Practice Essentials
The anterior cruciate ligament (ACL) is the most commonly injured of the major knee ligaments. These injuries plague both athletes and nonathletes. The ACL is a vital ligamentous stabilizer of the knee that resists anterior translation and secondarily resists varus and valgus forces. [1] The ACL also functions as a mechanoreceptor that relays information about knee tension to the central nervous system. Patients with ACL injury have variable knee instability that may limit even ordinary daily activities. They experience particular difficulty pivoting and ambulating on uneven surfaces. The torn ACL undergoes limited healing. Long-term morbidity is common with sequelae, including osteoarthritis and secondary meniscal tears. [2, 3, 4, 5, 6]
A primary role of MRI in the management of the patient with an ACL injury lies in allowing confident diagnosis or exclusion of a tear in patients with equivocal physical examination findings. It should be emphasized, however, that ACL injury management is critically dependent on accurate diagnosis of other coexisting knee internal derangements, in particular tears of the lateral collateral ligament (LCL), posterior cruciate ligament (PCL), and the menisci. [7, 8, 9, 10, 11, 12, 13] In a study of Olympic athletes who underwent at least one knee MRI, it was determined that ACL sprains had a significant association with medial and lateral meniscal tears and bone contusions. [14]
(See the image below.)
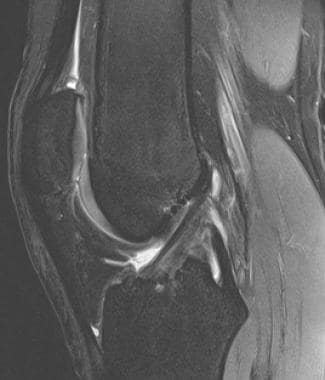
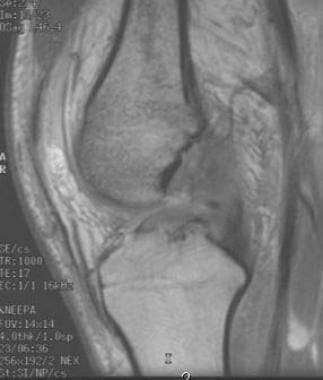
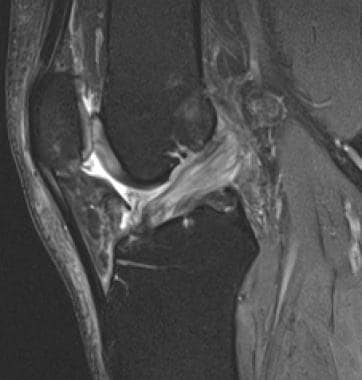
 Acute anterior cruciate ligament (ACL) tear. T2-weighted sagittal image in 22-year-old woman. Females have a variably increased incidence of ACL injury per hour of participation in activities at risk.
Acute anterior cruciate ligament (ACL) tear. T2-weighted sagittal image in 22-year-old woman. Females have a variably increased incidence of ACL injury per hour of participation in activities at risk.
Patients with combined LCL/ACL or PCL/ACL injuries often have profound instability requiring aggressive surgical management. In the instance of a coexisting LCL tear, intervention may be hastened, as LCL injuries are optimally repaired within 1-3 weeks. An unoperated LCL tear predisposes an ACL graft to early failure. [15, 16, 17, 18]
(See the image below.)
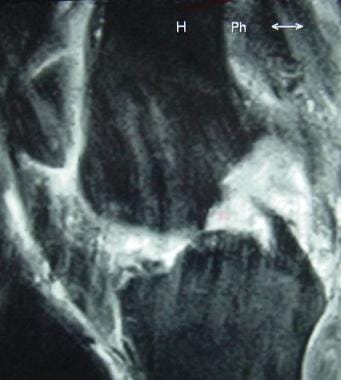
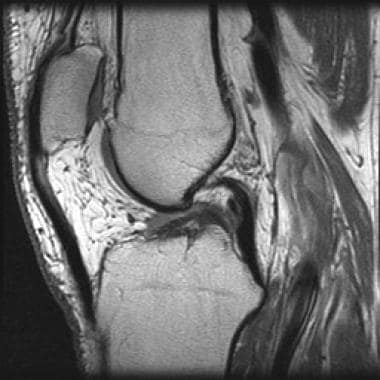
 Biceps femoris (lateral collateral ligament complex) injury in patient with anterior cruciate ligament (ACL) tear. Coronal T2-weighted image. Orthopedic surgeons often opt to operate earlier than customary in ACL-injured patients who also have a lateral collateral ligament (LCL) tear. This highlights the importance of accurate diagnosis of comorbid injuries in the ACL-injured patient.
Biceps femoris (lateral collateral ligament complex) injury in patient with anterior cruciate ligament (ACL) tear. Coronal T2-weighted image. Orthopedic surgeons often opt to operate earlier than customary in ACL-injured patients who also have a lateral collateral ligament (LCL) tear. This highlights the importance of accurate diagnosis of comorbid injuries in the ACL-injured patient.
Vincken et al noted that it is the evaluation of the knee joint as a whole (the composite diagnosis) that is central to appropriate selection of patients for therapeutic arthroscopy. The high reported composite sensitivity and specificity of knee MRI (87-94% and 88-93%, respectively) indicates MRI should serve well in this role. [7, 19] A study by Thomas et al concluded that while MRI may be overused in high-probability ACL-meniscal injury settings, a negative MRI largely excludes derangements that will benefit from arthroscopy. [20]
While accurate in the diagnosis of ACL injury, MRI findings are not helpful in ruling in or ruling out knee instability. Evaluation of instability enters strongly into the decision to opt for conservative or surgical treatment, and this remains a clinical assessment. [21]
The American College of Radiology (ACR) published guidelines for imaging acute trauma to the knee and stated that plain radiographs are usually appropriate for initial evaluation. The ACR recommended MRI without IV contrast as the most approriate follow-up study if no fracture is found and internal derangement is suspected. [22]
Clinical diagnosis
The skilled clinician can diagnose as many as 90% of ACL tears based on history and physical examination findings. [23, 24] Patients typically report an audible pop and "giving way" at the time of injury. A knee effusion usually develops over the next 24 hours. A tear is confirmed by physical examination, primarily by performing the Lachman test. [1] The anterior drawer and pivot shift tests are often helpful, and arthrometric examination may be contributory. Arthroscopy and arthrotomy are the criterion standards for diagnosis, but they are obviously more invasive and costly. [25, 26, 27, 28, 29]
Physical diagnosis is particularly difficult in large patients, in patients with strong secondary muscular restraints, and in patients with an acute injury and soft-tissue swelling and guarding. Partial ACL tears are also difficult to diagnose on physical examination. [30] MRI may provide pivotal diagnostic information about the ACL in all of these settings. [7, 31]
Treatment
Treatment of ACL tears ranges from conservative therapies (bracing and physical rehabilitation) to surgical ACL reconstruction. [32] More limited surgical interventions such as native ligament repair or augmentation have gained little traction in the orthopedic community. [33]
The patient's activity level (and expectation for activity in the future) is the most important factor guiding the choice of treatment. [1] Associated meniscal and ligamentous injuries, the degree of laxity, and the patient's age and willingness to pursue vigorous postoperative physical therapy are other major determinants.
ACL graft reconstruction stabilizes the ACL-deficient knee, thus increasing the range of activities tolerated and preventing reinjury from repeated subluxation. ACL reconstruction, however, has not been proven definitively to prevent long-term osteoarthritic deterioration. [1, 34] A study by Potter et al provides some evidence of chondroprotective effects of surgery in the medial and patellofemoral compartments. This study, however, concluded that all patients with an ACL injury incur articular chondral injuries and that variable progression of osteoarthritis develops over time in any or all of the 3 knee compartments, accelerating at 5-7 years after injury. [35]
ACL reconstruction is typically delayed several weeks or months until swelling has subsided and range of motion is restored. It is purported that late surgery decreases postprocedural stiffness; however, the effect on long-term outcomes is less clear. [1] Longer delays before surgery (>1 year) have been associated with an increasing incidence of various internal derangements, especially medial meniscal tears. [36, 37]
Anatomy
The anterior cruciate ligament (ACL) is a dense fibrous band composed of collagen fibrils. It is approximately 3.5-3.8 cm long and 1 cm in transverse diameter. [38] The ligament originates from the posteromedial aspect of the lateral femoral condyle (well posterior to the longitudinal mid axis of the femur) in the intercondylar notch. It courses through the notch in an anterior, inferior, and medial direction. [2] The distal ligament diverges, forming a roughly 11-19 mm horseshoe-shaped tibial insertion footprint. It inserts well posterior on the tibia, averaging 23 mm posterior to the anterior edge. The ligament does not typically insert directly on the medial intercondylar eminence (medial tibial spine), instead inserting just anterior and lateral to it. [38, 39] The ACL is not as strong as the posterior cruciate ligament (PCL), and it is less strong at its femoral origin than at its tibial insertion. [38]
(See the images below.)
