Practice Essentials
The extensor mechanism of the knee consists of the quadriceps muscle group, quadriceps tendon, patella, patellar retinaculum, patellar ligament, and adjacent soft tissues. Injuries to the extensor mechanism are common and consist of chronic degenerative injuries, overuse injuries, and acute trauma. [1, 2, 3, 4]
Normal anatomy of the knee extensor compartment
An understanding of normal anatomy and biomechanics of the knee extensor mechanism is necessary to comprehend the imaging of extensor mechanism injuries.
The extensor mechanism of the knee begins above the hip with the origin of the rectus femoris muscle on the anterior inferior iliac spine. The remainder of the quadriceps muscle group, vastus lateralis, vastus intermedius, and vastus medialis originate on the femoral shaft. The quadriceps tendon represents the confluence of the 4 muscle tendon units and inserts on the superior pole of the patella. The quadriceps tendon has 3 laminae, including (1) the most superficial lamina, which is formed by the rectus femoris; (2) the intermediate lamina, which is formed by the vastus lateralis and vastus medialis; and (3) the deep lamina, which is formed by the vastus intermedius.
Laterally, the iliotibial band supports the extensor mechanism and is an important lateral stabilizer of the patellofemoral joint. It originates above the hip joint as a wide fascial band, originating from the gluteal muscles, tensor fascia lata, and vastus lateralis. Distally, the iliotibial band consists of two tracts. The iliotibial tract inserts on Gerdy tubercle of the lateral tibial plateau. [5] Fibers connecting the iliotibial band to the patella are referred to as the iliopatellar band.
The patellar retinaculum is an important soft tissue stabilizer of the patellofemoral joint. It is composed of a medial and lateral component. The thicker lateral retinaculum comprises a distinct, thick deep layer and a thin superficial layer. The deep layer is a confluence of several fibrous structures consisting of the lateral patellofemoral ligament and iliopatellar band. Deep to the medial patellar retinaculum, there are 3 focal capsular thickenings. These occasionally are referred to as the medial patellofemoral, patellomeniscal, and patellotibial ligaments.
The patella, the largest sesamoid bone in the body, possesses the thickest articular cartilage. The articular surface, which can have a variable contour, articulates with the trochlear groove of the femur. Most patellae possess a median ridge that divides the proximal patella into a medial and lateral facet; the medial facet usually is the smaller of the two.
The patellar tendon, occasionally termed the patellar ligament, originates at the inferior pole of the patella and inserts onto the tibial tuberosity. The patellar tendon is invested in a paratenon of loose fibrillar tissue.
Additional soft tissue structures of the knee extensor compartment consist of the infrapatellar fat pad and pretibial and prepatellar bursae. Injuries to these structures are associated with extensor mechanism injuries and can result in anterior knee compartment pain.
Normal biomechanics of the knee extensor compartment
The quadriceps muscle group functions as a knee extensor when the leg is elevated. When the foot is on the ground, contraction of the quadriceps stabilizes the knee, functioning as a decelerator. The patella provides a significant mechanical advantage to the knee extensor mechanism, allowing the knee to extend with a smaller contractile force of the quadriceps. In addition, the patella redirects the force exerted by the quadriceps, resulting in a large compressive stress on the patellofemoral joint. The magnitude of this stress usually is at a maximum with the knee flexed 90° and the foot planted, such as that occurring when one stands from a sitting position.
Only a portion of the patellar cartilage articulates with the femoral trochlea at any one time. With the knee extended 0°, the patella rides laterally within the trochlear groove and is not in direct contact with the trochlear cartilage. With knee flexion, the patella moves medially, and the degree of surface contact of the patellofemoral joint increases. Bone and cartilage contours of the patella and trochlear groove determine stability of the patellofemoral joint. Patellar subluxation (lateral displacement of the patella from the trochlear groove) is associated with a flat articular surface of the patella and a shallow trochlear groove.
Additional soft tissue structures provide both dynamic and static stabilization of the patellofemoral joint. The vastus medialis obliquus (VMO) is an important dynamic medial stabilizer of the patellofemoral joint. The VMO originates in the adductor tubercle of the distal medial femur and inserts on the medial retinaculum and superomedial patella. The iliotibial band provides dynamic lateral stabilization of the patella through the iliopatellar band. Additional dynamic stabilization is provided by insertion of fibers from the vastus medialis and lateralis onto the patellar retinacula. Static stabilizers consist of the medial and lateral retinaculum and the joint capsule.
Pathophysiology of injury
Most chronic degenerative injuries of the extensor mechanism are related to patellar malalignment. Abnormal tracking of the patella within the trochlear groove can produce focal areas of increased stress on the patellofemoral joint. The shallow trochlear groove seen with trochlear dysplasia allows the patella to sublux laterally with knee flexion. Abnormal lateral patellar tilt can be seen with a tight lateral retinaculum and is associated with excessive lateral pressure syndrome (ELPS) and patellar tendon-lateral femoral condyle friction syndrome. Over time, the abnormal stresses applied to the patellofemoral joint can result in focal cartilage degeneration, patellofemoral osteoarthritis, and damage to the soft tissue stabilizers of the patellofemoral joint.
The role of a degenerative extensor mechanism in knee osteoarthritis (KOA) is not fully understood. While multiple structures can help distribute the load during knee flexion (e.g., proximal gastrocnemius tendons), the extensor mechanism is the sole mechanism for knee extension. Therefore, more direct loading to the extensor may contribute to the development of KOA. [6]
Overuse injuries typically are seen in high performance athletes, most commonly in sports requiring long distance running or jumping. Cumulative microtrauma produced by repetitive knee flexion and extension results in focal inflammation.
Acute traumatic injuries occur secondary to direct blunt trauma or excessive tension applied to the extensor mechanism through quadriceps contraction. Patellar fractures are the most common traumatic injury of the knee extensor mechanism.
