Practice Essentials
Bone infarct, or osteonecrosis, refers to ischemic death of the cellular elements of the bone and marrow. A considerable lack of uniformity exists in the use of terminology for bone infarct. At present, the term osteonecrosis is accepted and used widely. In general, bone infarct refers to lesions occurring in the metaphysis and diaphysis of bone. Lesions in the epiphysis are called avascular necrosis (AVN). [1, 2, 3, 4] Osteonecrosis can be idiopathic or secondary to a number of conditions that reduce blood supply to the bone; such conditions include an intraluminal abnormality, an extrinsic compression, or a combination of both.
Osteonecrosis can occur in any bone but most commonly affects the hip. If osteonecrosis is identified in an area other than the hip, the hip should be evaluated clinically and with radiographic and other imaging studies. The plain radiograph can remain normal for months after onset of symptoms such as groin pain. Earliest radiographic findings include mild density changes, sclerosis, and cysts. These can then progress to the pathognomonic crescent sign (ie, subchondral radiolucency in the anterolateral aspect of the proximal femoral head) from subchondral collapse and loss of sphericity (ie, measurement of roundness) or collapse of the femoral head. Key radiographic features to look for include precollapse versus postcollapse; size of lesion; and amount of head depression. [5]
CT scans, MRIs, and bone scans play a significant role in diagnosing the disease at an early stage and thereby reducing the number and/or severity of complications and morbidity associated with the disease.
(See the images below.)
 Lateral view of the knee in a deep-sea diver shows dysbaric osteonecrosis in the diaphysis of the femur and tibia. Note the irregular calcific deposits with a shell-like pattern, which is typical of a bone infarct.
Lateral view of the knee in a deep-sea diver shows dysbaric osteonecrosis in the diaphysis of the femur and tibia. Note the irregular calcific deposits with a shell-like pattern, which is typical of a bone infarct.
 Plain radiograph in a middle-aged man with shoulder discomfort demonstrates an irregularly calcified bone infarct in the diametaphysis of the right humerus.
Plain radiograph in a middle-aged man with shoulder discomfort demonstrates an irregularly calcified bone infarct in the diametaphysis of the right humerus.
 Coronal T1-weighted MRI in a 12-year-old boy with early Legg-Calvé-Perthes disease demonstrates slight irregularity of the right femoral capital epiphysis with abnormal signal intensity. The left hip appears normal.
Coronal T1-weighted MRI in a 12-year-old boy with early Legg-Calvé-Perthes disease demonstrates slight irregularity of the right femoral capital epiphysis with abnormal signal intensity. The left hip appears normal.
 Radioisotopic bone scan of the right humerus in a patient with pancreatitis shows a hot lesion, the result of revascularization, which is a part of the reparative process.
Radioisotopic bone scan of the right humerus in a patient with pancreatitis shows a hot lesion, the result of revascularization, which is a part of the reparative process.
Imaging modalities
Plain radiography is not sensitive in the detection of bone infarction. However, plain radiography has a role in the differential diagnosis. Radionuclide imaging and MRI are much more sensitive than plain radiography and may show changes caused by altered hemodynamics early in the course of disease. CT scanning is complementary to the other techniques, but it is not as sensitive as radionuclide imaging or MRI. CT scans may demonstrate subtle trabecular irregularity with bone necrosis when plain radiographic findings are normal. [2, 6, 7, 8, 3, 4] Ultrasonography may be useful in differentiating bone infarction from osteomyelitis in patients with sickle cell disease. [9, 10, 11, 12, 13, 14, 15]
For osteonecrosis of the femoral head, MRI has become the imaging modality of choice because of its high sensitivity and specificity. Radionuclide bone scans are less sensitive and specific than MRI but can be used to detect inflammatory activity if MRI is contraindicated. [4, 7, 16, 17, 18, 8] In patients with spontaneous osteonecrosis of the knee, diagnosis can be difficult because of the time before typical changes appear. MRI may provide an earlier diagnosis than other modalities. [16, 17, 18]
After the femoral head, osteonecrosis of the humeral head is the most common site for nontraumatic osteonecrosis. Early detection affects the prognosis, and shoulder osteonecrosis is not always visible on radiographs. Patients with clinically suspected humeral head osteonecrosis and negative radiographs should undergo MRI. [19]
The American College of Radiology has published the following recommendations [20] :
-
The initial imaging modality for suspected osteonecrosis is radiography.
-
For suspected osteonecrosis following normal or inconclusive radiographs, MRI without IV contrast is usually appropriate. CT may be used, although there is insufficient evidence to determine the benefits of this imaging modality.
-
For preoperative planning following radiographic evidence of articular collapse, MRI or CT is usually appropriate.
Limitations of techniques
No radiologic findings are specific for bone infarction. A variety of pathologies may mimic bone infarction, including stress fractures, infections, inflammations, and metabolic and neoplastic processes. A bone infarct may mimic a bone tumor on imaging. The limitations apply to all imaging modalities, including plain radiography, radionuclide studies, CT, and MRI. However, when the global picture is considered, including the history, clinical findings, and course of events, the diagnosis can be achieved with the help of imaging in most patients. [1]
Staging
Classification systems include Ficat and Arlet, Steinberg, the Association Research Circulation Osseous (ARCO), and the Japanese Investigation Committee (JIC). [2, 4, 7, 21, 22]
Steinberg has classified the radiologic appearance into 6 stages, as follows [2, 7, 21] :
-
Stage 0: normal findings are demonstrated.
-
Stage I: the appearance may vary from normal to subtle trabecular mottling, but an isotopic bone scan or MRI shows abnormal bone.
-
Stage II: stage IIa - focal radiopacity is associated with osteopenia; stage IIb - radiopacity is associated with osteoporosis and an early crescent sign.
-
Stage III: stage IIIa - an established crescent sign is associated with cyst formation; stage IIIb - mild alteration in the configuration of the femoral head is caused by a subchondral fracture, but the joint space is maintained.
-
Stage IV: marked collapse of the femoral head is demonstrated with an associated acetabular abnormality.
-
Stage V: joint space narrowing is demonstrated with changes of secondary osteoarthrosis.