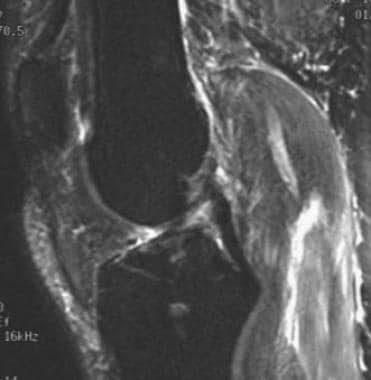
 Anterior cruciate ligament (ACL) anatomy in the sagittal plane. Sagittal T1-weighted image. The ACL arises from the posterior aspect of the medial surface of the lateral femoral condyle, high in the intercondylar notch. It courses obliquely anterior, bands diverging distally, to insert on the tibia well posterior to the anterior margin. The ligament is low signal in nature due to its collagenous nature, but higher signal than the posterior cruciate ligament (PCL).
Anterior cruciate ligament (ACL) anatomy in the sagittal plane. Sagittal T1-weighted image. The ACL arises from the posterior aspect of the medial surface of the lateral femoral condyle, high in the intercondylar notch. It courses obliquely anterior, bands diverging distally, to insert on the tibia well posterior to the anterior margin. The ligament is low signal in nature due to its collagenous nature, but higher signal than the posterior cruciate ligament (PCL).
 ACL anatomy in the coronal plane. Coronal T1-weighted MRI shows the lateral position of the ACL in the intercondylar notch (arrow), surrounded by high-signal fat. Note the slanted course of the ligament. The ACL bundles diverge distally at their tibial insertion medial to the anterior intercondylar eminence.
ACL anatomy in the coronal plane. Coronal T1-weighted MRI shows the lateral position of the ACL in the intercondylar notch (arrow), surrounded by high-signal fat. Note the slanted course of the ligament. The ACL bundles diverge distally at their tibial insertion medial to the anterior intercondylar eminence.
 Anterior cruciate ligament (ACL) anatomy in the axial plane. A fat-saturated neutral-weighted MRI shows the collagenous low-signal ACL positioned in the lateral aspect of the intercondylar notch (arrow). Distally (not shown) the ACL moves away from the wall and diverges into a horseshoe-array of multiple fascicles.
Anterior cruciate ligament (ACL) anatomy in the axial plane. A fat-saturated neutral-weighted MRI shows the collagenous low-signal ACL positioned in the lateral aspect of the intercondylar notch (arrow). Distally (not shown) the ACL moves away from the wall and diverges into a horseshoe-array of multiple fascicles.
The ACL is organized into anteromedial and posterolateral bundles. The bundles are named for their locations relative to each other at their tibial insertion. [38, 40] The biomechanics of the bundles are complex and are under increasing investigation. It is generally stated that the anteromedial bundle tightens with flexion of the knee and resists anterior translation of the tibia in flexion, while the bulkier and less isometric posterolateral bundle tightens with knee extension and resists hyperextension. [38] The physiologic property in which different parts of the spriraled ACL are taut at different points in the normal range of motion is termed isometry. Graft isometry is a stated goal of reconstructive surgery: the differing attachments and roles of the 2 bundles are the basis for the current intense investigational interest in double-bundle ACL reconstruction surgery.
Interestingly, Smigielski et al dissected 111 cadavers and found that the ACL consistently demonstrates a flattened ribbon-like segment just 2 mm from its femoral origin that is devoid of double bundle anatomy. [41]
Cadaver and clinical studies have shown the normal anteromedial and posterolateral bundles to be distinguishable in most patients at 3-Tesla. [42, 43, 44] Visualization of bundle anatomy is limited at 1.5 Tesla and low-field MRI imaging.
(See the image below.)
 Normal double bundle anterior cruciate ligament (ACL) anatomy. Axial and coronal proton density-weighted fat-saturation 3-Tesla images demonstrate normal anteromedial and posterolateral bundles in 2 different patients.
Normal double bundle anterior cruciate ligament (ACL) anatomy. Axial and coronal proton density-weighted fat-saturation 3-Tesla images demonstrate normal anteromedial and posterolateral bundles in 2 different patients.
The ACL is an extrasynovial and intracapsular ligament. Bands of mesentery-like synovium, arising from the posterior intercondylar region of the tibia, surround the cruciate ligaments. [38] This feature accounts for fluid often seen anterior to the normal ACL (and posterior to the PCL) on MRI. The extrasynovial location also helps explain why hemarthrosis is often delayed in the setting of an acute ACL tear.
The primary blood supply to the ACL derives from arteries to the surrounding synovial membrane. These, in turn, derive from branches of the middle geniculate artery piercing the posterior capsule. [38] The central core of the ACL is relatively avascular. This helps explain the generally ineffective healing of ACL tears. Tibial nerve terminal branches innervate the ACL. [38] Sensory mechanoreceptors are present, and this causes loss of proprioception in ACL-injured patients that can be clinically significant.
Mechanism of Injury
Mechanisms of anterior cruciate ligament (ACL) injury are numerous. Alpine-skiing ACL injury studies have served to demonstrate the complexity of this subject: a welter of characteristic mechanisms of injury have been identified in skiers, including aggressive quadriceps contraction, boot-induced injuries, "phantom foot" injuries, hit-from-behind injuries, and various types of valgus, rotatory, and hyperextension injuries.
ACL tears occur with or without contact and with the knee in any position from flexed to fully extended. A well-known contact mechanism of injury is the valgus-abduction clip injury. [39] These injuries are frequent in football players and occur with a lateral blow to the partially flexed knee. A study of 2460 knee injuries in students playing football at American universities found that playing on artificial turf resulted in ACL injuries at 1.63 times the rate of injuries resulting from playing on natural grass. [45] Coexisting medial and lateral meniscal tears are common, as are medial collateral ligament (MCL) injuries.
Hyperextension or varus-hyperextension from an anterior blow (eg, injury from a motor vehicle accident or contact sports) is the second most common contact mechanism of ACL injury. The posterior cruciate ligament (PCL) and posterolateral-corner structures are also frequently injured. With more severe hyperextension, the knee may dislocate; the popliteal neurovascular bundle or peroneal nerve may be injured in this setting.
(See the image below.)
 Hyperextension anterior "kissing" bone bruises in patient with anterior cruciate ligament (ACL) tear. Sagittal T2-weighted image in 25-year-old man. Anterior bone bruises of this nature indicate a hyperextension mechanism of injury. The reader should thus be alert for the possibility of ACL, posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and neurovascular injuries. (This patient had ACL and LCL tears.)
Hyperextension anterior "kissing" bone bruises in patient with anterior cruciate ligament (ACL) tear. Sagittal T2-weighted image in 25-year-old man. Anterior bone bruises of this nature indicate a hyperextension mechanism of injury. The reader should thus be alert for the possibility of ACL, posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and neurovascular injuries. (This patient had ACL and LCL tears.)
Noncontact mechanisms actually account for the majority (70-80%) of ACL tears. [39, 46] The pivot-shift mechanism (see the images below) is most commonly implicated: the slightly flexed knee incurs a valgus load, with internal rotation of the tibia or external rotation of the femur. Some studies indicate that the initial loading of the ACL is due to anterior drawer translation of the lateral tibia (marked quadriceps loading implicated), with the pivot-shift rotation occurring microseconds later. [46] These pivot-shift injuries often occur with rapid simultaneous deceleration and directional movements in skiers and football, basketball, and soccer players. Again, associated meniscal tears and collateral ligament injuries are common (much less often, lateral patellar subluxation).
(See the image below.)
 Pivot-shift twisting mechanism lateral bone bruises in a patient with anterior cruciate ligament (ACL) tear. T2-weighted sagittal image in 22-year-old woman. This pattern of lateral bone bruises occurs with lateral rotation of the femur relative to the tibia and indicates a very high likelihood of an associated ACL injury. This patient had meniscal and medial collateral ligament (MCL) injuries in addition to an ACL tear.
Pivot-shift twisting mechanism lateral bone bruises in a patient with anterior cruciate ligament (ACL) tear. T2-weighted sagittal image in 22-year-old woman. This pattern of lateral bone bruises occurs with lateral rotation of the femur relative to the tibia and indicates a very high likelihood of an associated ACL injury. This patient had meniscal and medial collateral ligament (MCL) injuries in addition to an ACL tear.
Noncontact hyperextension, such as that occurring in a gymnast or cheerleader who misses a landing, is another mechanism of injury that often injures the ACL. [39]
The incidence of ACL tears in females is higher than that in males for each hour of participation in activities at risk. A relative risk of up to 10 times higher has been suggested; however, a review of the literature by Prodromos et al suggests a more modest 3.5 times greater risk (basketball being the sport with the greatest sex differential). [47, 48] Explanations for this increased susceptibility are under debate. [49] Lax joints, more common in females, appears to predispose patients to ACL injury. [50, 51]
MRI Technique for ACL Evaluation
Relevant history and physical examination findings should be provided to the MRI reader. Especially helpful is history regarding previous knee surgeries and dates of injuries. The authors have found it beneficial for technologists to place MRI markers at sites of pain and surgical scars.
