-enhanced CT of a 65-year-old woman with a remote history of blunt abdominal trauma and severe abdominal pain. A large pseudoaneurysm is present and is associated with an infarcted segment of the liver.
-
Vascular and solid organ trauma. Hepatic angiogram (same patient as in the previous image) demonstrates large bilobed pseudoaneurysm of right hepatic artery. Notice the "jet effect" of contrast material extending from the lower to the upper pseudoaneurysm sac. In addition, an aneurysm of the proper hepatic artery and diffuse ectasia of the proximal right hepatic artery are apparent.
-
Vascular and solid organ trauma. Fluoroscopic control image (same patient as in the previous 2 images) showing a catheter in the lower component of the bilobed pseudoaneurysm. Multiple stainless steel embolization coils have been deposited into the pseudoaneurysm.
-
Vascular and solid organ trauma. Immediate postembolization hepatic angiogram demonstrating occlusion of the complex right hepatic artery, pseudoaneurysm, and back thrombosis of the entire right hepatic artery (same patient as in the previous 3 images).
-
Vascular and solid organ trauma. Contrast-enhanced 5-month follow-up CT (same patient as in the previous 4 images) demonstrating coils in shrunken pseudoaneurysm sac and scarring in region of previous hepatic infarction.
-
Vascular and solid organ trauma. Celiac angiogram 5-month follow-up image (same patient as in the previous 5 images) showing occlusion of pseudoaneurysm and entire right hepatic, left hepatic, and common hepatic arteries.
-
A 30-year-old woman who sustained blunt abdominal trauma. Contrast-enhanced CT demonstrates a large perirenal hematoma and a fractured right kidney. CT evidence of acute extravasation is present.
-
Selective renal angiogram (same patient as in the previous image) reveals a vascular pedicle injury with an avulsed renal artery branch, multiple renal artery branch occlusions, and an inhomogeneous nephrogram but no active extravasation. Major devascularization is present. The patient had signs of persistent hemorrhage and was hypotensive.
-
Immediate postembolization renal angiogram demonstrates a satisfactory position of stainless steel coils effectively occluding the main right renal artery. A surgical nephrectomy was planned (same patient as in the previous 2 images).
-
Selective left renal angiogram in an older man with an expanding retroperitoneal hematoma. This was secondary to penetrating trauma to the flank following an encounter with an angry bull. The arrow delineates the avulsed left renal artery branch to the upper pole of the left kidney (Courtesy of Dr Kenneth E Najarian).
-
Control angiogram (same patient as in the previous image) obtained immediately before deployment of a custom-made stent -graft across the origin of the avulsed left renal artery branch. The balloon-mounted stent-graft is in a good position and is ready to be deployed (Courtesy of Dr Kenneth E Najarian).
-
Post–stent-graft deployment left renal angiogram (same patient as in the previous 2 images). The avulsed branch artery has been excluded effectively (Courtesy of Dr Kenneth E Najarian).
-
Contrast-enhanced CT in a 9-year-old boy who sustained blunt abdominal injury after falling onto the handle bar of his bicycle. He presented with exsanguinating hematuria caused by a fractured left kidney. CT demonstrates a pseudoaneurysm (arrow) off of an intrarenal artery branch.
-
Left renal angiogram (early phase; same patient as in the previous image shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
-
Left renal angiogram (late phase; same patient as in the previous 2 images) shows the faint opacification of a pseudoaneurysm (arrow), which correlates with the CT finding.
-
Postembolization left renal angiogram (same patient as in the previous 3 images) shows stainless steel embolization coil (arrow) completely occluding the renal artery branch previously containing the pseudoaneurysm.
-
Unsubtracted right iliac angiogram in a young woman who had evidence of continued hemorrhage from a pelvic fracture and/or dislocation following a motor vehicle accident. Mass effect from a large right-sided pelvic hematoma is identified compressing and displacing the urinary bladder to the left.
-
Digital subtraction right iliac angiogram (same patient as in the previous image) demonstrating acute extravasation (arrows) from the right superior and inferior lateral sacral arteries, arising off of the posterior division of the right hypogastric artery.
-
Right iliac artery angiogram (early phase) following transcatheter embolization of lateral sacral arteries showing no further extravasation from these vessels. Some inadvertent embolic occlusion of the posterior division of the right hypogastric artery also is evident (same patient as in the previous 2 images).
-
Right iliac artery angiogram (late phase) following transcatheter embolization of lateral sacral arteries, showing no further extravasation from these vessels. An acute extravasation now is identified from the right internal pudendal artery (arrow; same patient as in the previous 3 images).
-
Final postembolization right iliac study showing occlusion of much of the posterior division and internal pudendal artery of the right hypogastric artery. No extravasation is evident (same patient as in the previous 4 images).
-
Final postembolization right iliac study showing occlusion of much of the posterior division and internal pudendal artery of the right hypogastric artery. No extravasation is evident (same patient as in the previous 5 images).
-
Cut-film angiogram of a young man with an expanding hematoma following a stab wound to the right thigh. Extravasation (arrow) is identified from a medial muscular branch of the right profunda femoral artery (Courtesy of Dr Robert D'Agostino).
-
Postembolization angiogram of descending right profunda femoral artery branch demonstrating successful embolic occlusion of the medial muscular branch with a microcoil (arrow). The contrast material extravasation occurred prior to the embolic occlusion (same patient as in the previous image; courtesy of Dr Robert D'Agostino).
-
Digital subtraction left lower extremity angiogram of a young man who presented with continuous hemorrhage from open wounds of his left calf. He had previously been treated with a fasciotomy after sustaining trauma to his left leg following a pedestrian-vs-automobile encounter. Extravasation (arrow) from the proximal left peroneal artery is present. The peroneal artery provides the only arterial runoff down the leg.
-
Unsubtracted left lower extremity angiogram (same patient as in the previous image) demonstrating the extravasation from the left peroneal artery (arrow) and the extension into the calf
-
Final postembolization left lower extremity angiogram following placement of a detachable microcoil (arrow) within the rent of the left peroneal artery, which preserved flow down the left leg. No further extravasation is identified (same patient as in the previous 2 images).
-
Cut-film left subclavian angiogram in a young patient with a gunshot wound demonstrating a proximity injury of the left subclavian artery. A laceration causing extravasation is present. The projectile is located over the left shoulder joint (Courtesy of Dr Robert D'Agostino).
-
Digital subtraction angiogram of cervical right carotid arteries in a comatose 33-year-old man who sustained neck trauma in a snowmobile accident. Complete occlusion of the right internal carotid artery is present.
-
Unsubtracted digital right cervical carotid angiogram (same patient as in the previous image) demonstrating occlusion of the right internal carotid artery
-
Digital subtraction left cervical carotid angiogram demonstrating traumatic injury of the left internal carotid artery, manifested by pseudoaneurysm formation and an intimal dissection (same patient as in the previous 2 images)
-
Infarcted Left Kidney