The Ficat and Arlet classification is as follows [23, 24, 25, 26] :
Stage 0
-
Plain radiograph: normal
-
MRI: normal
-
Clinical symptoms: nil
Stage I
-
Plain radiograph: normal or minor osteopenia
-
MRI: edema
-
Bone scan: increased uptake
-
Clinical symptoms: pain typically in the groin
Stage II
-
Plain radiograph: mixed osteopenia and/or sclerosis and/or subchondral cysts, without any subchondral lucency (crescent sign)
-
MRI: geographic defect
-
Bone scan: increased uptake
-
Clinical symptoms: pain and stiffness
Stage III
-
Plain radiograph: crescent sign and eventual cortical collapse
-
MRI: same as plain radiograph
-
Clinical symptoms: pain and stiffness +/- radiation to knee and limp
Stage IV
-
Plain radiograph: end-stage with evidence of secondary degenerative change
-
MRI: same as plain radiograph
-
Clinical symptoms: pain and limp
The ARCO classification is as follows [27, 28] :
Stage 0
-
Plain radiograph: normal
-
MRI: normal
-
Clinically: no symptoms
Stage I
-
Plain radiograph: normal
-
MRI or bone scan: abnormal
-
Clinically: no symptoms or presence symptoms
Stage II
-
Plain radiograph: trabecular bone changes without changes in subchondral bone; preserved joint space
-
MRI: abnormal, diagnostic appearance
-
Clinically: symptoms present
Stage III
-
Presence of trabecular bone changes and subchondral fracture (crescent sign or subchondral bone collapse); preserved joint space
-
Clinically: symptoms present
-
Further subdivided with regard to the depth of femoral head depression: IIIA - depression ≤2 mm; IIIB - depression >2 mm
Stage IV
-
Features of osteoarthritis, with distorted femoral head shape, acetabular changes, and narrowed joint space
-
Clinically: symptoms present
In a study by Lee et al of 308 hips classified as ARCO (Association Research Circulation Osseous) stage I or II on simple radiography, 20.5% (63 hips) were found to be stage III on CT imaging. Therefore, according to the authors, when a joint-preserving treatment is considered for early stage osteonecrosis of the femoral head, CT examination is necessary for more precise staging of the disease. [29]
Radiography
Plain radiographic findings in established osteonecrosis may be characteristic of the disease. In the epiphyseal region, an arclike, subchondral, lucent lesion may be associated with areas of patchy loss of bone opacity intermingled with sclerotic areas and bone collapse. In the diametaphyseal region, a sheetlike lucency of varying size is usually surrounded by shell-like sclerosis and/or calcification and periostitis. In flat or complex bones, patchy lucencies and sclerosis are often associated with bone collapse or fractures (see the images below). Radiographic features of bone infarction do not occur until several months after the onset of symptoms; therefore, plain radiography is not a sensitive technique in the detection of bone infarction. However, plain radiography has a role in the differential diagnosis.
 Plain radiograph in a middle-aged man with shoulder discomfort demonstrates an irregularly calcified bone infarct in the diametaphysis of the right humerus.
Plain radiograph in a middle-aged man with shoulder discomfort demonstrates an irregularly calcified bone infarct in the diametaphysis of the right humerus.
 Plain radiograph in a 68-year-old man with hip pain demonstrates patchy sclerosis of both femoral heads that is consistent with avascular necrosis.
Plain radiograph in a 68-year-old man with hip pain demonstrates patchy sclerosis of both femoral heads that is consistent with avascular necrosis.
 Plain radiograph of the pelvis in a man demonstrates collapse of the left femoral head due to osteonecrosis.
Plain radiograph of the pelvis in a man demonstrates collapse of the left femoral head due to osteonecrosis.
 Plain radiograph of the right knee joint in a 52-year-old woman with abrupt onset of right knee pain demonstrates subtle loss of bone density in the proximal aspect of the tibia (arrow).
Plain radiograph of the right knee joint in a 52-year-old woman with abrupt onset of right knee pain demonstrates subtle loss of bone density in the proximal aspect of the tibia (arrow).
 Plain radiograph of the left wrist in a man with posttraumatic osteonecrosis of the scaphoid bone shows sclerosis of the proximal portion of the scaphoid bone.
Plain radiograph of the left wrist in a man with posttraumatic osteonecrosis of the scaphoid bone shows sclerosis of the proximal portion of the scaphoid bone.
 Plain radiograph of the right wrist of a man demonstrates sclerosis, irregularity, and collapse of the lunate bone consistent with osteonecrosis Kienböck disease.
Plain radiograph of the right wrist of a man demonstrates sclerosis, irregularity, and collapse of the lunate bone consistent with osteonecrosis Kienböck disease.
 Osteonecrosis of the third metatarsal head (ie, Freiberg disease) in a 60-year-old woman is shown as flattening of the third metatarsal head, widening of the third metatarsal, and expansion of the corresponding proximal phalangeal base.
Osteonecrosis of the third metatarsal head (ie, Freiberg disease) in a 60-year-old woman is shown as flattening of the third metatarsal head, widening of the third metatarsal, and expansion of the corresponding proximal phalangeal base.
 Plain radiograph of the left ankle in an adult patient with osteonecrosis of the talus. Note the increased radiopacity of the body of the talus.
Plain radiograph of the left ankle in an adult patient with osteonecrosis of the talus. Note the increased radiopacity of the body of the talus.
 Plain abdominal radiograph in a patient with sickle cell disease shows generalized coarsening of the bone trabeculae with characteristic H-shaped vertebrae due to a growth disturbance. Note the calcified and contracted spleen.
Plain abdominal radiograph in a patient with sickle cell disease shows generalized coarsening of the bone trabeculae with characteristic H-shaped vertebrae due to a growth disturbance. Note the calcified and contracted spleen.
 Lateral view of the knee in a deep-sea diver shows dysbaric osteonecrosis in the diaphysis of the femur and tibia. Note the irregular calcific deposits with a shell-like pattern, which is typical of a bone infarct.
Lateral view of the knee in a deep-sea diver shows dysbaric osteonecrosis in the diaphysis of the femur and tibia. Note the irregular calcific deposits with a shell-like pattern, which is typical of a bone infarct.
Posttraumatic osteonecrosis
Posttraumatic osteonecrosis usually follows a fracture; most cases occur in areas with vulnerable blood supply, such as the femoral head, humeral head, talus, or scaphoid bone (see the image below).