Imaging protocols
Knee MRI protocols must be designed to yield diagnostic images of not only the anterior cruciate ligament (ACL), but also the menisci, bones, articular cartilage, and other ligamentous structures of the knee. Furthermore, the requirements for optimal meniscus and cartilage imaging are more exacting than the requirements for diagnostic ACL imaging. As such, for the most part, a protocol that images the menisci and cartilage optimally also adequately demonstrates the ACL. This explains why most centers image patients in full knee extension, though the ACL is optimally evaluated with the knee in about 30° of flexion. Imaging in flexion complicates evaluation of the menisci and other knee structures. [52]
The minimal protocol requirements of ACL imaging include T2-weighted sequences (or proton-weighted fat-suppressed) in 2-3 orthogonal planes. [53, 54] Most centers perform at least one T1-weighted sequence in either the sagittal or coronal plane.
T2-weighted sequences are most important in diagnosing acute ACL injuries. [55, 56] This is due in part to confounding increased signal intensity seen in ligaments and tendons in short-echo time T1 and gradient-echo sequences. This, in turn, is related to internal degeneration, magic-angle artifact, and other factors. Fast spin-echo fat-saturation sequences (termed turbo spin-echo by some vendors) are faster and more sensitive to injury than conventional T2-weighted spin-echo images and have largely replaced these sequences.
Any of the 3 imaging planes may prove pivotal to interpretation in a given case (see the images below). The MRI reader should routinely inspect the ACL in all planes and become familiar with the range of normal and abnormal in each plane. Axial images in particular provide a cross-sectional perspective free of partial volume artifact with the intercondylar roof and are invaluable in evaluation of the proximal ACL. [53, 57, 58, 59]
(See the images below.)
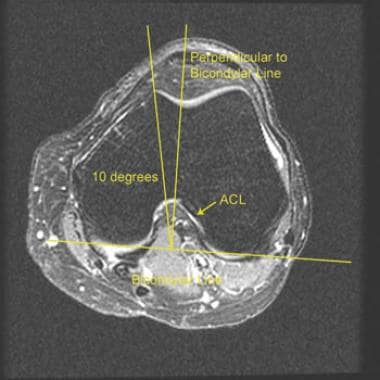 Prescribing sagittal images. Images are prescribed on a scout axial image off a line tangent to the femoral condyle posterior margins (the bicondylar line). Most centers now generate images perpendicular to the bicondylar line. Slightly oblique images may be obtained but should be no more than 10 degrees off perpendicular. Prescribing images along the axial plane long axis of the ACL is discouraged; this will usually lead to overly oblique sagittal images with degraded visualization of the menisci and other knee structures.
Prescribing sagittal images. Images are prescribed on a scout axial image off a line tangent to the femoral condyle posterior margins (the bicondylar line). Most centers now generate images perpendicular to the bicondylar line. Slightly oblique images may be obtained but should be no more than 10 degrees off perpendicular. Prescribing images along the axial plane long axis of the ACL is discouraged; this will usually lead to overly oblique sagittal images with degraded visualization of the menisci and other knee structures.
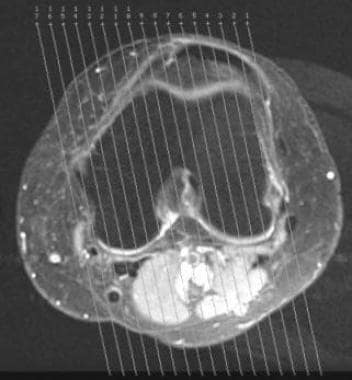 Example of prescribed sagittal images on axial scout image. In this case, images were obtained oblique to a line perpendicular to the bicondylar line. Care should be taken to avoid over-obliquity of sagittal images.
Example of prescribed sagittal images on axial scout image. In this case, images were obtained oblique to a line perpendicular to the bicondylar line. Care should be taken to avoid over-obliquity of sagittal images.
Other technical considerations
Several methods for the prescription of sagittal images of the ACL by the MRI technologist have evolved over time. Early recommendations were to allow patients to naturally externally rotate their legs and then to prescribe longitudinal images perpendicular to the table. However, this method leads to suboptimal, inconsistent results.
The subsequent recommendation was to perform sagittal oblique slices 10-15° off a perpendicular to a bicondylar line tangent to the posterior margins of the medial and lateral femoral condyles on an axial scout image, thus aligning images closer to the long axis of the ACL.
Garner et al demonstrated that the true sagittal plane (perpendicular to the bicondylar line) is superior for evaluation of the ACL. [60] This also restores optimal meniscal evaluation. The authors have noted the same and recommend this simpler approach.
Additional problem-solving sequences
Most MRI vendors provide for a number of 3-dimensional thin-slice isotropic imaging options, including isotropic fast spin-echo sequences. These acquisitions allow equal high-resolution reformatting in any desired plane. Such data sets are now acquired routinely in the knee protocols of most modern imaging centers (including those of the authors). With an indeterminate ACL, the imager may sit at a workstation and post-process high-resolution ACL images in any desired plane. Further studies, however, are needed to determine the value added by these 3-dimensional isotropic data sets.
Other special problem-solving oblique ACL sequences have not found wide application but clearly may be helpful in equivocal cases. Katahira et al reported increased ACL diagnostic accuracy prescribing oblique coronal images parallel to the long axis of the ACL as prescribed off of an oblique sagittal image (the sagittal image was in turn prescribed off a coronal image). [61] This is termed a "double-oblique" sequence. Park et al reported improved diagnosis of single bundle tears on 3-T scanners with oblique coronal sequences prescribed off a sagittal image. [62] Several other investigators have also reported improved diagnosis prescribing oblique imaging along the ACL long axis. [63, 64, 65, 66]
(See the images below.)
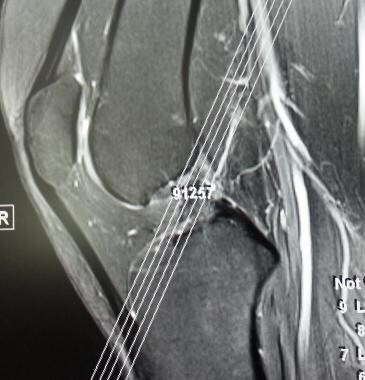 Problem-solving oblique coronal sequence. This additional sequence may be helpful in equivocal ACL-tear cases. On a sagittal scout image, the MRI technologist prescribes thin (3mm or less) T2-weighted or proton-density-weighted fat suppression images along the long axis of the ACL.
Problem-solving oblique coronal sequence. This additional sequence may be helpful in equivocal ACL-tear cases. On a sagittal scout image, the MRI technologist prescribes thin (3mm or less) T2-weighted or proton-density-weighted fat suppression images along the long axis of the ACL.
 Problem-solving oblique coronal sequence. Note how the entire proximal-to-distal ACL is visible on one coronal image. On conventional coronal images, the ACL is visualized on multiple successive slices. Note: we ordinarily perform this extra sequence with a smaller field-of-view than evident here.
Problem-solving oblique coronal sequence. Note how the entire proximal-to-distal ACL is visible on one coronal image. On conventional coronal images, the ACL is visualized on multiple successive slices. Note: we ordinarily perform this extra sequence with a smaller field-of-view than evident here.
In equivocal cases, the MRI reader may also try imaging the knee in mild flexion. ACL imaging is improved, in part because of decreased partial voluming of the proximal ACL with the intercondylar roof. [52, 67]
(See the image below.)
 Problem-solving sequence with knee in flexed position. This sequence may be helpful when conventional MRI sequences demonstrate an equivocal proximal ACL tear near its origin off the femur. This patient is actually status post ACL graft reconstruction. Note the helpful separation of the anterior aspect of the proximal ACL from the intercondylar roof, allowing optimal evaluation.
Problem-solving sequence with knee in flexed position. This sequence may be helpful when conventional MRI sequences demonstrate an equivocal proximal ACL tear near its origin off the femur. This patient is actually status post ACL graft reconstruction. Note the helpful separation of the anterior aspect of the proximal ACL from the intercondylar roof, allowing optimal evaluation.
Normal ACL MRI Appearance
Normal MRI appearances
On sagittal images, the normal anterior cruciate ligament (ACL), as shown in the image below, appears as a solid band or as a striated band diverging slightly distally. Interestingly, while the ACL is known to be composed predominantly of anteromedial and posterolateral bands, as many as 4 distinct striations may be visible. [54] The ACL is usually ruler-straight; however, mild convex-inferior sagging may be evident in normal ACLs.