In a study by Horga et al of 230 asympomatic knees, 3.0 Tesla high-resolution MRI showed abnormalities in 97% of knees. Thirty percent had meniscal tears, with 23% horizontal, 3% complex, 2% vertical, 2% radial, and 1% bucket handle. Cartilage abnormalities were present in 57%, and bone marrow abnormalities in 48%. [7]
Technical Considerations for MRI Evaluation of the Knee Extensor Mechanism
Because of the excellent soft tissue contrast and the ability to obtain images directly in the sagittal plane, MRI is the preferred technique for evaluating soft tissue injuries to the knee extensor mechanism. [8, 9, 10, 11, 12, 13]
To maximize image signal to noise, acquire images using a dedicated extremity coil. In specific cases of patellar pathology, limited high-resolution images of the patellofemoral joint can be obtained using a small anterior surface coil. MRI protocol for evaluating the extensor mechanism consists of the following:
-
Sagittal spin-echo T1-weighted images
-
Sagittal fast spin-echo (FSE) T2-weighted images with chemical shift fat suppression or short tau inversion recovery (STIR) images
-
Axial FSE proton density-weighted images with fat suppression
On sagittal images, the field of view should extend from the musculotendinous junction of the rectus femoris to just below the tibial tuberosity. On axial images, the direction of phase encoding should be left to right to prevent pulsation artifact from the popliteal artery.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Injuries of the Patellofemoral Joint
Abnormalities of alignment
Abnormalities of alignment of the patellofemoral joint can result in a group of symptom complexes variously termed excessive lateral pressure syndrome, lateral hypercompression syndrome, and patellofemoral pain syndrome, according to Thomee. [14] The syndromes are characterized by joint pain accentuated by flexion.
During routine imaging, patellar subluxation may be seen, which reflects the underlying forces. In addition, abnormalities of the trochlear sulcus or patellar dysplasia may be seen. Specialized MRI techniques for dynamic evaluation of patellofemoral tracking under simulated load-bearing conditions are used in research studies evaluating subjects with patellofemoral pain [3] but are not routinely used in clinical practice. These techniques have been reviewed by Spritzer [15] and by Shellock and Powers [16] in a text on kinematic MRI.
An increased tibial tuberosity-trochlear groove (TTTG) distance is used for deciding a treatment plan in patellofemoral instability. The center of the patellar tendon and the chondral trochlear groove can be directly visualized on MRI and measured, providing the patellar tendon-trochlear groove (PTTG) distance. [17]
Patellar malalignment and dysplasia
Patellar malalignment and patellar dysplasia increase stress on patellar cartilage, resulting in development of patellofemoral osteoarthritis. In addition, patellofemoral cartilage degeneration may be related to underlying depositional disease, most frequently, calcium pyrophosphate deposition disease (CPPD), as described by Brandt. [18, 19, 20, 21]
MRI can visualize sites of cartilage damage directly. Early cartilage lesions are identified by areas of increased signal on T2-weighted images and by associated surface irregularity (see the image below), according to Disler. [22]
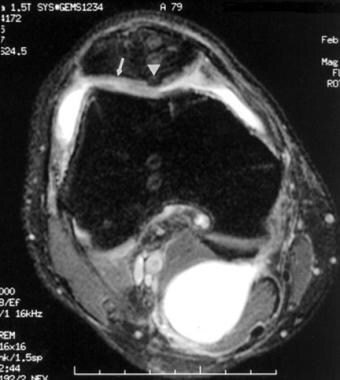 Extensor mechanism injuries of the knee. An axial fast spin-echo proton density-weighted image with fat suppression of a 50-year-old man demonstrates mild thinning of the patellar cartilage associated with foci of abnormal increased signal intensity within the patellar cartilage, consistent with areas of cartilage degeneration in mild patellofemoral osteoarthritis (arrow). Beware of pulsation artifact from the popliteal artery (simulating a central osteophyte) projecting off the posterior articular surface of the patella (arrowhead). Note the small joint effusion and increased signal intensity posteriorly resulting from a Baker cyst.
Extensor mechanism injuries of the knee. An axial fast spin-echo proton density-weighted image with fat suppression of a 50-year-old man demonstrates mild thinning of the patellar cartilage associated with foci of abnormal increased signal intensity within the patellar cartilage, consistent with areas of cartilage degeneration in mild patellofemoral osteoarthritis (arrow). Beware of pulsation artifact from the popliteal artery (simulating a central osteophyte) projecting off the posterior articular surface of the patella (arrowhead). Note the small joint effusion and increased signal intensity posteriorly resulting from a Baker cyst.
Whether isolated focal cartilage hyperintensity without associated surface irregularity represents preclinical cartilage damage not visualized on arthroscopy is under debate. Advanced stages of cartilage damage are associated with partial- or full-thickness loss of cartilage, osteophyte formation, and increased T2-weighted signal in the subchondral bone with or without subchondral cyst formation (see the image below).
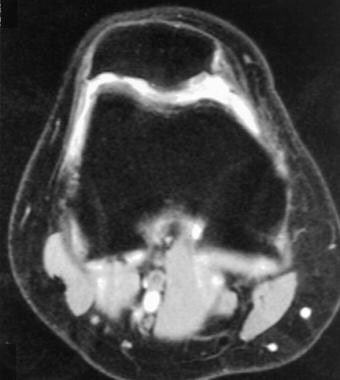 Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in a 39-year-old woman demonstrates irregularity, fissuring, and marked thinning of patellar cartilage associated with osteophyte formation. Findings are consistent with advanced osteoarthritis of the patellofemoral joint. Note the abnormal flat contour of the patellar articular surface. Abnormal joint biomechanics resulting from patellar dysplasia are associated with an increased incidence of patellofemoral osteoarthritis.
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in a 39-year-old woman demonstrates irregularity, fissuring, and marked thinning of patellar cartilage associated with osteophyte formation. Findings are consistent with advanced osteoarthritis of the patellofemoral joint. Note the abnormal flat contour of the patellar articular surface. Abnormal joint biomechanics resulting from patellar dysplasia are associated with an increased incidence of patellofemoral osteoarthritis.