 Posttraumatic osteonecrosis of the right femoral head in a woman. Note the arclike subchondral radiolucency secondary to subchondral fracture and collapse.
Posttraumatic osteonecrosis of the right femoral head in a woman. Note the arclike subchondral radiolucency secondary to subchondral fracture and collapse.
Infarcted bone appears opaque as a result of compression. The femoral head is the most common site of osteonecrosis, which is a well-known complication of femoral head fractures and dislocations. Additionally, subchondral fracture of the femoral head has been associated with osteonecrosis, transient osteoporosis of the hip, and Pastel disease (ie, rapidly progressing osteoarthritis of the hip).
Radiographs obtained several months after the onset of symptoms may show a radiolucent crescent parallel to the articular surface secondary to subchondral collapse of the necrotic bone. Often, flattening of the articular surface is demonstrated, but the joint space tends to be preserved. The opacity of the infarcted femoral head is increased.
Radiographic changes in traumatic osteonecrosis of the talus are delayed (by 1-3 mo) and become apparent with osteoporosis of the surrounding bones, which creates relatively increased opacity in the body of the talus. The increase in radiopacity may be associated with a collapse of the articular surface.
Occasionally, a subchondral radiolucent band is demonstrated in the proximal talus; this finding is related to bone resorption. This Hawkins impingement sign usually indicates the presence of viable bone with an intact blood supply (see the image below).
 Plain radiograph of the left ankle in a patient with ankle injury demonstrates subchondral radiolucent band (arrow) in proximal talus, the Hawkins impingement sign, which represents bone resorption and an intact blood supply.
Plain radiograph of the left ankle in a patient with ankle injury demonstrates subchondral radiolucent band (arrow) in proximal talus, the Hawkins impingement sign, which represents bone resorption and an intact blood supply.
Osteonecrosis of the humeral head is usually a complication of a fracture of the anatomic neck or severe fracture dislocation. Radiographic findings are delayed; they include flattening, sclerosis, and irregularity of part of the articular surface of the humeral head.
In the scaphoid bone, 10-15% of the fractures are complicated by osteonecrosis in the proximal pole of the scaphoid bone. Plain radiographic findings include relatively increased opacity in the infarcted pole of the scaphoid bone. This appearance may be delayed for 4-8 weeks, a period possibly associated with delayed union or nonunion of the fracture; collapse of the infarcted part of the bone; and, eventually, changes related to secondary osteoarthrosis.
Osteonecrosis of the capitate may occur after accidental or occupational trauma. The proximal part of the capitate is the site of AVN. After trauma or prolonged stress, AVN also may affect the lunate; the other carpal bones; the tarsal navicular bone; the mandibular condyle; the patella; the glenoid region of the scapula; and, occasionally, the metatarsal bones.
Osteonecrosis of the vertebral body (ie, Kümmell disease) usually occurs weeks to years after acute trauma. It usually causes vertebral collapse in middle-aged or elderly men or women. Generally, the lower dorsal or upper lumbar vertebrae are involved. Gas may be apparent in the vertebral body and may extend into the psoas muscles. These changes are depicted more elegantly on CT scans than on other images.
Spontaneous infarction of the femoral head is uncommon and affects men more often than women in the group aged 40-70 years. Infarction may be unilateral or bilateral. The radiographic appearance depends on the severity of the disease. A minor form of femoral head infarction is recognized; this form affects a superficial area of the femoral head in a segmental distribution. The disease is nonprogressive. Radiographs may show a lobulated or segmental subcortical lucency, which may be surrounded by a sclerotic margin. The latter is better demonstrated on CT scans.
Spontaneous osteonecrosis
Spontaneous osteonecrosis around the adult knee (ie, Ahlbäck disease) is a distinct clinical entity that affects women more often than men. It commonly affects the medial femoral condyle and less commonly affects the medial or lateral tibial condyle. Initial radiographic findings are usually normal. Weeks or months later, subtle flattening and sclerosis of the weight-bearing femoral or tibial condyle may be seen. If untreated, further depression, sclerosis, and joint space narrowing occur. If the affected area is small, spontaneous recovery may ensue if weight-bearing is avoided.
Conventional tomography may show angular or wedge-shaped areas of patchy sclerotic bones and subtle collapse of the bone surface that is undetected on plain radiographs. The diagnosis of spontaneous osteonecrosis of the knee is being questioned. Current theories suggest that this entity is actually a subchondral stress fracture that most often occurs in the medial femoral condyle.
Spontaneous osteonecrosis of the tarsal navicular in adults (ie, Mueller-Weiss syndrome) may occur, especially in women. Plain radiographic features include medial or dorsal protrusion of a portion of the bone or the entire navicular bone.
These findings are often associated with a comma-shaped deformity caused by collapse of the lateral part of the bone. The disease may be bilateral or asymmetric and may be associated with pathologic fractures. The disease can be progressive at times, and it is associated with severe pain and disability. This syndrome is distinct from the osteochondrosis of the tarsal navicular bone that occurs in children (ie, Köhler disease).
Osteonecrosis secondary to Cushing disease
Osteonecrosis secondary to Cushing disease occurs as a result of excess levels of endogenous steroids. Most of the steroids are present in the vertebral bodies. Characteristic features are osteoporosis, osteosclerosis, subchondral radiolucent shadows, wedging and/or collapse, and bone fragmentation associated with a relatively normal articular space.
Gaucher disease
Osteonecrosis that affects the epiphysis and diaphysis is a known complication of Gaucher disease and is commonly associated with bone pain. In the long bones, bands of sclerosis and radiolucency alternate. These findings are associated with periostitis and a bone-within-bone appearance identical to that seen in sickle cell disease. [30]
Hemophilia
Osteonecrosis may complicate hemophilia and is usually found in the femoral head and talus (see the image below). Bone infarction results from intraosseous hemorrhage with the subsequent collapse of bone or intracapsular hemorrhage and an elevation in intra-articular pressure that causes vascular compromise and eventual osteonecrosis. Radiographic features are similar to those of traumatic osteonecrosis. Ossification related to bleeding in the periarticular region may be apparent.
 Plain abdominal radiograph in a 19-year-old man with hemophilia. Osteonecrosis of the right humeral head is associated with calcified hematoma in the left groin.