 Normal anterior cruciate ligament (ACL) in sagittal plane. T2-weighted image in 25-year-old woman. The robust ligament demonstrates uninterrupted low-signal linear bands. It is nonangulated and either ruler-straight or demonstrating minimal convex-inferior sagging. The long axis of a normal ligament should be at least as steep as the nearby intercondylar roof.
Normal anterior cruciate ligament (ACL) in sagittal plane. T2-weighted image in 25-year-old woman. The robust ligament demonstrates uninterrupted low-signal linear bands. It is nonangulated and either ruler-straight or demonstrating minimal convex-inferior sagging. The long axis of a normal ligament should be at least as steep as the nearby intercondylar roof.
The ACL substance shows slightly higher signal than that of the adjacent posterior cruciate ligament (PCL), with low-to-intermediate intensity. The distal ACL further demonstrates relatively increased signal intensity, in part because of distal divergence of bands/striations. Data from one study confirmed that the increased internal signal intensity is the result of macroscopic (rather than histologic) features of the ACL, although in elderly patients, internal degeneration accounts for some of the observed increased signal intensity. [68]
On coronal images, a normal ACL (see the image below) is usually well seen, although the band (or bands) often appears much more attenuated and less bulky than in the sagittal plane. The lateral position of the ACL in the femoral intercondylar notch is apparent in the coronal plane; the PCL is seen medially. In normal ACLs, ample fat signal is seen in the notch surrounding the cruciate ligaments.
 Normal anterior cruciate ligament (ACL) in coronal plane. T2-weighted image in 25-year-old woman. In this plane, the normal ACL often appears much more attenuated than in the sagittal plane. Again, however, the ACL manifests as one or several straight, nonangulated, distally diverging low-signal bands. In this patient, the anteromedial and posterolateral bundles are readily differentiated. Note the lateral position of the ACL in the intercondylar notch. Note also the predominant fat signal surrounding the ACL: this is usually replaced by edema in the setting of an acute tear.
Normal anterior cruciate ligament (ACL) in coronal plane. T2-weighted image in 25-year-old woman. In this plane, the normal ACL often appears much more attenuated than in the sagittal plane. Again, however, the ACL manifests as one or several straight, nonangulated, distally diverging low-signal bands. In this patient, the anteromedial and posterolateral bundles are readily differentiated. Note the lateral position of the ACL in the intercondylar notch. Note also the predominant fat signal surrounding the ACL: this is usually replaced by edema in the setting of an acute tear.
In the axial plane, the proximal ACL is especially well seen (see the image below) and appears normally as an elliptical low-signal intensity band adjacent to the lateral wall of the upper intercondylar notch. It gradually moves away from the wall and splits into a horseshoe (fan-shaped) array of fascicles as it approaches its tibial insertion. [57] The distal ACL is difficult to critically evaluate on axial images.
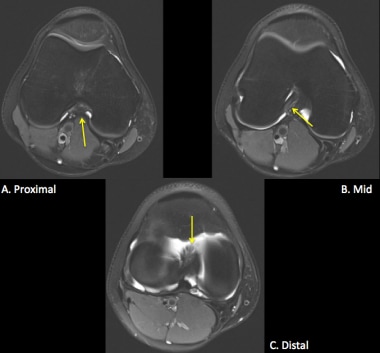 Normal anterior cruciate ligament (ACL) in the axial plane. T2-weighted images in 21-year-old woman. A. Proximal ACL. The ACL is low signal and cigar-shaped. It hugs the lateral wall of the high posterior intercondylar notch. B. Mid ACL. The ligament is coursing through the notch in anterior and medial direction. C. Distal ACL. The ACL diverges into a horseshoe-shaped array of fascicles near its insertion on the tibia. The distal ligament here is more difficult to critically evaluate.
Normal anterior cruciate ligament (ACL) in the axial plane. T2-weighted images in 21-year-old woman. A. Proximal ACL. The ACL is low signal and cigar-shaped. It hugs the lateral wall of the high posterior intercondylar notch. B. Mid ACL. The ligament is coursing through the notch in anterior and medial direction. C. Distal ACL. The ACL diverges into a horseshoe-shaped array of fascicles near its insertion on the tibia. The distal ligament here is more difficult to critically evaluate.
Normal distinct anteromedial and posterolateral bands are identifiable in the majority of patients imaged at 3-Tesla field strength (94% of patients in a study by Adriaensen et al [44] ). The posterolateral band is so named because of its relatively posterolateral tibial insertion, and this serves to explain the more vertical appearance of this band on sagittal and coronal plane images.
Pitfalls in interpreting normal findings
It is not uncommon for the ACL to be suboptimally demonstrated in healthy knees in the sagittal plane. [54] T1-weighted images are especially likely to demonstrate an ill-defined indeterminate ACL appearance. However, the absence of hemorrhage or edema in the expected location of the ACL, a normal appearance of the ACL in other planes, and the absence of secondary signs of ACL injury are almost always sufficient to confirm that the ACL is normal. [54] Smith et al noted that the ACL is highly likely intact when poorly visualized on either the T1- or T2-weighted sagittal sequence and normal in appearance on other sequences. [69]
Partial-volume superimposition of the inner aspect of the lateral femoral condyle on the proximal ACL may produce a pseudomass that mimics an acute ACL tear on sagittal images.
If section thicknesses of 4 mm or less are routinely used and if other imaging planes are correlated, this is not a diagnostic problem. [54]
(See the image below.)
 Partial-volume inclusion of the lateral femoral condyle causing a false appearance of an ACL tear. T1-weighted sagittal MRI shows an ill-defined pseudomass about the proximal ACL that could be taken as evidence for ACL injury. With evaluation of adjacent images and other imaging planes, this should not cause problems in interpretation.
Partial-volume inclusion of the lateral femoral condyle causing a false appearance of an ACL tear. T1-weighted sagittal MRI shows an ill-defined pseudomass about the proximal ACL that could be taken as evidence for ACL injury. With evaluation of adjacent images and other imaging planes, this should not cause problems in interpretation.
MRI Findings in Acute Injury
Studies report variable 78-100% sensitivity and 68-100% specificity of MRI for the diagnosis of anterior cruciate ligament (ACL) tears. [20, 70, 71, 8, 9, 72, 11, 73, 12] Accuracy of approximately 95% has been reported, with the diagnosis of proximal, partial, or chronic tears accounting for many of the persistent errors in interpretation. Sensitivity is also significantly decreased if other major ligamentous injuries are present in the knee. [74]
Less data are available for children than for adults. Decreased accuracy of MRI has been reported in preadolescents, [75] but a study of patients aged 5-16 years demonstrated a sensitivity of 95% and a specificity of 88%. [24]
Koch et al compared MRI diagnosis with arthroscopic findings in 218 consecutive knee arthroscopies with the following patient characteristics: age >15 years-old, primary arthroscopy, 1.5-Tesla MRI performed, and time interval from MRI to surgery < 6 months. The authors concluded from their findings that 1.5-Tesla MRI can accurately diagnose ACL and medial meniscal tears and reliably complete the diagnostic workup after physical examination but is not reliable for diagnosing short peripheral tears at the posterior horn of the medial meniscus and partial-thickness articular cartilage lesion of the femoral condyles. They suggested that for these lesions, definitive diagnosis may require cartilage-specific MRI sequences or direct arthroscopic evaluation. [76]
According to the Koch et al, the highest accuracy was observed in medial meniscus and in ACL findings. For the medial meniscus, sensitivity, specificity, agreement, and Kappa coefficient were 77, 92, 86%, and 0.7; for the ACL, the measures were 82, 97, 87%, and 0.73. MRI accuracy was lower in the lateral meniscus and articular cartilage, with Kappa coefficient 0.42 and 0.3, respectively. Also, short peripheral tears in the posterior horn of the medial meniscus were characteristic of false negative findings. [76]
In a meta-analysis by Phelan et al of 14 studies on the accuracy of MRI for ACL tears, 19 studies on medial meniscal tears, and 19 studies on lateral meniscal tears, sensitivity and specificity of MRI were 87% and 93%, respectively, for ACL tears; 89% and 88% for medial meniscal tears; and 78% and 95% for lateral meniscal tears. [9]
Van der List et al reported on preoperative MRI to help predict eligibility for arthroscopic primary ACL repair. Patients underwent either arthroscopic primary repair (in cases with sufficient tissue length and quality) or single-bundle ACL reconstruction. The modified Sherman classification was used to grade preoperative MRI tear locations, as follows: type I (>90% distal remnant length), type II (75-90%), type III (25-75%). MRI tissue quality was graded as good, fair, or poor. In this study of 63 repair patients and 67 reconstruction patients, the use of MRI tear location and tissue quality to predict eligibility for primary repair showed the following: 90% of all type I tears and 88% of type II tears with good tissue quality were repaired, while only 23% of type II tears with fair tissue quality, 0% of type II tears with poor tissue quality, and 14% of all type III tears could be repaired. [77]
ACL accuracy has not been shown to be significantly improved with 3-Tesla imaging, despite demonstrably improved visualization of distinct anteromedial and posterolateral bands. [44, 78, 79]
Most ACL tears (about 70%) occur in the middle aspect of the ligament [38] ; 7-20% occur proximally near its origin. Only 3-10% occur distally at the tibial attachment. [54]
Primary signs of ACL tear
Primary signs of acute ACL tear (ie, MRI abnormalities of the ACL proper) allow for high accuracy in the diagnosis of ACL injury, even in the absence of secondary signs. [24, 56, 80, 81, 82, 83]
(See the images below.)