A study by Zanetti and coworkers indicates this subchondral signal abnormality corresponds to degenerative edema, necrosis, and cyst formation in the subchondral bone marrow. [23]
Trochlear dysplasia is frequently associated with patellar malalignment. Yildiz and Ekin found that an increased medial patellofemoral ligament (MPFLL)/lateral patellar retinaculum (LPR) ratio helps detect patellar malalignment on knee MRI. [21]
Patellar dislocation
Patellar dislocation is often associated with dysplasia of the patella and trochlear groove. Hypoplasia of the femoral sulcus and lateral femoral condyle result in a shallow trochlear groove, which decreases stability of the patellofemoral joint. Similarly, findings of patellar dysplasia with a poorly formed median ridge and medial facet also are associated with abnormal patellar tracking and lateral dislocation, as reported by Resnick. [24, 25, 26]
An actual dislocation of the patella is rarely observed with MRI, although unusual cases of chronic patellar dislocation are documented (see the image below).
 Extensor mechanism injuries of the knee. An axial fast spin-echo proton density-weighted image with fat suppression of a 30-year-old man demonstrates a chronic congenital patellar dislocation. The small dysplastic patella is dislocated laterally (arrow).
Extensor mechanism injuries of the knee. An axial fast spin-echo proton density-weighted image with fat suppression of a 30-year-old man demonstrates a chronic congenital patellar dislocation. The small dysplastic patella is dislocated laterally (arrow).
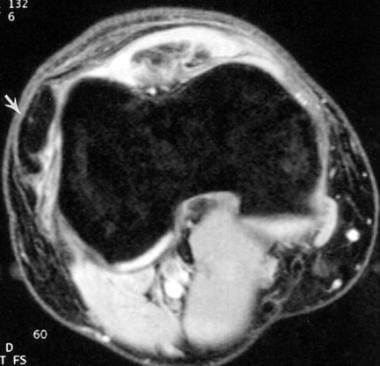
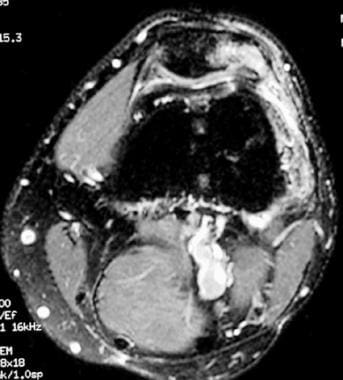
However, the sequela of patellar dislocation results in pathognomonic MRI findings, which include sprain or tear of the medial retinaculum, contusions of the anterior lateral femoral condyle and medial patellar facet, strain or tear of the VMO, and concomitant joint effusion (see the image below).
 Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in an 18-year-old man with prior knee trauma demonstrates many findings of previous patellar dislocation. A large joint effusion with focal marrow edema in the medial patellar facet and lateral femoral condyle is present. Edema and thickening of the medial retinaculum are compatible with partial tear.
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in an 18-year-old man with prior knee trauma demonstrates many findings of previous patellar dislocation. A large joint effusion with focal marrow edema in the medial patellar facet and lateral femoral condyle is present. Edema and thickening of the medial retinaculum are compatible with partial tear.
Osteochondral injury
Acute or chronic osteochondral injuries subsequent to trauma frequently are the causes of anterior knee pain, as reported by Obedian. [27] The imaging appearance and surgical management of these lesions has been reviewed by Gallo and Mosher. [28]
MRI FSE T2-weighted images with fat suppression or STIR images are sensitive to marrow edema and hemorrhage associated with radiographically occult bone marrow contusions (see the first image below) or nondisplaced patellar fractures. If patellar contusion is suspected, scrutinize the overlying patellar cartilage for focal cartilage tear or defects (see the second image below). [29]
 Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in an 18-year-old man following a fall on the knee. Diffuse hyperintensity of patellar marrow signal is compatible with acute bone marrow contusion. This abnormal signal corresponds to hemorrhage and edema with areas of fractured trabecula. Marrow contusion of the medial femoral condyle and moderate-sized joint effusion are seen.
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in an 18-year-old man following a fall on the knee. Diffuse hyperintensity of patellar marrow signal is compatible with acute bone marrow contusion. This abnormal signal corresponds to hemorrhage and edema with areas of fractured trabecula. Marrow contusion of the medial femoral condyle and moderate-sized joint effusion are seen.
 Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in a 28-year-old man following a fall resulting in blunt anterior knee trauma demonstrates fissuring of the medial patellar cartilage with underlying subchondral marrow edema. Abnormal fluid signal intensity extends in a linear fashion from the articular surface to involve the deep cartilage layer.
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in a 28-year-old man following a fall resulting in blunt anterior knee trauma demonstrates fissuring of the medial patellar cartilage with underlying subchondral marrow edema. Abnormal fluid signal intensity extends in a linear fashion from the articular surface to involve the deep cartilage layer.
Osteochondritis dissecans of the patella
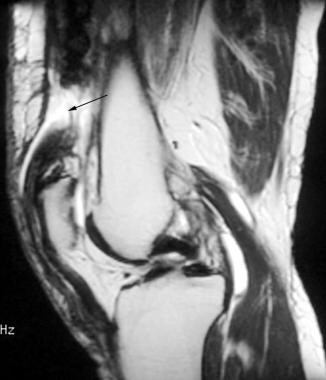
Osteochondritis dissecans (OCD) is characterized by partial or complete separation of an osteochondral fragment from the native bone in the absence of acute trauma. Compared to OCD of the femur, osteochondritis dissecans patella is a rare imaging finding (see the image below). [30, 31, 32]
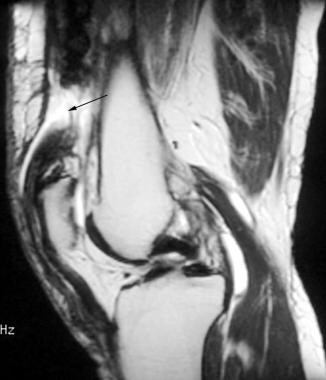
 Extensor mechanism injuries of the knee. This 42-year-old woman was referred for evaluation of chronic anterior knee pain for 2 years following a motor vehicle accident. Sagittal T1-weighted image demonstrates areas of focal decreased signal involving the posterior aspect of the patella and the medial femoral condyle, consistent with areas of chronic osteochondral injury (osteochondritis dissecans). With the knee flexed, these areas are aligned (kissing contusions). This pattern is consistent with focal areas of traumatic osteochondral injury from impaction during the motor vehicle accident.