Plain abdominal radiograph in a 19-year-old man with hemophilia. Osteonecrosis of the right humeral head is associated with calcified hematoma in the left groin.
Caisson disease or dysbaric osteonecrosis
Two types of bone lesions that occur in patients with dysbaric osteonecrosis can be identified on plain radiographs: juxta-articular lesions, which are more common and mostly affect the head of the humerus and femur, and diaphyseal and metaphyseal lesions that occur at a distance from the joint.
Juxta-articular alterations are frequently encountered in the region of the head of the femur and humerus. They are depicted as radiopaque areas, spherical segmental radiopaque areas that may eventually produce a snow-capped appearance, radiolucent subcortical bands termed the crescent sign, and osseous collapse and fragmentation.
Diaphyseal and metaphyseal lesions are demonstrated as ill-defined radiopaque foci; irregular intraosseous areas of shell-like calcification; and, rarely, radiolucent defects. These changes may be unilateral or bilateral.
Pancreatitis
Osteonecrosis is a known complication of pancreatitis; it is usually associated with chronic or inactive forms of pancreatitis (see the image below). [31] Epiphyseal involvement is characterized by lucencies of mottled appearance or lucencies interspersed with sclerosis, subchondral radiolucent areas, and partial or complete collapse of the involved bone. Diaphyseal and metaphyseal involvement is associated with radiolucency, calcification, and periosteal new bone formation. The distal femur and the proximal tibia are the sites most commonly involved.
 Patchy irregular sclerotic lesion characteristic of bone infarct is seen in the proximal metadiaphysis of right humerus in a patient with pancreatitis.
Patchy irregular sclerotic lesion characteristic of bone infarct is seen in the proximal metadiaphysis of right humerus in a patient with pancreatitis.
Pregnancy
Osteonecrosis in pregnancy appears to be closely associated with childbirth. The femoral and humeral heads are the sites most commonly involved.
Systemic lupus erythematosus
The pathogenesis of osteonecrosis in patients with SLE is not clear, and the role of steroids is speculative. The overall radiographic appearances of bone infarcts are similar to those of infarcts in patients without SLE. The most commonly affected sites are the humeral head, femoral condyles, tibial plateaus, and talus. An unusual feature is the involvement of small bones of the wrist, hands, and feet; examples include the carpus, tarsus, and metatarsal and metacarpal heads.
Radiation-induced osteonecrosis
Exposure to internal or external, accidental, or diagnostic and/or therapeutic radiation may produce diverse osseous changes, including disruption of growth, bone infarction, scoliosis, and benign and malignant neoplasms. Osseous changes are usually related to dose and age. Various parts of the skeleton respond differently upon exposure to radiation. Most osseous changes result from secondary radiation exposure during radiation therapy for soft tissue cancers. Common sites of involvement include the mandible, skull, shoulder, sternum, and shoulder. The threshold for osseous radiation injury is believed to be 3000 cGy, with cell death occurring at 5000 cGy.
Radiation osteitis is manifested by a mottled appearance with a mixture of osteoporosis, increased opacity, and coarse trabecular pattern demonstrated on plain radiographs. Different bones develop radiation-induced changes at varying times after the initial insult. Mandibular osteonecrosis commonly appears 1 year after radiation exposure; at other sites, the latent period is longer. Osteonecrosis is considerably more common in the mandible than in other bones because of its compact bone structure and poor blood supply.
In addition, the mandible is exposed to a higher radiation dose because of its superficial location. Bone necrosis is usually mild and may be aseptic or associated with infection. Osteonecrosis appears as an ill-defined area of bone destruction without a sequestrum. An associated soft tissue mass is unusual with osteonecrosis; the presence of a soft tissue component suggests tumor recurrence.
Radiation necrosis of the skull usually occurs after a minimum radiation dose of 3500 cGy. The radiographic appearance is that of a mixed lytic and sclerotic area within the calvarium. If the osteonecrosis is associated with soft tissue necrosis, infection and/or osteomyelitis may ensue.
Osteonecrosis of the shoulder girdle may follow radiation therapy for breast carcinoma. Osteopenia is common after radiation therapy and is often associated with disorganized bone trabeculae that resemble findings in Paget disease. Pathologic rib fractures are common and often multiple. The edges of rib fractures show resorption, and the tips are often pointed or sclerotic. Clavicular and scapular fractures are often associated with these rib fractures.
Radiation necrosis of the humerus may develop as long as 7-10 years after radiation therapy. Changes include patchy bone resorption, fractures, and necrosis of the humeral head with a slipped proximal humeral head epiphysis.
Radiation necrosis of the sternum may follow treatment of breast cancer. Osseous changes may be mild and may be demonstrated as osteoporosis, abnormal trabecular patterns, localized lucencies, and sclerosis. More severe changes include abnormalities in alignment with localized pectus excavatum or complete necrosis of one or more segments of the sternum.
Unilateral or bilateral femoral neck fractures are reported in 2% of patients who are exposed to pelvic irradiation. These fractures are commonly subcapital. Often, sclerotic changes occur, and trabecular opacity increases in the femoral neck, preceding a fracture. Fractures usually heal normally with abundant callous formation. Protrusio acetabuli is also reported to occur after radiation therapy of the pelvis; this condition may be associated with peritoneal calcification. Changes indistinguishable from osteitis pubis may occur in the symphysis pubis.
Radionecrosis of the sacroiliac joints may cause widening and irregularity of the joint space. This condition is often associated with sclerosis, which is commonly symmetric and bilateral. Pathologic fractures of pelvic bones may occur after radiation therapy; these can involve the sacrum and may extend into one or both innominate bones.
Complications resulting from osteonecrosis
Complications from osteonecrosis usually are well depicted on plain radiographs. Cartilaginous abnormalities, such as fibrillation, erosions, and joint space narrowing, may affect joints. Changes of secondary osteoarthrosis may be apparent in cases involving significant collapse of an articular surface that occurs after an infarction. Loose bodies, either chondral or osteochondral, may be seen in a joint embedded within the depressed part of the bone or within the synovium.
Cystic degeneration in areas of bone infarction may occur, particularly in the diaphysis of tubular bones. Appearances are those of a well-marginated expanding osteolytic area eroding the cortex. The well-marginated cyst and the lack of cortical disruption help in differentiating the cyst from a malignant degeneration.