 Nonvisualization as a primary sign of ACL tear. Complete (or near-complete) nonvisualization of the ACL on sagittal images with ill-defined edema and hemorrhage in the usual location of the ACL is a very common presentation of an acute tear. Note: the normal ACL is sometimes poorly seen on low–echo-time (T1 or gradient echo) sagittal images; this usually does not present a problem in interpretation if T2 images, and images in other planes are carefully correlated.
Nonvisualization as a primary sign of ACL tear. Complete (or near-complete) nonvisualization of the ACL on sagittal images with ill-defined edema and hemorrhage in the usual location of the ACL is a very common presentation of an acute tear. Note: the normal ACL is sometimes poorly seen on low–echo-time (T1 or gradient echo) sagittal images; this usually does not present a problem in interpretation if T2 images, and images in other planes are carefully correlated.
 Nonvisualization of the ACL as a primary sign of a tear in a T2-weighted sequence. Sagittal T2-weighted fat-saturated fast spin-echo (FSE) image shows replacement of the ACL in the intercondylar notch by extensive edema-fluid signal intensity.
Nonvisualization of the ACL as a primary sign of a tear in a T2-weighted sequence. Sagittal T2-weighted fat-saturated fast spin-echo (FSE) image shows replacement of the ACL in the intercondylar notch by extensive edema-fluid signal intensity.
 Focal interruption as a primary sign of anterior cruciate ligament (ACL) tear. T2-weighted image shows focal hyperintense edema and/or fluid involving the proximal ACL.
Focal interruption as a primary sign of anterior cruciate ligament (ACL) tear. T2-weighted image shows focal hyperintense edema and/or fluid involving the proximal ACL.
 Angulation/nonlinearity as a primary sign of anterior cruciate ligament (ACL) tear. T1-weighted sagittal MRI shows an abruptly angulated mid ACL (arrow). The normal ACL occasionally has a gently curved, convex-inferior appearance, but a wavy or sharply angulated appearance is abnormal.
Angulation/nonlinearity as a primary sign of anterior cruciate ligament (ACL) tear. T1-weighted sagittal MRI shows an abruptly angulated mid ACL (arrow). The normal ACL occasionally has a gently curved, convex-inferior appearance, but a wavy or sharply angulated appearance is abnormal.
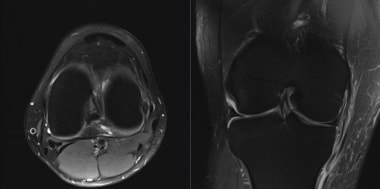
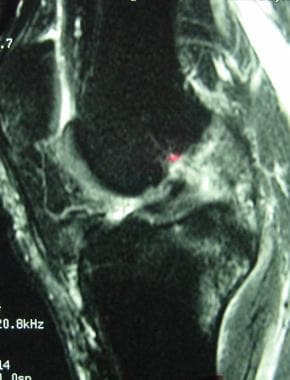
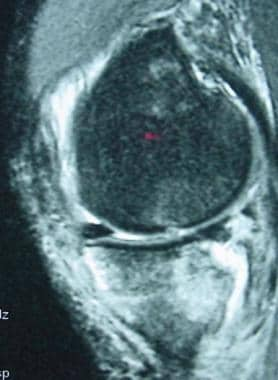
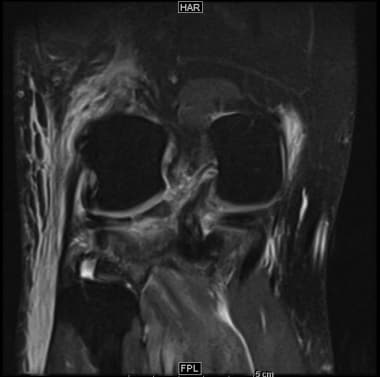
 Primary signs of an ACL tear. Sagittal image (top left) demonstrates high-signal disruption of the ACL with multifragmented appearance. Coronal T2 (top right) and T1 (below) images show nonvisualization of ACL fibers and abnormal increased edema and fluid in the lateral intercondylar notch.
Primary signs of an ACL tear. Sagittal image (top left) demonstrates high-signal disruption of the ACL with multifragmented appearance. Coronal T2 (top right) and T1 (below) images show nonvisualization of ACL fibers and abnormal increased edema and fluid in the lateral intercondylar notch.
 Flattened axis of the distal ACL as a primary sign of ACL tear. This sign has very high specificity for ACL injury. Visualization of the proximal ACL is poor, further confirming tear.
Flattened axis of the distal ACL as a primary sign of ACL tear. This sign has very high specificity for ACL injury. Visualization of the proximal ACL is poor, further confirming tear.
 Subtle flattened axis as a primary sign of ACL tear. Sagittal T2-weighted image MRI shows axis of the ACL (arrowhead) to be slightly more horizontal than that of the intercondylar roof, or Blumensaat line (arrow), in this patient with arthroscopically proven ACL tear.
Subtle flattened axis as a primary sign of ACL tear. Sagittal T2-weighted image MRI shows axis of the ACL (arrowhead) to be slightly more horizontal than that of the intercondylar roof, or Blumensaat line (arrow), in this patient with arthroscopically proven ACL tear.
The primary signs of an ACL tear include nonvisualization, disruption of the substance of the ACL by abnormal increased signal intensity, abrupt angulation or a wavy appearance, and an abnormal ACL axis. The axis of the ACL is abnormal if it is clearly more horizontal than a line projected along the intercondylar roof (Blumensaat line) on sagittal images. The ACL axis can be quantitated (although the authors have not found this to be necessary). [84]
A common presentation of an acute ACL tear is nonvisualization of the ligament with replacement by an ill-defined cloud of focal edema and hemorrhage. A partial tear manifesting as enlargement of the ACL and increased internal signal intensity but with visible intact fascicles has been termed an interstitial tear (or delaminated tear). These appearances must be differentiated from mucoid degeneration of the intact ACL.
A torn or partially torn ACL stump may angle anteriorly into the anterior intercondylar notch, with or without nodule formation. This has been called the "bell-hammer sign," or the "preoperative cyclops syndrome " (analagous to focal arthrofibrotic cyclops lesions developing anterior to ACL grafts). [85, 86]
Axial images should be reviewed as diligently as the sagittal and coronal images for primary signs of ACL tear. The elliptical hypointense band representing the proximal ACL may be attenuated, fragmented, completely or partially replaced by hemorrhage, or displaced away from the lateral wall of the intercondylar notch. [57]
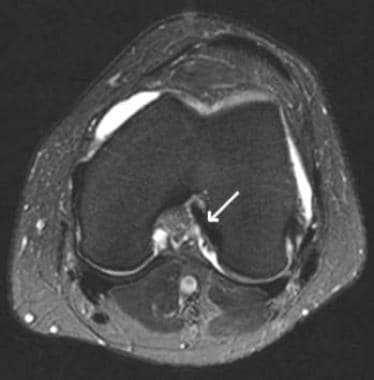
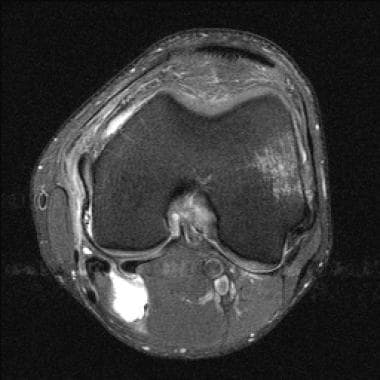
(See the images below.)
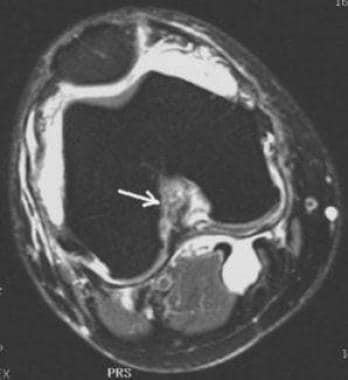 ACL tear on axial image. T2-weighted fat-saturated fast spin-echo axial image shows nonvisualization of the ACL in the upper intercondylar notch (arrow). A large knee effusion and a Baker cyst are noted incidentally.
ACL tear on axial image. T2-weighted fat-saturated fast spin-echo axial image shows nonvisualization of the ACL in the upper intercondylar notch (arrow). A large knee effusion and a Baker cyst are noted incidentally.