Extensor mechanism injuries of the knee. This 42-year-old woman was referred for evaluation of chronic anterior knee pain for 2 years following a motor vehicle accident. Sagittal T1-weighted image demonstrates areas of focal decreased signal involving the posterior aspect of the patella and the medial femoral condyle, consistent with areas of chronic osteochondral injury (osteochondritis dissecans). With the knee flexed, these areas are aligned (kissing contusions). This pattern is consistent with focal areas of traumatic osteochondral injury from impaction during the motor vehicle accident.
Unlike the dorsal defect of the patella, which, based on data reported by Safran, [33] typically is located in the superolateral patella, osteochondritis dissecans of the patella occurs most frequently in the distal half of the medial facet, as reported by Schwarz. [34] Typically, the subchondral fragment remains in situ.
Injuries of the Musculotendon Extensor Mechanism
Patellar tendinopathy
Patellar injuries can result from chronic overuse injuries or as a result of acute trauma. Patellar tendonosis, or jumper's knee, results from chronic overload on the patellar tendon because of strain from the quadriceps muscle group, as described by Khan. [35] Chronic overload results in microtears and focal degeneration, which is characterized histologically by pseudocyst formation, increased fibrocartilage, and myxomatous and hyaline metaplasia. [36, 37] Because few inflammatory cells are identified in tendons of patients with chronic patellar tendinopathy, the term patellar tendonitis should be reserved for acute tendinopathy. [38]
Patellar tendonosis frequently is seen in participants in sports associated with jumping and is associated with malalignment syndromes, as described by Allen and coworkers. [39]
MRI findings consist of focal thickening of the proximal patellar tendon, with increased signal on T1-weighted and T2-weighted images (see the image below).
 Extensor mechanism injuries of the knee. Sagittal T1-weighted images in a 29-year-old man with chronic infrapatellar knee pain demonstrate a focal area of abnormal increased signal intensity in the proximal portion of the patellar tendon at the bone-tendon insertion. This involves the posterior portion of the tendon more extensively and is associated with focal enlargement of the tendon. Sparing of the anterior component of the tendon is typical of chronic patellar tendonitis (jumper's knee) and helps distinguish this condition from an acute process. Note the lack of subcutaneous edema in this patient.
Extensor mechanism injuries of the knee. Sagittal T1-weighted images in a 29-year-old man with chronic infrapatellar knee pain demonstrate a focal area of abnormal increased signal intensity in the proximal portion of the patellar tendon at the bone-tendon insertion. This involves the posterior portion of the tendon more extensively and is associated with focal enlargement of the tendon. Sparing of the anterior component of the tendon is typical of chronic patellar tendonitis (jumper's knee) and helps distinguish this condition from an acute process. Note the lack of subcutaneous edema in this patient.
It is important to recognize that intermediate signal on T1-weighted images is observed in the posterior margin of the proximal patellar tendon and near the tibial tuberosity in normal tendons, as described by Yu. [40] Edema in the paratenon, infrapatellar fat pad, and subcutaneous adipose tissue is associated with acute patellar tendonitis, which is defined as symptoms of less than 2-week duration and patellar tendon tears. Acute patellar tendonitis is associated with increased intrasubstance signal on T1-weighted and T2-weighted images without tendon thickening.
Patellar tendon tears
Patellar tendon tears may be partial or complete; they most frequently occur in the proximal inferior patellar tendon. A patellar sleeve fracture represents a cartilaginous avulsion from the lower pole of the patella and is often associated with patellar tendon tears (see the image below). With complete inferior patellar tendon tears, the patella retracts proximally as a result of the pull of the superior patellar tendon.
 Extensor mechanism injuries of the knee. Patellar avulsion fracture resulting from acute trauma as a result of a football injury. Sagittal FSE T2-weighted image with fat suppression demonstrates an avulsion fracture from the lower pole of the patella (arrow) and associated tear of the patellar tendon (arrow) (Image courtesy of Gary Gold, Stanford University).
Extensor mechanism injuries of the knee. Patellar avulsion fracture resulting from acute trauma as a result of a football injury. Sagittal FSE T2-weighted image with fat suppression demonstrates an avulsion fracture from the lower pole of the patella (arrow) and associated tear of the patellar tendon (arrow) (Image courtesy of Gary Gold, Stanford University).
Generally, discontinuity of the tendon is demonstrated on fluid-sensitive sagittal T2-weighted and STIR images. MRI findings in partial patellar tendon tears can resemble acute patellar tendonitis. Correlation with a history of acute trauma is useful for specific diagnosis.
Quadriceps tendinopathy
Quadriceps tendinopathy occurs with much less frequency than patellar tendinopathy but demonstrates similar imaging findings. The distal tendon, at the insertion in the patella, is the most common site of involvement.
MRI findings consist of fusiform tendon thickening with loss of the normal lamellated architecture and indistinctness of the intervening fatty tissue planes (see the image below). Focal signal changes are observed less frequently than with patellar tendonitis.
 Extensor mechanism injuries of the knee. Sagittal fast spin-echo proton density-weighted images with fat suppression images in a 40-year-old man with anterior knee pain following trauma demonstrates diffuse thickening of the infrapatellar tendon as well as linear areas of abnormal intermediate signal intensity within the substance of the tendon. Findings are consistent with an acute partial tear of the patellar tendon. Chronic patellar tendonitis complicated by chronic tears associated with inflammation and necrosis can appear similar on MRI; however, in this patient, subcutaneous edema anterior to the tendon also is seen, suggesting a relatively acute injury.
Extensor mechanism injuries of the knee. Sagittal fast spin-echo proton density-weighted images with fat suppression images in a 40-year-old man with anterior knee pain following trauma demonstrates diffuse thickening of the infrapatellar tendon as well as linear areas of abnormal intermediate signal intensity within the substance of the tendon. Findings are consistent with an acute partial tear of the patellar tendon. Chronic patellar tendonitis complicated by chronic tears associated with inflammation and necrosis can appear similar on MRI; however, in this patient, subcutaneous edema anterior to the tendon also is seen, suggesting a relatively acute injury.