Malignant degeneration (eg, sarcoma) is a known complication of bone infarction irrespective of etiology. [32] Men are affected more often than women; patients are usually aged 40-70 years. Typically, the distal part of the femur or proximal tibia is involved, although other sites may be affected as well. The radiographic appearance is that of a soft tissue mass associated with bone destruction at a site of previous bone infarction.
Degree of confidence
Radiographic features of bone infarction do not occur until several months after the onset of symptoms; therefore, plain radiography is not a sensitive technique in the detection of bone infarction. However, plain radiography has a role in the differential diagnosis.
False positives/negatives
Early radiographic features of a bone infarct, particularly in the metaphyseal region of long bones, lack specificity. Vague areas of radiolucencies may mimic infections and neoplastic processes. Osteochondritis dissecans may mimic spontaneous osteonecrosis around the knee.
Radiographic findings in dysbaric osteonecrosis are indistinguishable from those of osteonecrosis resulting from other causes. Virtually identical features may be seen with bone islands. Osteonecrosis of the vertebral body may be difficult to differentiate from an osteoporotic fracture and vertebral collapse secondary to malignancy.
Cyst formation that occurs after bone infarction is occasionally difficult to differentiate from a malignant degeneration, particularly in early stages when the cysts are poorly marginated. Mimics of malignant degeneration of bone infarcts include fibrosarcoma, malignant fibrous histiocytoma, chondrosarcoma, and, rarely, osteosarcoma.
Radiation-induced mandibular osteonecrosis may be difficult to differentiate from tumor recurrence. Other regions of radiation osteonecrosis may mimic osteomyelitis. Radionecrosis of the shoulder girdle may mimic Paget disease. Changes indistinguishable from osteitis pubis may occur in the symphysis pubis, with radionecrosis. Radionecrosis of the sacroiliac joints may mimic osteitis condensans ilii.
Computed Tomography
CT scans demonstrate central or peripheral areas of reduced attenuation. Reformatted sagittal and coronal images show subchondral fractures and collapse of the articular surface. CT findings may show subtle trabecular irregularity associated with bone necrosis when plain radiographic findings are normal. Collapse or buckling of articular surfaces indicates more advanced disease and influences the choice of treatment.
As with conventional radiography, CT is not sensitive in the detection of bone infarcts. However, CT scans can help in diagnosing bone infarction earlier than would be the case with plain radiographs. The sensitivity of CT in the diagnosis of bone infarction is lower than that of MRI and bone scintigraphy.
As with plain radiography, early CT features of a bone infarct lack specificity, particularly in the metaphyseal region of the long bones. Vague radiolucencies may mimic infections and neoplastic processes.
Magnetic Resonance Imaging
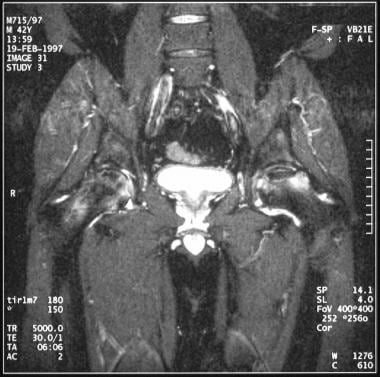
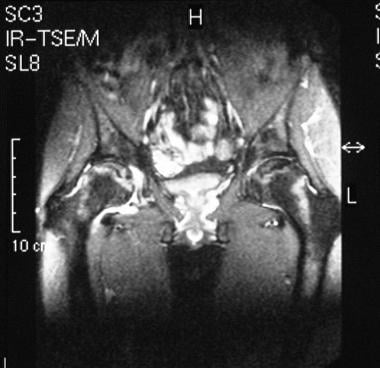
Ischemic bone changes become apparent in hematopoietic tissues on MRIs within 6-12 hours. Ischemia is detectable in osteophytes, osteoblasts, and osteoclasts within approximately 2 days. An inflammatory response surrounding the devascularized bone, resulting from increased vascularity and granulation tissue, is demonstrated well as an interface on MRIs. A risk of subsequent AVN is associated with the early conversion of active marrow to fatty marrow in the proximal femur and with prominent physeal scars that close off the femoral head (see the images below). [33, 14, 15]
 Coronal T1-weighted MRI in a 12-year-old boy with early Legg-Calvé-Perthes disease demonstrates slight irregularity of the right femoral capital epiphysis with abnormal signal intensity. The left hip appears normal.
Coronal T1-weighted MRI in a 12-year-old boy with early Legg-Calvé-Perthes disease demonstrates slight irregularity of the right femoral capital epiphysis with abnormal signal intensity. The left hip appears normal.
 Coronal T1 weighted MR image of a 20-year-old woman with bilateral late-stage Legg-Calvé-Perthes disease demonstrates flattening of the right femoral head and acetabulum.
Coronal T1 weighted MR image of a 20-year-old woman with bilateral late-stage Legg-Calvé-Perthes disease demonstrates flattening of the right femoral head and acetabulum.
 Coronal T1-weighted MRI of the left hip in the patient in the previous image, shows a short, broad femoral neck. This bone remodeling is associated with Legg-Calvé-Perthes disease.
Coronal T1-weighted MRI of the left hip in the patient in the previous image, shows a short, broad femoral neck. This bone remodeling is associated with Legg-Calvé-Perthes disease.
 Coronal T2-weighted MRI in a 35-year-old man with bilateral avascular necrosis of the hip demonstrates a central region of increased signal intensity and a peripheral region of decreased signal intensity. The double-line sign is characteristic of osteonecrosis.
Coronal T2-weighted MRI in a 35-year-old man with bilateral avascular necrosis of the hip demonstrates a central region of increased signal intensity and a peripheral region of decreased signal intensity. The double-line sign is characteristic of osteonecrosis.
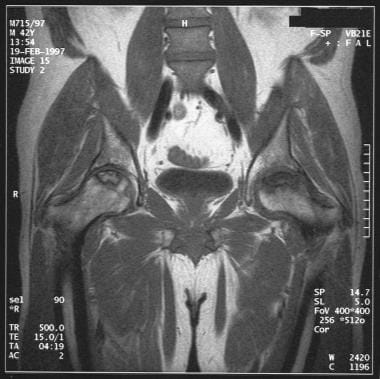 Coronal T1-weighted MRI in a 42-year-old man with bilateral avascular necrosis shows an area of osteonecrosis in both femoral heads in which a serpentine area of low signal intensity surrounds a central area of intermediate signal intensity similar to that of fat.