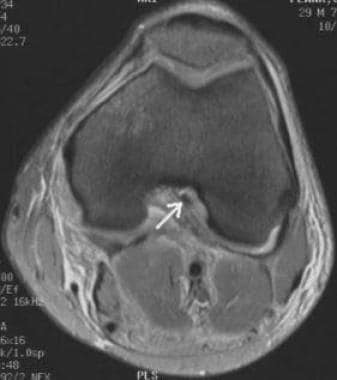 ACL tear on an axial image. Neutral-weighted fast spin-echo (FSE) fat-saturated MRI shows an abnormally truncated, small ACL remnant in the upper intercondylar notch (arrow). Surrounding edema is present.
ACL tear on an axial image. Neutral-weighted fast spin-echo (FSE) fat-saturated MRI shows an abnormally truncated, small ACL remnant in the upper intercondylar notch (arrow). Surrounding edema is present.
Secondary signs of ACL tear
MRI findings of an ACL tear apart from abnormalities of the ACL proper are termed secondary signs. The sensitivity of these signs is limited [80] ; therefore, the absence of secondary signs in no way excludes ACL disruption. Certain signs, however, have greater than 80% specificity for ACL injury. As a consequence, they may allow for a fairly confident diagnosis of tear when primary signs are equivocal. [80, 87, 81, 88, 89, 90, 91, 92, 93, 94, 95, 96]
Secondary signs with high specificity for ACL injury include pivot-shift bone bruises/osteochondral fractures and Segond fractures.
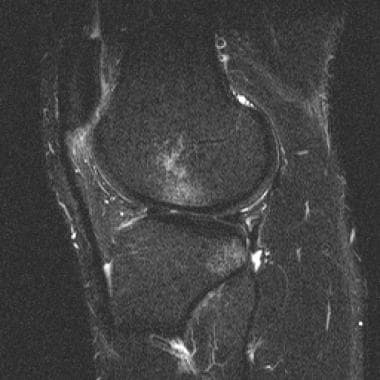
Pivot-shift bone bruises and fractures
With a pivot-shift rotatory injury of the ACL, there is external rotation of the lateral femoral condyle relative to the fixed tibia. This shift allows the lateral femoral condyle to impact the posterolateral tibial plateau, frequently causing characteristic bone bruises of one or both bones. [56, 92, 94] The lateral femoral condyle bone bruise is usually near the anterior horn lateral meniscus but may be more posteriorly located if the injury occurs during flexion. The tibial bone bruise subtends the posterolateral corner of the tibia.
(See the images below.)
 Pivot shift bone bruises of the femur and tibia as a secondary sign of an ACL tear. Sagittal T2-weighted fast spin-echo fat-saturated MRI shows typical pivot-shift subchondral bone bruises of the posterior lateral tibial plateau and lateral femoral condyle near the anterior horn meniscus. The probability of an ACL tear is very high if both pivot shift bone bruises are present, only slightly lower if either the tibial or femoral bone bruise is seen in isolation.
Pivot shift bone bruises of the femur and tibia as a secondary sign of an ACL tear. Sagittal T2-weighted fast spin-echo fat-saturated MRI shows typical pivot-shift subchondral bone bruises of the posterior lateral tibial plateau and lateral femoral condyle near the anterior horn meniscus. The probability of an ACL tear is very high if both pivot shift bone bruises are present, only slightly lower if either the tibial or femoral bone bruise is seen in isolation.
 Pivot-shift osteochondral fracture of the lateral femoral condyle. This is a sagittal gradient-echo MRI in 17-year-old boy with an arthroscopically proven ACL tear. The fracture is manifest by focal cortical indentation of lateral femoral condyle (arrow), near the anterior horn lateral meniscus. This fracture was accompanied by typical femoral and tibial pivot-shift bone bruises, as best demonstrated on T2-weighted sequences.
Pivot-shift osteochondral fracture of the lateral femoral condyle. This is a sagittal gradient-echo MRI in 17-year-old boy with an arthroscopically proven ACL tear. The fracture is manifest by focal cortical indentation of lateral femoral condyle (arrow), near the anterior horn lateral meniscus. This fracture was accompanied by typical femoral and tibial pivot-shift bone bruises, as best demonstrated on T2-weighted sequences.
 Deep lateral femoral notch (sulcus) sign as a secondary sign of anterior cruciate ligament (ACL) injury. A lateral radiograph demonstrates an unusually pronounced lateral condylopatellar groove. Such appearances should suggest to the reader the possibility of a pivot-shift impaction injury.
Deep lateral femoral notch (sulcus) sign as a secondary sign of anterior cruciate ligament (ACL) injury. A lateral radiograph demonstrates an unusually pronounced lateral condylopatellar groove. Such appearances should suggest to the reader the possibility of a pivot-shift impaction injury.
With more severe injury, osteochondral fractures may accompany these bone bruises. MRI demonstrates linear subchondral fracture lines or cortical contour flattening. Sagittal MRIs (and lateral radiographs) may reveal a "deep lateral femoral-notch sign" that manifests as an exaggerated (>1.5-mm-deep) condylopatellar notch of the lateral femoral condyle. [89, 97] Pivot-shift fractures of the posterolateral tibial plateau are easily seen on MRIs but are often occult on radiographs. These fractures manifest as subtle cortical impaction or as a posterior capsular bony avulsion fragment. [98]
Characteristic pivot-shift bone bruises (and osteochondral fractures) of the tibia or femur indicate a greater than 90% likelihood of ACL injury. [39] However, pivot-shift bone bruises can occur, in rare cases, without an associated ACL tear, usually in the pediatric or adolescent population. [99]
"Contrecoup" medial tibial bone bruises/impaction fractures may be seen with especially pronounced pivot-shift twisting injuries. These injuries involve the posteromedial tibial plateau at or near the semimembranosus tendon insertion.
(See the images below.)
 Contrecoup medial bone bruise of the tibia in a patient with an ACL tear. High-signal bone bruise in the posteromedial aspect of the tibial plateau (arrow). This is a common finding in patients with ACL tears with pivot-shift/twisting mechanisms. This bone bruise is a marker for a pronounced twisting injury. As such, nearby medial meniscal tears are exceptionally frequent. (Even when no meniscal tears are seen, occult medial meniscal-meniscocapsular junction tears are not uncommonly present.)
Contrecoup medial bone bruise of the tibia in a patient with an ACL tear. High-signal bone bruise in the posteromedial aspect of the tibial plateau (arrow). This is a common finding in patients with ACL tears with pivot-shift/twisting mechanisms. This bone bruise is a marker for a pronounced twisting injury. As such, nearby medial meniscal tears are exceptionally frequent. (Even when no meniscal tears are seen, occult medial meniscal-meniscocapsular junction tears are not uncommonly present.)
 Severe medial contrecoup bone bruise of the posteromedial tibia with associated impaction fracture. Patient is a 26-year-old man with an arthroscopically proven ACL tear.
Severe medial contrecoup bone bruise of the posteromedial tibia with associated impaction fracture. Patient is a 26-year-old man with an arthroscopically proven ACL tear.
Bone bruises were originally reported to persist on MRIs for about 6 weeks. [90] It is now clear, however, that bone bruises commonly remain visible on MRI studies 12-14 weeks after injury.
It is surmised that MRI-diagnosed bone bruises probably have prognostic significance by indicating an increased probability of underlying articular chondral injury and subsequent joint degeneration. [35, 100]
Anterior translocation of the tibia
Anterior translocation of the tibia is the MRI correlate to anterior drawer instability elicited on physical examination and, as such, indirectly suggests ACL incompetency. The radiologist should seek this finding on sagittal images through the middle of the lateral femoral condyle. If the tibia translocates anteriorly to the extent that the distance between vertical tangent lines through the posterior margins of the femur and tibia laterally exceeds 5 mm, acute or chronic ACL tear is likely. [88, 96] Milder degrees of anterior translocation are unreliable.
(See the image below.)
 Anterior translation of tibia as a secondary sign of an ACL tear. Sagittal T1-weighted image in a patient with an arthroscopically proven ACL tear shows mild anterior translation of the tibia. As a result, a tangent line to the posterior margin of the tibia passes through the posterior horn lateral meniscus (uncovered meniscus sign). In normal knees, this line passes posterior to the meniscus. This sign should be sought on an image through the midportion of the lateral femoral condyle. Both chronic and acute ACL tears often demonstrate anterior translation of the tibia.
Anterior translation of tibia as a secondary sign of an ACL tear. Sagittal T1-weighted image in a patient with an arthroscopically proven ACL tear shows mild anterior translation of the tibia. As a result, a tangent line to the posterior margin of the tibia passes through the posterior horn lateral meniscus (uncovered meniscus sign). In normal knees, this line passes posterior to the meniscus. This sign should be sought on an image through the midportion of the lateral femoral condyle. Both chronic and acute ACL tears often demonstrate anterior translation of the tibia.