Quadriceps tendon tear
A tear of the quadriceps tendon is the second most common acute injury to the extensor mechanism. Tears of the quadriceps tendon usually occur in an older patient population than tears of the patellar tendon. Often, a predisposing risk factor exists, such as diabetes, gout, or rheumatoid arthritis. In the younger patient, acute tears can result as a function of forced muscle contraction or blunt trauma.
MRI is useful in differentiating complete from partial quadriceps tendon tears. With complete tears, discontinuity of the tendon with associated retraction of the proximal remnant usually is visualized best using T2-weighted images (see the image below).
 Extensor mechanism injuries of the knee. FSE T2-weighted image demonstrating complete tear of the quadriceps tendon in 67-year-old man. Retraction of the quadriceps tendon consistent with complete tear is observed (arrow) with mild undulating contour of the patellar tendon. (Image courtesy of Douglas Goodwin, Dartmouth-Hitchcock Medical Center).
Extensor mechanism injuries of the knee. FSE T2-weighted image demonstrating complete tear of the quadriceps tendon in 67-year-old man. Retraction of the quadriceps tendon consistent with complete tear is observed (arrow) with mild undulating contour of the patellar tendon. (Image courtesy of Douglas Goodwin, Dartmouth-Hitchcock Medical Center).
Often, an associated hematoma is seen with heterogeneous signal intensity on T1-weighted images. Although an undulating contour of the patellar tendon can be seen with complete quadriceps tendon tears, it also can result from hyperextension of the knee and is not a specific indirect sign. Partial tears most commonly involve the anterior rectus femoris tendon fibers at the patellar insertion. Discontinuity of any of the quadriceps lamina is consistent with a partial tear.
Myotendinous strain
Myotendinous strain is a common injury in athletes. The most commonly injured muscles are fusiform muscles that cross 2 joints. In these muscles, high tensile stress develops when the muscle is forced to lengthen during active contraction, a process termed eccentric contraction. Because the rectus femoris muscle is the only component of the quadriceps muscle group that crosses 2 joints, it is the most common site for myotendinous strain injuries in the knee extensor mechanism.
MRI findings of strain injuries consist of focal edema centered on the central tendon of the rectus femoris. The presence of a focal hematoma is indicative of a partial myotendinous tear (see the first image below). Complete myotendinous tears often are recognized clinically, and patients with these injuries undergo MRI less frequently. Other abnormalities of the regional muscles, such as traumatic muscle tears (see the second image below), myositis, and infarction, can produce regional knee pain.
 Extensor mechanism injuries of the knee. Sagittal T1-weighted image in a 68-year-old man demonstrates abnormal thickening of the quadriceps tendon associated with areas of linear abnormal increased signal intensity within the substance of the tendon (arrow). This is consistent with a partial tear of the quadriceps tendon in this patient with acute injury. The normal tendon typically has a laminated appearance. Fusiform thickening and loss of normal sharp margins of the quadriceps laminae are common manifestations of injury.
Extensor mechanism injuries of the knee. Sagittal T1-weighted image in a 68-year-old man demonstrates abnormal thickening of the quadriceps tendon associated with areas of linear abnormal increased signal intensity within the substance of the tendon (arrow). This is consistent with a partial tear of the quadriceps tendon in this patient with acute injury. The normal tendon typically has a laminated appearance. Fusiform thickening and loss of normal sharp margins of the quadriceps laminae are common manifestations of injury.
 Extensor mechanism injuries of the knee. FSE T2-weighted image demonstrating complete tear of the quadriceps tendon in 67-year-old man. Retraction of the quadriceps tendon consistent with complete tear is observed (arrow) with mild undulating contour of the patellar tendon. (Image courtesy of Douglas Goodwin, Dartmouth-Hitchcock Medical Center).
Extensor mechanism injuries of the knee. FSE T2-weighted image demonstrating complete tear of the quadriceps tendon in 67-year-old man. Retraction of the quadriceps tendon consistent with complete tear is observed (arrow) with mild undulating contour of the patellar tendon. (Image courtesy of Douglas Goodwin, Dartmouth-Hitchcock Medical Center).
Injuries of Peripatellar Soft Tissues
Prepatellar bursitis (housemaid's knee)
Prepatellar bursitis can result from a number of causes (ie, acute or chronic trauma, inflammatory or deposition diseases, infection). The prepatellar bursa is located anterior to the distal half of the patella. Acute bursitis may result from direct trauma or chronic friction, resulting in an acute inflammatory response. Chronic bursitis results from repeated insults (see the image below). Septic bursitis may be the sequela of direct inoculation or hematogenous dissemination.
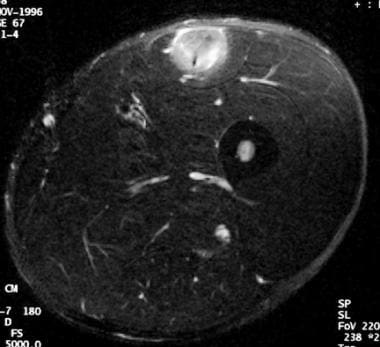 Extensor mechanism injuries of the knee. Axial fast spin-echo T2-weighted image with fat suppression in a 21-year-old soccer player demonstrates focal abnormal high signal intensity centered on the tendon of the rectus femoris, at the musculotendinous junction. The location and appearance is indicative of a partial tear of the musculotendinous junction. These tears usually are seen in young athletes and are associated with either forced muscle contraction or direct injury.
Extensor mechanism injuries of the knee. Axial fast spin-echo T2-weighted image with fat suppression in a 21-year-old soccer player demonstrates focal abnormal high signal intensity centered on the tendon of the rectus femoris, at the musculotendinous junction. The location and appearance is indicative of a partial tear of the musculotendinous junction. These tears usually are seen in young athletes and are associated with either forced muscle contraction or direct injury.
Pes anserinus bursitis
The pes anserinus bursa is located between the aponeurosis of the sartorius, gracilis, and semitendinosus tendons and the medial collateral ligament. It is approximately 2 cm below the anteromedial joint line and does not communicate with the knee joint. Inflammation of the pes anserinus bursa typically presents as anteromedial joint line pain and may mimic a meniscal tear. It most commonly is seen in long-distance runners in whom it can be associated with inflammatory changes of the adjacent pes anserine tendons.