Coronal T1-weighted MRI in a 42-year-old man with bilateral avascular necrosis shows an area of osteonecrosis in both femoral heads in which a serpentine area of low signal intensity surrounds a central area of intermediate signal intensity similar to that of fat.
 Sagittal T1-weighted MRI of the cervical spine in a 37-year-old woman who underwent radiation therapy for a slow-growing cystic glioma of the cervical cord. The fatty marrow change in vertebral bodies C4 through T1 is a result of radiation-induced ischemia. Note the posterior vertebral scalloping of the C7 and T1 due to long-standing spinal cord expansion caused by the tumor.
Sagittal T1-weighted MRI of the cervical spine in a 37-year-old woman who underwent radiation therapy for a slow-growing cystic glioma of the cervical cord. The fatty marrow change in vertebral bodies C4 through T1 is a result of radiation-induced ischemia. Note the posterior vertebral scalloping of the C7 and T1 due to long-standing spinal cord expansion caused by the tumor.
MRI characteristics of bone infarction are variable focal abnormalities and are commonly demonstrated as patchy areas of low signal intensity on T1-weighted spin-echo images. Diffuse abnormal signal intensity may be present in osteonecrosis of the femoral head; these changes are reflected on both T1- and T2-weighted images.
The most characteristic appearance is the double-line sign, which consists of a hyperintense inner ring and a hypointense outer ring, on T2-weighted MRIs. This finding reflects the reactive interface between ischemic and nonischemic bone. The absence of a double-line sign does not exclude osteonecrosis. On T1-weighted MRIs, the interface appears as a low-signal-intensity line, which reflects a combination of granulation tissue and, to a lesser extent, sclerotic bone. Gadolinium-enhanced short–inversion recovery images demonstrate diminished enhancement in early infarctions of the femoral head.
In sickle cell disease, acute bone infarcts are caused by sequestration of red blood cells in the bone marrow. Thus, non-enhanced T1-weighted fat-saturated sequences appear to be diagnostic of acute bone infarcts. [11] Contrast enhancement aids in the diagnosis of acute osteomyelitis. [12]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
MRI is highly sensitive and specific for osteonecrosis of the femoral head. T1 images typically demonstrate a serpiginous band-like lesion with low signal intensity in the anterosuperior femoral head; a double-line sign is seen on T2 sequences. [4]
No consensus has been reached regarding the best MRI sequences or imaging planes to use, although sagittal images, particularly when combined with the application of surface coils and small fields of view, appear to be more helpful than other images. [6]
In a study by Tsukamoto et al of 63 knees that underwent MRI, spontaneous osteonecrosis of the knee, compared with osteoarthritis, had a significantly larger varus deformity at the proximal tibia and larger joint play in the coronal plane. [34]
Degree of confidence
MRI is considered more sensitive than standard scintigraphy. MRI is sensitive in the detection of spontaneous infarction around the knee.
MRI is useful in assessing the response to therapy, particularly the response of the femoral head to core decompression in which ischemic areas may shrink and edema may resolve. However, more often, the MRI characteristics of the infarcted area change little over time.
Diffusely distributed abnormal MRI findings of osteonecrosis in the femoral head may mimic transient osteoporosis of the hip, infection, or neoplasia. For instance, diffuse abnormal signal intensity on both T1- and T2-weighted images may mimic findings in infective and neoplastic processes.
Ultrasonography
A combination of scintigraphy and ultrasonography has been used in the differentiation of osteomyelitis from bone infarction in patients with sickle cell disease. [9, 10] Scintigraphic studies are useful in locating all areas of suggested osteomyelitis. Ultrasonography has a role in confirming the presence of a subperiosteal fluid collection and in guiding aspiration, which can be performed to distinguish a hematoma from an abscess.
In one series of 23 patients in whom osteomyelitis was associated with sickle disease, 21 patients had a subperiosteal fluid collection that was more than 10 mm at its thickest point. By contrast, patients with sickle cell crises had fluid collections less than 10 mm. Aspiration of fluid under ultrasonographic guidance is useful in differentiating osteomyelitis from infarction. In patients with osteomyelitis, the identification of the organism guides antibiotic administration. Needle decompression can help relieve pain in patients with osteomyelitis and sickle cell crises.
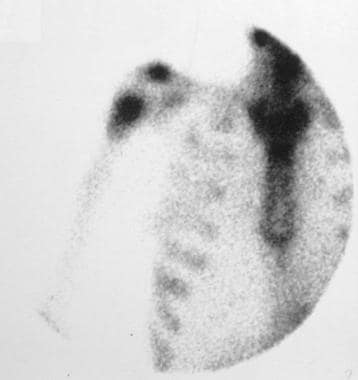
Nuclear Imaging
After acute osteonecrosis occurs, technetium-99m diphosphonate uptake can be absent after 72 hours. Subsequently, with revascularization and associated osteoblastic repair, intense activity is seen.
The clinical assessment of posttraumatic AVN of the femoral head is difficult, though the preoperative identification of AVN is important. The displacement at the fracture site and the degree of femoral head ischemia are significantly correlated, but plain-film radiology is not reliable in the prediction of ischemia.
The appearances on isotopic scans depend on the time elapsed since injury (see the images below). Initially, the area of infarction has a photon-deficient or doughnut-like appearance, with increased activity surrounding the photopenic area. Subsequently, the photopenic area shrinks; as healing progresses, activity becomes uniform and intense. These changes are reliable, with a predictive value of 92.5%. Further improvement may be achieved by using single-photon emission tomography (SPECT). The major role of SPECT is in demonstrating a persistent photopenic defect resulting from incomplete vascularization.