Abnormal tibial translocation is also suspected if a vertical line tangent to the posterior cortex of the tibial plateau courses through, or anterior to, the posterior horn meniscus (the "uncovered meniscus sign").
An unusually vertically oriented lateral collateral ligament (LCL), seen in its entirety on a single slice, is essentially another manifestation of anterior drawer displacement of the lateral tibia. The normal LCL is tilted off the coronal plane and thus requires review of multiple consecutive coronal images to visualize the ligament from origin to insertion. As a corollary of this, a verticalized single-slice LCL is a soft secondary sign of ACL compromise. [101]
(See the image below.)
 Vertically oriented lateral collateral ligament (LCL) as a secondary sign of anterior cruciate ligament (ACL) injury. The entire fibular collateral ligament is visualized on a single coronal image. This ligament is ordinarily oblique to the coronal plane but is verticalized in the setting of ACL tear-related anterior tibial translocation.
Vertically oriented lateral collateral ligament (LCL) as a secondary sign of anterior cruciate ligament (ACL) injury. The entire fibular collateral ligament is visualized on a single coronal image. This ligament is ordinarily oblique to the coronal plane but is verticalized in the setting of ACL tear-related anterior tibial translocation.
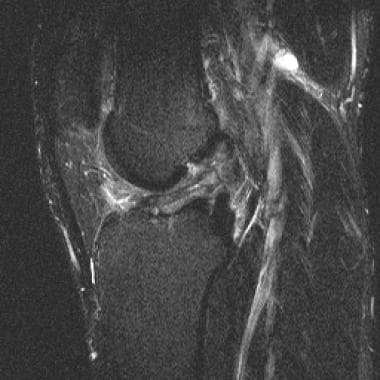
Segond fracture: high association with ACL injury
A Segond fracture (see the images below) is a stereotypical fracture of the tibia that has a 75-100% association with ACL tear. [38] The Segond fracture is an elliptical, vertical, 3 X 10-mm bone fragment paralleling the lateral tibial cortex about 4 mm distal to the plateau. Segond fractures have historically been attributed to traction avulsion of the middle third of the meniscotibial capsular ligament; slips of the iliotibial band and lateral collateral ligament complex have been implicated. [102]
 Segond fracture in a patient with an ACL tear. T1 coronal image demonstrates stereotypical elongate fracture fragment along the proximal and lateral margin of the tibia (arrow). This fracture has a very high statistical association with ACL tear. (Torn ACL is visualized in intercondylar notch.)
Segond fracture in a patient with an ACL tear. T1 coronal image demonstrates stereotypical elongate fracture fragment along the proximal and lateral margin of the tibia (arrow). This fracture has a very high statistical association with ACL tear. (Torn ACL is visualized in intercondylar notch.)
 Segond fracture in a patient with an ACL tear. Fat-saturated proton-weighted fast spin echo image shows stereotypical elongate tibial fracture fragment (arrow). (Retracted, discontinuous ACL fibers are visible in the intercondylar notch.)
Segond fracture in a patient with an ACL tear. Fat-saturated proton-weighted fast spin echo image shows stereotypical elongate tibial fracture fragment (arrow). (Retracted, discontinuous ACL fibers are visible in the intercondylar notch.)
 Segond fracture. Anteroposterior (AP) knee radiograph shows a linear fracture fragment that parallels the proximal lateral surface of the tibia (arrow). The probability of an ACL tear is very high in patients with a Segond fracture.
Segond fracture. Anteroposterior (AP) knee radiograph shows a linear fracture fragment that parallels the proximal lateral surface of the tibia (arrow). The probability of an ACL tear is very high in patients with a Segond fracture.
On MRIs, the Segond fracture fragment is often inconspicuous and easily overlooked. In fact, the MRI reader is often tipped off instead by an associated focal marrow edema-like signal focus of the adjacent lateral tibial plateau. The Segond fragment demonstrates a marrow-edema high T2-signal appearance in the acute setting; in the long term, it usually shows isointensity relative to marrow (or low signal related to osseous sclerosis) and may fuse to the underlying bone. [38, 103]
On plain films, a Segond fracture must be distinguished from a Gerdy tubercle bony avulsion anterolaterally (with iliotibial band traction); this fracture is optimally seen on a radiograph with external rotation. In contrast, a Segond fracture is best seen on a true anteroposterior radiograph (and is also readily shown on a tunnel view). [38, 104]
Fracture of the tibial spine: less reliably associated with ACL tear
The ACL does not actually insert on the anterior tibial spine; it inserts immediately lateral and anterior to it. Thus, tibial spine fractures can be seen in patients with a normal competent ACL; nevertheless, the possibility of an ACL tear (or ACL insufficiency) should be borne in mind when these fractures are detected. Tibial spine avulsion with ACL insufficiency or injury indicates a hyperextension mechanism in most cases. While relatively more common in the pediatric population, the majority of ACL tears in children are not associated with a tibial osseous avulsion. Only 5% of adults with traumatic ACL insufficiency have an associated tibial avulsion. Tibial spine fractures are often isolated in children, but they imply a high-force injury in adults, and other internal derangements are usually present. [39, 105, 106, 107]
(See the images below.)
 Anterior cruciate ligament (ACL) insufficiency secondary to distal tibial bony avulsion. An avulsion fracture (arrow) is seen at the expected region of the distal insertion of the ACL near the tibial spines. This finding should suggest the possibility of ACL insufficiency/injury because the ACL inserts just lateral to the tibial spine. This is often an isolated injury (with or without ACL compromise) in children. In adults, however, such fractures imply great force; the fractures are often more extensive than expected and are usually accompanied by other internal derangements.
Anterior cruciate ligament (ACL) insufficiency secondary to distal tibial bony avulsion. An avulsion fracture (arrow) is seen at the expected region of the distal insertion of the ACL near the tibial spines. This finding should suggest the possibility of ACL insufficiency/injury because the ACL inserts just lateral to the tibial spine. This is often an isolated injury (with or without ACL compromise) in children. In adults, however, such fractures imply great force; the fractures are often more extensive than expected and are usually accompanied by other internal derangements.
 ACL insufficiency in a pediatric patient secondary to tibial avulsion fracture. Sagittal T2-weighted MRI shows a minimally displaced fracture of the tibia at the insertion of the ACL (arrow). Such avulsions are more common in children than in adults.
ACL insufficiency in a pediatric patient secondary to tibial avulsion fracture. Sagittal T2-weighted MRI shows a minimally displaced fracture of the tibia at the insertion of the ACL (arrow). Such avulsions are more common in children than in adults.
On MRI, tibial spine fracture fragments may be small and difficult to appreciate. The MRI reader must be alert for their presence, especially in MRI examinations in children.
(See the image below.)
 Osseous avulsion of the anterior cruciate ligament (ACL) insertion. Gradient echo sagittal image demonstrates a displaced tibial fracture fragment at the distal ACL insertion. The MRI reader must be vigilant as these fractures are often subtle and easily missed. In indeterminate cases, plain films or CT may be beneficial.
Osseous avulsion of the anterior cruciate ligament (ACL) insertion. Gradient echo sagittal image demonstrates a displaced tibial fracture fragment at the distal ACL insertion. The MRI reader must be vigilant as these fractures are often subtle and easily missed. In indeterminate cases, plain films or CT may be beneficial.
Several tibial spine fracture classification systems have been proposed. [108] Treatment is somewhat controversial; however, surgery is often performed in the setting of displaced larger fractures.
Summary of fractures commonly associated with ACL injury
The image interpreter should be alert for 5 fractures that are statistically associated with ACL injuries. Two of these fractures have a very high association with ACL tear: the Segond fracture and the deep-lateral femoral-notch sign fracture. Three other fractures have an intermediate probability of ACL injury: tibial spine avulsion fracture, fracture of the posterolateral corner of the tibia, and arcuate fibular head fracture. The MRI reader should be especially careful to search for a subtle Segond fracture (or adjacent associated focal marrow edema focus of the tibia) and tibial spine avulsions. These findings may be helpful in the setting of equivocal primary MRI signs of ACL injury. [97] CT correlation may be helpful in difficult cases.
Other secondary signs of ACL tear
Kissing anterior femoral and tibial bone bruises suggest a hyperextension injury. [109] Similarly, avulsion fractures of the proximal fibula (termed the arcuate sign) predict a possible hyperextension/varus injury. The LCL complex is usually torn, and the ACL was torn in 13 of 18 patients in one study. [110] Posterior cruciate ligament (PCL) tears are also often present in these hyperextension injuries. In severe cases, the knee frankly dislocates, and popliteal neurovascular injuries should be sought on images. [111]
(See the images below.)
 Hyperextension anterior "kissing" bone bruises as a secondary sign of anterior cruciate ligament (ACL) tear. Sagittal T2-weighted image in 52-year-old woman. This pattern of bone bruises is reported to be associated with ACL tear in about 50% of patients. Patient had clinical history of subluxation and other images showed posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and medial collateral ligament (MCL) injuries.