Imaging findings of pes anserinus bursitis are increased signal intensity and fluid on T2-weighted images, best seen on axial and coronal imaging, and inflammatory stranding in this characteristic location.
Iliotibial band friction syndrome
The iliotibial band originates as a wide fascial band in the upper lateral pelvis and thigh and inserts on Gerdy tubercle of the lateral tibial plateau. Iliotibial band friction syndrome (see the image below) results in pain in the lateral side of the knee during activity and, most frequently, is seen in long-distance runners, cyclists, or others performing tasks resulting in repetitive knee flexion. Symptoms arise from excessive friction between the iliotibial band and the lateral femoral condyle. Imaging findings in this entity are abnormal increased signal on T2-weighted images centered between the iliotibial band and lateral femoral condyle.
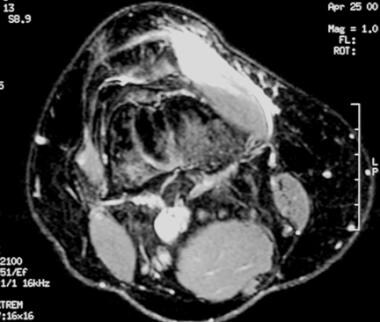 Extensor mechanism injuries of the knee. Axial fast spin-echo T2-weighted image with fat suppression in this 38-year-old woman presenting after direct trauma to the knee demonstrates abnormal increased signal intensity in the vastus medialis oblique muscle consistent with myositis and edema from a partial tear. The vastus medialis oblique muscle provides dynamic medial force on the patella and is an important stabilizer for patellar tracking.
Extensor mechanism injuries of the knee. Axial fast spin-echo T2-weighted image with fat suppression in this 38-year-old woman presenting after direct trauma to the knee demonstrates abnormal increased signal intensity in the vastus medialis oblique muscle consistent with myositis and edema from a partial tear. The vastus medialis oblique muscle provides dynamic medial force on the patella and is an important stabilizer for patellar tracking.
Synovial plica syndrome
Synovial plicae are folds in the synovium representing residual embryonic synovial septi that occasionally may be responsible for peripatellar pain, as reported by Dupont. [41] Four locations of plicae are described, including suprapatellar, infrapatellar, medial, and lateral. They may become inflamed from overuse or direct trauma. Chronic inflammation of the plica leads to fibrosis, resulting in inelasticity and thickening. The most frequent clinical symptom of plica syndrome is chronic aching discomfort aggravated by activity. Abnormal plicae are theorized to produce symptoms via several mechanisms. The inflammation of the plica may be painful, or pain may result from irritation or inflammation of the synovium (see the image below). Fibrotic plica also may abrade and damage the neighboring hyaline cartilage. The medial patellar plica is most often associated with symptoms. Imaging findings in this entity include thickening and irregularity of the plicae.
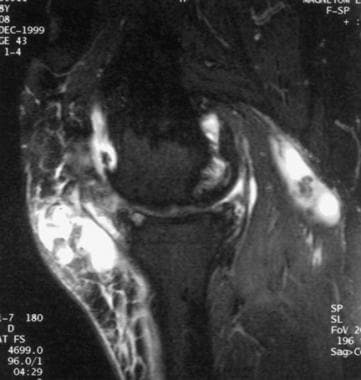 Extensor mechanism injuries of the knee. Sagittal fast spin-echo T2-weighted image with fat suppression in a 58-year-old woman demonstrates a complex fluid collection anterior to the knee in the region of the prepatellar bursa. The wall of the prepatellar bursa is thickened and irregular in appearance, consistent with chronic prepatellar bursitis. Note the underlying degenerative changes of the knee joint associated with osteophytic spurring. Irregularity of the Hoffa fat pad and a complex Baker cyst consistent with synovitis are seen. Synovial inflammatory processes can predispose patients to prepatellar bursitis.
Extensor mechanism injuries of the knee. Sagittal fast spin-echo T2-weighted image with fat suppression in a 58-year-old woman demonstrates a complex fluid collection anterior to the knee in the region of the prepatellar bursa. The wall of the prepatellar bursa is thickened and irregular in appearance, consistent with chronic prepatellar bursitis. Note the underlying degenerative changes of the knee joint associated with osteophytic spurring. Irregularity of the Hoffa fat pad and a complex Baker cyst consistent with synovitis are seen. Synovial inflammatory processes can predispose patients to prepatellar bursitis.
Fibrosis
Patellofemoral maltracking can compress the superior lateral region of the infrapatellar fat pad between the patellar tendon and the lateral femoral condyle, leading to focal inflammation. [42] Chronic impingement on the infrapatellar (Hoffa) fat pad may result in irritation and inflammation, culminating in fibrosis, which is termed Hoffa disease, as described by Jacobson (see the image below). [43]
Typical MRI features consist of irregularity and heterogeneous edema within the fat pad identified as high signal on STIR or T2-weighted images with or without fat suppression. Areas of fibrosis are identified by low signal intensity of the infrapatellar fat pad on T1-weighted and T2-weighted images. On rare occasions, calcification can be seen, which should be differentiated from superficial irregularity of the superior surface of the infrapatellar fat pad (a nonspecific sign of synovitis).
 Extensor mechanism injuries of the knee. In this 27-year-old female marathon runner with anterolateral pain superior to the joint line, coronal fast spin-echo T2-weighted image with fat suppression demonstrates edema between the iliotibial band and lateral femoral condyle (arrow). The location of edema is consistent with the clinical diagnosis of iliotibial band friction syndrome.
Extensor mechanism injuries of the knee. In this 27-year-old female marathon runner with anterolateral pain superior to the joint line, coronal fast spin-echo T2-weighted image with fat suppression demonstrates edema between the iliotibial band and lateral femoral condyle (arrow). The location of edema is consistent with the clinical diagnosis of iliotibial band friction syndrome.