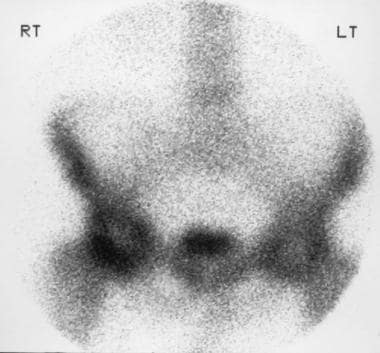 Radionuclide bone scan of the pelvis in a 68-year-old man with hip pain demonstrates a bilateral central area of diminished uptake surrounded by a zone of increased uptake in the femoral head consistent with avascular necrosis.
Radionuclide bone scan of the pelvis in a 68-year-old man with hip pain demonstrates a bilateral central area of diminished uptake surrounded by a zone of increased uptake in the femoral head consistent with avascular necrosis.
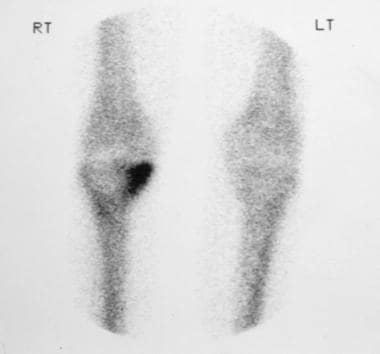 Radionuclide bone scan of the right knee joint in a 52-year-old woman with abrupt onset of right knee pain shows increased accumulation of the isotope in the medial aspect of the tibia plateau consistent with spontaneous osteonecrosis.
Radionuclide bone scan of the right knee joint in a 52-year-old woman with abrupt onset of right knee pain shows increased accumulation of the isotope in the medial aspect of the tibia plateau consistent with spontaneous osteonecrosis.
Because myeloid tissue death precedes death of osteophytes, it has been proposed that radiocolloid imaging is superior to imaging with 99mTc diphosphonate in determining the viability of the femoral head, although some success has been achieved by using 99mTc sulfur colloid or 99mTc antimony colloid. However, false-positive scanning results have been reported in inactive marrow, particularly in elderly patients.
The scaphoid bone is the most frequently fractured carpal bone. Approximately one quarter to one half of fractures are missed on radiographs. Isotopic bone scans are 100% sensitive in the diagnosis of scaphoid fractures. AVN of the proximal fragment of the scaphoid bone is often a concern. On scintigraphs, a photopenic area may be demonstrated in the proximal fragment.
In patients with sickle cell disease, bone infarcts are typically multiple during the course of a sickle cell crisis. Areas of infarction are demonstrated as photopenic foci within 72 hours after the crisis. Splenic infarcts are also known to take up 99mTc diphosphonate and are a useful hint to the presence of sickling (see the image below). [35]
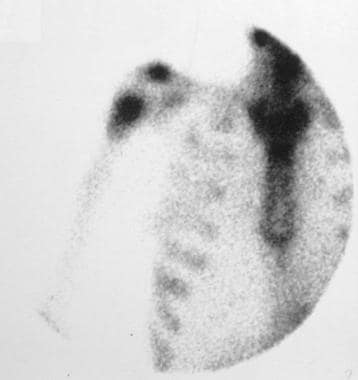 Radioisotopic bone scan of the right humerus in a patient with pancreatitis shows a hot lesion, the result of revascularization, which is a part of the reparative process.
Radioisotopic bone scan of the right humerus in a patient with pancreatitis shows a hot lesion, the result of revascularization, which is a part of the reparative process.
Revascularization results from collateral vessels that are predominantly derived from the periosteal blood supply; revascularization can be observed on isotopic bone scans as peripheral stripes of enhanced activity that extend with the healing process. However, a true bone infarct seldom occurs in an epiphysis because the epiphysis usually has an adequate collateral blood supply.
Ischemia may stimulate only osteoblastic activity, which results in increased isotope uptake without a photopenic stage. This feature poses problems in differentiating a bone infarct from osteomyelitis in the setting of sickle cell disease. Scanning with gallium-67 citrate may be required because its uptake is decreased or absent in acute infarction and is normal or increased in healing infarcts. Ga-67 citrate is useful in differentiating septic infarction from fulminant photon-deficient osteomyelitis.
Similar changes occur in patients with Gaucher disease. In these patients, vascular compromise is caused by the accumulation of lipid-filled enlarged histiocytes within the medulla. The radioactivity is reduced, with a subsequent increase in isotopic uptake in the healing phase. Ga-67 citrate is invaluable in differentiating photo-deficient osteomyelitis from a bone infarction.
Radiation necrosis is dose dependent and most probably is related to alteration in the microvasculature rather than direct bone damage. In most instances, affected bone is incidentally irradiated during the course of therapy in an adjacent organ. The isotopic uptake in radiation necrosis is variable. Changes indistinguishable from radiation necrosis may occur as a result of frostbite.
Bone scintigraphy reveals a focal increase in activity in spontaneous osteonecrosis around the knee, which can be identified long before radiographic changes become apparent. Similar findings apply to AVN of the talus that occurs after trauma.
Steroid-induced AVN causes a variety of changes, a fact that probably reflects its multifactorial etiology. A large photopenic area may be seen, similar to changes associated with major vascular compromise; however, more often, intense activity is noted at the site of infarction. These changes are less common than findings of patchy areas of increased accumulation of the radionuclide, sometimes with a streaky pattern of increase in the uptake. On occasion, multiple small areas of uptake are seen in the infarcted area.
Caisson disease is characterized by large areas of increased activity, which mostly is juxta-articular. The role of radionuclide scans is proposed to lie in predicting the development of necrosis in the lesions and thereby predicting the risk of the later development of osteoarthrosis.
Degree of confidence
Radionuclide uptake can be absent after 72 hours in viable osteocytes, whereas MRI findings are not altered for as long as 6 weeks. MRI findings in a series of 8 patients were negative, whereas radionuclide studies showed decreased isotope uptake in early osteonecrosis in patients at risk for AVN. This observation is not surprising because MRI depicts osteonecrosis by demonstrating bone marrow edema.
However, studies have revealed that fat cells are resistant to ischemia, dying 5 days after the initial insult. Though MRI findings may be negative, findings from isotopic scans may become positive during this period.
Many investigators have found that the series of changes in femoral neck fractures are reliable in ascertaining the viability of the femoral head. The accuracy in the prediction of such viability is 92.5%.
Bone scanning appears to be more sensitive than MRI in the detection of AVN of the scaphoid bone, but it is less specific. In scaphoid fractures, demonstration of a focal area of hyperemia and increased uptake provide reassurance in indicating revascularization.