Conditions Seen in Juveniles
Osgood-Schlatter disease is osteochondrosis of the tibial tuberosity, which is believed to result from repetitive microtrauma (see the images below). The condition is manifested by activity-related pain around the tibial tubercle. A high incidence of Osgood-Schlatter is seen in patients with patella alta, [44] presumably because of increased tension on the tibial tuberosity, as reported by Grelsamer. [2, 45, 46]
 Extensor mechanism injuries of the knee. Sagittal gadolinium-enhanced T1-weighted image with fat suppression in a 32-year-old man demonstrates thickened, irregular, abnormally enhancing synovium and a thick enhancing suprapatellar plica (arrow). A large joint effusion is present as well, which aids in evaluating the abnormal appearing synovium and plica by distending the joint space.
Extensor mechanism injuries of the knee. Sagittal gadolinium-enhanced T1-weighted image with fat suppression in a 32-year-old man demonstrates thickened, irregular, abnormally enhancing synovium and a thick enhancing suprapatellar plica (arrow). A large joint effusion is present as well, which aids in evaluating the abnormal appearing synovium and plica by distending the joint space.
 Extensor mechanism injuries of the knee. Osteochondrosis of the tibial tuberosity: A sagittal T1-weighted image demonstrates bony fragmentation and irregularity of the tibial tuberosity. These findings are compatible with chronic Osgood-Schlatter condition in the appropriate clinical setting.
Extensor mechanism injuries of the knee. Osteochondrosis of the tibial tuberosity: A sagittal T1-weighted image demonstrates bony fragmentation and irregularity of the tibial tuberosity. These findings are compatible with chronic Osgood-Schlatter condition in the appropriate clinical setting.
Sinding-Larsen-Johansson syndrome is osteochondrosis involving the distal patellar pole. [45, 47, 48]
Bipartite patella is a rare cause of anterior knee pain, as described by Iossifidis (see the first image below). [49] In symptomatic bipartite patellae, the pain may result from chronic stress injury, a mechanism similar to that in the above 2 conditions (see the second image below).
 Extensor mechanism injuries of the knee. Painful bipartite patella. This 33-year-old man has a 2-year history of pain over the superolateral aspect of the patella. Axial fast spin-echo proton density-weighted image with fat suppression demonstrates a large amount of edema in the synchondrosis, superolateral fragment, and adjacent soft tissues. Painful bipartite patella is a rare condition believed to be related to chronic stress fracture and fibrous nonunion.
Extensor mechanism injuries of the knee. Painful bipartite patella. This 33-year-old man has a 2-year history of pain over the superolateral aspect of the patella. Axial fast spin-echo proton density-weighted image with fat suppression demonstrates a large amount of edema in the synchondrosis, superolateral fragment, and adjacent soft tissues. Painful bipartite patella is a rare condition believed to be related to chronic stress fracture and fibrous nonunion.
 Extensor mechanism injuries of the knee. A 19-year-old female runner with a long-standing history of anterior knee pain. Sagittal T2-weighted gradient-echo image demonstrates an irregular area of abnormal signal intensity in the Hoffa fat pad, which represents focal scarring and fibrosis. This is consistent with Hoffa disease, which is believed to result from repetitive impingement of the infrapatellar fat pad. Short term, increased signal intensity in the fat pad is seen on T2-weighted images. Long term, as in this patient, the subsequent fibrosis results in decreased signal intensity. Focal hypointensity on gradient-echo image is indicative of prior hemorrhage with hemosiderin deposits in the area of fibrosis.
Extensor mechanism injuries of the knee. A 19-year-old female runner with a long-standing history of anterior knee pain. Sagittal T2-weighted gradient-echo image demonstrates an irregular area of abnormal signal intensity in the Hoffa fat pad, which represents focal scarring and fibrosis. This is consistent with Hoffa disease, which is believed to result from repetitive impingement of the infrapatellar fat pad. Short term, increased signal intensity in the fat pad is seen on T2-weighted images. Long term, as in this patient, the subsequent fibrosis results in decreased signal intensity. Focal hypointensity on gradient-echo image is indicative of prior hemorrhage with hemosiderin deposits in the area of fibrosis.
-
Extensor mechanism injuries of the knee. An axial fast spin-echo proton density-weighted image with fat suppression of a 50-year-old man demonstrates mild thinning of the patellar cartilage associated with foci of abnormal increased signal intensity within the patellar cartilage, consistent with areas of cartilage degeneration in mild patellofemoral osteoarthritis (arrow). Beware of pulsation artifact from the popliteal artery (simulating a central osteophyte) projecting off the posterior articular surface of the patella (arrowhead). Note the small joint effusion and increased signal intensity posteriorly resulting from a Baker cyst.
-
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in a 39-year-old woman demonstrates irregularity, fissuring, and marked thinning of patellar cartilage associated with osteophyte formation. Findings are consistent with advanced osteoarthritis of the patellofemoral joint. Note the abnormal flat contour of the patellar articular surface. Abnormal joint biomechanics resulting from patellar dysplasia are associated with an increased incidence of patellofemoral osteoarthritis.
-
Extensor mechanism injuries of the knee. An axial fast spin-echo proton density-weighted image with fat suppression of a 30-year-old man demonstrates a chronic congenital patellar dislocation. The small dysplastic patella is dislocated laterally (arrow).
-
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in an 18-year-old man with prior knee trauma demonstrates many findings of previous patellar dislocation. A large joint effusion with focal marrow edema in the medial patellar facet and lateral femoral condyle is present. Edema and thickening of the medial retinaculum are compatible with partial tear.
-
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in an 18-year-old man following a fall on the knee. Diffuse hyperintensity of patellar marrow signal is compatible with acute bone marrow contusion. This abnormal signal corresponds to hemorrhage and edema with areas of fractured trabecula. Marrow contusion of the medial femoral condyle and moderate-sized joint effusion are seen.
-
Extensor mechanism injuries of the knee. Axial fast spin-echo proton density-weighted image with fat suppression in a 28-year-old man following a fall resulting in blunt anterior knee trauma demonstrates fissuring of the medial patellar cartilage with underlying subchondral marrow edema. Abnormal fluid signal intensity extends in a linear fashion from the articular surface to involve the deep cartilage layer.
-
Extensor mechanism injuries of the knee. This 42-year-old woman was referred for evaluation of chronic anterior knee pain for 2 years following a motor vehicle accident. Sagittal T1-weighted image demonstrates areas of focal decreased signal involving the posterior aspect of the patella and the medial femoral condyle, consistent with areas of chronic osteochondral injury (osteochondritis dissecans). With the knee flexed, these areas are aligned (kissing contusions). This pattern is consistent with focal areas of traumatic osteochondral injury from impaction during the motor vehicle accident.
-
Extensor mechanism injuries of the knee. Sagittal T1-weighted images in a 29-year-old man with chronic infrapatellar knee pain demonstrate a focal area of abnormal increased signal intensity in the proximal portion of the patellar tendon at the bone-tendon insertion. This involves the posterior portion of the tendon more extensively and is associated with focal enlargement of the tendon. Sparing of the anterior component of the tendon is typical of chronic patellar tendonitis (jumper's knee) and helps distinguish this condition from an acute process. Note the lack of subcutaneous edema in this patient.
-
Extensor mechanism injuries of the knee. Patellar avulsion fracture resulting from acute trauma as a result of a football injury. Sagittal FSE T2-weighted image with fat suppression demonstrates an avulsion fracture from the lower pole of the patella (arrow) and associated tear of the patellar tendon (arrow) (Image courtesy of Gary Gold, Stanford University).
-
Extensor mechanism injuries of the knee. Sagittal fast spin-echo proton density-weighted images with fat suppression images in a 40-year-old man with anterior knee pain following trauma demonstrates diffuse thickening of the infrapatellar tendon as well as linear areas of abnormal intermediate signal intensity within the substance of the tendon. Findings are consistent with an acute partial tear of the patellar tendon. Chronic patellar tendonitis complicated by chronic tears associated with inflammation and necrosis can appear similar on MRI; however, in this patient, subcutaneous edema anterior to the tendon also is seen, suggesting a relatively acute injury.
-
Extensor mechanism injuries of the knee. Sagittal T1-weighted image in a 68-year-old man demonstrates abnormal thickening of the quadriceps tendon associated with areas of linear abnormal increased signal intensity within the substance of the tendon (arrow). This is consistent with a partial tear of the quadriceps tendon in this patient with acute injury. The normal tendon typically has a laminated appearance. Fusiform thickening and loss of normal sharp margins of the quadriceps laminae are common manifestations of injury.
-
Extensor mechanism injuries of the knee. FSE T2-weighted image demonstrating complete tear of the quadriceps tendon in 67-year-old man. Retraction of the quadriceps tendon consistent with complete tear is observed (arrow) with mild undulating contour of the patellar tendon. (Image courtesy of Douglas Goodwin, Dartmouth-Hitchcock Medical Center).
-
Extensor mechanism injuries of the knee. Axial fast spin-echo T2-weighted image with fat suppression in a 21-year-old soccer player demonstrates focal abnormal high signal intensity centered on the tendon of the rectus femoris, at the musculotendinous junction. The location and appearance is indicative of a partial tear of the musculotendinous junction. These tears usually are seen in young athletes and are associated with either forced muscle contraction or direct injury.
-
Extensor mechanism injuries of the knee. Axial fast spin-echo T2-weighted image with fat suppression in this 38-year-old woman presenting after direct trauma to the knee demonstrates abnormal increased signal intensity in the vastus medialis oblique muscle consistent with myositis and edema from a partial tear. The vastus medialis oblique muscle provides dynamic medial force on the patella and is an important stabilizer for patellar tracking.
-
Extensor mechanism injuries of the knee. Sagittal fast spin-echo T2-weighted image with fat suppression in a 58-year-old woman demonstrates a complex fluid collection anterior to the knee in the region of the prepatellar bursa. The wall of the prepatellar bursa is thickened and irregular in appearance, consistent with chronic prepatellar bursitis. Note the underlying degenerative changes of the knee joint associated with osteophytic spurring. Irregularity of the Hoffa fat pad and a complex Baker cyst consistent with synovitis are seen. Synovial inflammatory processes can predispose patients to prepatellar bursitis.
-
Extensor mechanism injuries of the knee. In this 27-year-old female marathon runner with anterolateral pain superior to the joint line, coronal fast spin-echo T2-weighted image with fat suppression demonstrates edema between the iliotibial band and lateral femoral condyle (arrow). The location of edema is consistent with the clinical diagnosis of iliotibial band friction syndrome.
-
Extensor mechanism injuries of the knee. Sagittal gadolinium-enhanced T1-weighted image with fat suppression in a 32-year-old man demonstrates thickened, irregular, abnormally enhancing synovium and a thick enhancing suprapatellar plica (arrow). A large joint effusion is present as well, which aids in evaluating the abnormal appearing synovium and plica by distending the joint space.
-
Extensor mechanism injuries of the knee. A 19-year-old female runner with a long-standing history of anterior knee pain. Sagittal T2-weighted gradient-echo image demonstrates an irregular area of abnormal signal intensity in the Hoffa fat pad, which represents focal scarring and fibrosis. This is consistent with Hoffa disease, which is believed to result from repetitive impingement of the infrapatellar fat pad. Short term, increased signal intensity in the fat pad is seen on T2-weighted images. Long term, as in this patient, the subsequent fibrosis results in decreased signal intensity. Focal hypointensity on gradient-echo image is indicative of prior hemorrhage with hemosiderin deposits in the area of fibrosis.
-
Extensor mechanism injuries of the knee. Osteochondrosis of the tibial tuberosity: A sagittal T1-weighted image demonstrates bony fragmentation and irregularity of the tibial tuberosity. These findings are compatible with chronic Osgood-Schlatter condition in the appropriate clinical setting.
-
Extensor mechanism injuries of the knee. Painful bipartite patella. This 33-year-old man has a 2-year history of pain over the superolateral aspect of the patella. Axial fast spin-echo proton density-weighted image with fat suppression demonstrates a large amount of edema in the synchondrosis, superolateral fragment, and adjacent soft tissues. Painful bipartite patella is a rare condition believed to be related to chronic stress fracture and fibrous nonunion.
-
Extensor mechanism injuries of the knee. Acute patellar dislocation. The findings of joint effusion, medial retinacular tear, and marrow edema of the medial patellar facet are common sequelae of acute patellar dislocation.