Scintigraphic changes in steroid-induced osteonecrosis are detectable months before any abnormal findings are discernible on radiographs. Radionuclide scans have a sensitivity of 89% in detecting ischemic necrosis; by contrast, radiologic methods have a sensitivity of 41%.
Imaging characteristics of a bone infarct per se are nonspecific, and increased activity can be caused by a variety of conditions such as fractures, infections, inflammations, and metabolic and neoplastic processes. Photon-deficient bone lesions may occur with early osteomyelitis, plasmacytoma, histiocytosis X, bone metastases, and sickle cell crises.
Angiography
Intramedullary phlebography has been used in the diagnosis of bone infarction in the femoral head. The technique involves traversing the trochanteric bone with a bone needle, such as the Jamshidi needle, and injecting radiographic iodinated contrast material through it. Normal venographic findings thus obtained are usually characterized by painlessness on injection and by the demonstration of draining veins without diaphyseal reflux or stasis. When necrosis of the femoral head is present, the injection is painful and is usually followed by reflux into the diaphysis and stasis of the contrast agent for as long as 15 minutes.
The exact sensitivity of intramedullary phlebography is not known. The technique is invasive, and because there are so many other techniques now available, phlebography is seldom indicated. The technique must be performed by a radiologist with expertise in this area.
-
Diagram shows how the vascular supply to the femoral head is maintained by the retinacular blood vessels in the pertrochanteric fracture of the femur.
-
Diagram shows how a subcapital fracture of the femoral neck cuts off of the blood supply to the femoral head, resulting in osteonecrosis.
-
Diagram shows the blood supply to the humeral head.
-
Diagram shows the blood supply to the talus via the artery of the tarsal canal.
-
Diagram shows the blood supply to the scaphoid bone.
-
Plain radiograph in a middle-aged man with shoulder discomfort demonstrates an irregularly calcified bone infarct in the diametaphysis of the right humerus.
-
Coronal T1-weighted MRI in a 12-year-old boy with early Legg-Calvé-Perthes disease demonstrates slight irregularity of the right femoral capital epiphysis with abnormal signal intensity. The left hip appears normal.
-
Coronal T1 weighted MR image of a 20-year-old woman with bilateral late-stage Legg-Calvé-Perthes disease demonstrates flattening of the right femoral head and acetabulum.
-
Coronal T1-weighted MRI of the left hip in the patient in the previous image, shows a short, broad femoral neck. This bone remodeling is associated with Legg-Calvé-Perthes disease.
-
Plain radiograph in a 68-year-old man with hip pain demonstrates patchy sclerosis of both femoral heads that is consistent with avascular necrosis.
-
Radionuclide bone scan of the pelvis in a 68-year-old man with hip pain demonstrates a bilateral central area of diminished uptake surrounded by a zone of increased uptake in the femoral head consistent with avascular necrosis.
-
Plain radiograph of the pelvis in a man demonstrates collapse of the left femoral head due to osteonecrosis.
-
Coronal T2-weighted MRI in a 35-year-old man with bilateral avascular necrosis of the hip demonstrates a central region of increased signal intensity and a peripheral region of decreased signal intensity. The double-line sign is characteristic of osteonecrosis.
-
Coronal T1-weighted MRI in a 42-year-old man with bilateral avascular necrosis shows an area of osteonecrosis in both femoral heads in which a serpentine area of low signal intensity surrounds a central area of intermediate signal intensity similar to that of fat.
-
Coronal T2-weighted MRI of the same patient as in the previous image.
-
Plain radiograph of the right knee joint in a 52-year-old woman with abrupt onset of right knee pain demonstrates subtle loss of bone density in the proximal aspect of the tibia (arrow).
-
Radionuclide bone scan of the right knee joint in a 52-year-old woman with abrupt onset of right knee pain shows increased accumulation of the isotope in the medial aspect of the tibia plateau consistent with spontaneous osteonecrosis.
-
Posttraumatic osteonecrosis of the right femoral head in a woman. Note the arclike subchondral radiolucency secondary to subchondral fracture and collapse.
-
Plain radiograph of the left wrist in a man with posttraumatic osteonecrosis of the scaphoid bone shows sclerosis of the proximal portion of the scaphoid bone.
-
Plain radiograph of the right wrist of a man demonstrates sclerosis, irregularity, and collapse of the lunate bone consistent with osteonecrosis Kienböck disease.
-
Osteonecrosis of the third metatarsal head (ie, Freiberg disease) in a 60-year-old woman is shown as flattening of the third metatarsal head, widening of the third metatarsal, and expansion of the corresponding proximal phalangeal base.
-
Plain radiograph of the left ankle in a patient with ankle injury demonstrates subchondral radiolucent band (arrow) in proximal talus, the Hawkins impingement sign, which represents bone resorption and an intact blood supply.
-
Plain radiograph of the left ankle in an adult patient with osteonecrosis of the talus. Note the increased radiopacity of the body of the talus.
-
Patchy irregular sclerotic lesion characteristic of bone infarct is seen in the proximal metadiaphysis of right humerus in a patient with pancreatitis.
-
Radioisotopic bone scan of the right humerus in a patient with pancreatitis shows a hot lesion, the result of revascularization, which is a part of the reparative process.
-
Plain abdominal radiograph in a patient with sickle cell disease shows generalized coarsening of the bone trabeculae with characteristic H-shaped vertebrae due to a growth disturbance. Note the calcified and contracted spleen.
-
Lateral view of the knee in a deep-sea diver shows dysbaric osteonecrosis in the diaphysis of the femur and tibia. Note the irregular calcific deposits with a shell-like pattern, which is typical of a bone infarct.
-
Plain abdominal radiograph in a 19-year-old man with hemophilia. Osteonecrosis of the right humeral head is associated with calcified hematoma in the left groin.
-
Sagittal T1-weighted MRI of the cervical spine in a 37-year-old woman who underwent radiation therapy for a slow-growing cystic glioma of the cervical cord. The fatty marrow change in vertebral bodies C4 through T1 is a result of radiation-induced ischemia. Note the posterior vertebral scalloping of the C7 and T1 due to long-standing spinal cord expansion caused by the tumor.