Hyperextension anterior "kissing" bone bruises as a secondary sign of anterior cruciate ligament (ACL) tear. Sagittal T2-weighted image in 52-year-old woman. This pattern of bone bruises is reported to be associated with ACL tear in about 50% of patients. Patient had clinical history of subluxation and other images showed posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and medial collateral ligament (MCL) injuries.
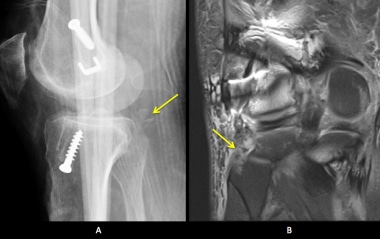 Arcuate fracture of the fibular head as a secondary sign of possible anterior cruciate ligament (ACL) (and lateral collateral ligament [LCL]/posterior cruciate ligament [PCL]) injury. Forty-year-old man with a history of knee dislocation. A. Lateral radiograph shows several fibular head avulsion fracture fragments. B. Coronal T2-weighted MRI shows several subtle fibular head low-signal fracture fragments (arrow) and associated marrow edema of the fibular head. The LCL is absent/torn. The PCL and ACL were also torn. A fibular head avulsion fracture is suggestive (although not diagnostic) of a hyperextension/varus injury, which, in turn, may cause a combination of PCL, LCL, and ACL injuries.
Arcuate fracture of the fibular head as a secondary sign of possible anterior cruciate ligament (ACL) (and lateral collateral ligament [LCL]/posterior cruciate ligament [PCL]) injury. Forty-year-old man with a history of knee dislocation. A. Lateral radiograph shows several fibular head avulsion fracture fragments. B. Coronal T2-weighted MRI shows several subtle fibular head low-signal fracture fragments (arrow) and associated marrow edema of the fibular head. The LCL is absent/torn. The PCL and ACL were also torn. A fibular head avulsion fracture is suggestive (although not diagnostic) of a hyperextension/varus injury, which, in turn, may cause a combination of PCL, LCL, and ACL injuries.
An arched redundant-appearing PCL is one of the least useful secondary signs of ACL injury. While this occurs commonly in ACL injuries with anterior translation of the tibia, similar appearances occur with hyperextended normal knees and with quadriceps dysfunction. [39, 90, 112]
(See the image below.)
 Posterior cruciate ligament (PCL) redundancy as a secondary sign of an anterior cruciate ligament (ACL) tear. T1-weighted sagittal MRI shows an unusually arched PCL (arrow). This is a relatively unreliable secondary sign of ACL tear. Many patients with this finding do not have an ACL tear and some patients with an ACL tear do not demonstrate a redundant PCL. However, this patient did have an arthroscopically proven ACL tear.
Posterior cruciate ligament (PCL) redundancy as a secondary sign of an anterior cruciate ligament (ACL) tear. T1-weighted sagittal MRI shows an unusually arched PCL (arrow). This is a relatively unreliable secondary sign of ACL tear. Many patients with this finding do not have an ACL tear and some patients with an ACL tear do not demonstrate a redundant PCL. However, this patient did have an arthroscopically proven ACL tear.
Cadaver studies have shown no normal synovial recesses in the triangular space inferior to the intersecting ACL and PCL as observed on sagittal images. Therefore, Lee et al hypothesized that fluid in this location may indirectly indicate abnormality of the cruciate ligaments, but this has not been confirmed in a clinical setting. [113] As noted, fluid-filled synovial recesses anterior and posterior to the ACL are a common finding in normal ACLs. Edema in the region of the ACL is an abnormal but nonspecific finding [95] ; other evidence is needed to make a definitive diagnosis of tear.
Partial ACL tear
Partial tears of the ACL are common, accounting for 10-43% of all ACL tears [24, 30, 57, 114] and accounting for a higher percentage of ACL tears in the pediatric population. [115] The natural history and optimal treatment of these injuries is still being worked out. [30, 116] A tear involving less than 25% of the ACL arthroscopically has a favorable prognosis; a tear involving 0.5-0.75 of the ACL has a high probability of progressing to a complete tear. [30, 114, 116, 117] Overall, less than 50% of patients with an unoperated partial tear are able to return to their preinjury level of activity. [118]
On physical examination, partial tears often present with a normal or indeterminate Lachman test. [30, 119] In cadavers, laxity is absent on physical examination and arthrometric testing when only the anteromedial band of the ACL is transected.
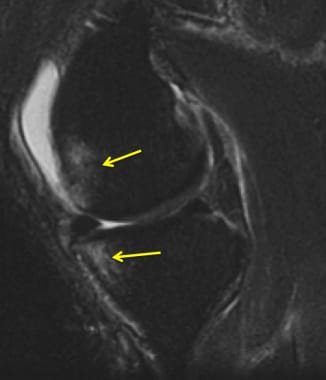
(See the images below.)
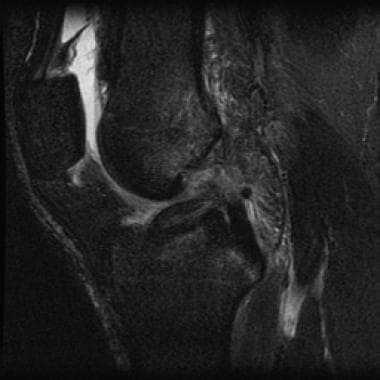
 Partial ACL tear. T2 sagittal image shows attenuated appearance of ACL and question of subtle flattening of the axis of the ACL.
Partial ACL tear. T2 sagittal image shows attenuated appearance of ACL and question of subtle flattening of the axis of the ACL.
 (Same patient as in the previous image.) Partial tear of the anterior cruciate ligament (ACL). Axial image showing poorly visualized, high-signal, fragmented ACL.
(Same patient as in the previous image.) Partial tear of the anterior cruciate ligament (ACL). Axial image showing poorly visualized, high-signal, fragmented ACL.
 (Same patient as in the previous image.) Partial ACL tear. Sagittal T2-weighted image shows typical ACL-tear related pivot-shift bone bruises of the lateral femoral condyle and the posterolateral tibia. Patient had a normal Lachman test. These images demonstrate that secondary signs of ACL tear (eg, pivot-shift bone bruises) can occur with partial ACL tears and that high-grade partial tears are difficult to distinguish from complete tears.
(Same patient as in the previous image.) Partial ACL tear. Sagittal T2-weighted image shows typical ACL-tear related pivot-shift bone bruises of the lateral femoral condyle and the posterolateral tibia. Patient had a normal Lachman test. These images demonstrate that secondary signs of ACL tear (eg, pivot-shift bone bruises) can occur with partial ACL tears and that high-grade partial tears are difficult to distinguish from complete tears.
 Partial ACL tear (arthroscopically proven). Images show unusually attenuated appearing ACL surrounded by increased high-signal edema/hemorrhage. With subtle/equivocal primary signs of ACL injury, one must look for other secondary signs of ACL injury and correlate with clinical history/Lachman test findings. One could also consider problem-solving additional MRI sequences.
Partial ACL tear (arthroscopically proven). Images show unusually attenuated appearing ACL surrounded by increased high-signal edema/hemorrhage. With subtle/equivocal primary signs of ACL injury, one must look for other secondary signs of ACL injury and correlate with clinical history/Lachman test findings. One could also consider problem-solving additional MRI sequences.
 Partial tear of the ACL. T1-weighted sagittal MRI image shows disrupted ACL fibers proximally compatible with an ACL tear.
Partial tear of the ACL. T1-weighted sagittal MRI image shows disrupted ACL fibers proximally compatible with an ACL tear.
 (Same patient as in previous image.) Partial tear of the ACL. T1-weighted sagittal MRI slice, immediately adjacent to the previous image, shows a normal-appearing ACL. Arthroscopy confirmed a partial tear of the ACL. Partial ACL tears may be suggested in the proper clinical setting when primary signs of ACL tear are present, but at least one slice shows a normal, taut-appearing ACL.
(Same patient as in previous image.) Partial tear of the ACL. T1-weighted sagittal MRI slice, immediately adjacent to the previous image, shows a normal-appearing ACL. Arthroscopy confirmed a partial tear of the ACL. Partial ACL tears may be suggested in the proper clinical setting when primary signs of ACL tear are present, but at least one slice shows a normal, taut-appearing ACL.
 Partial tear versus mucinous degeneration of the anterior cruciate ligament (ACL) (unproven case). T2-weighted sagittal image. Patient presented with pain and no history of significant trauma. The ACL is enlarged with non-fluid-like increased signal separating intact-appearing straight ACL fibrils. The differential diagnosis for this appearance includes mucinous degeneration (not uncommon) and a delaminating partial tear. Detailed history and Lachman test is necessary to differentiate.
Partial tear versus mucinous degeneration of the anterior cruciate ligament (ACL) (unproven case). T2-weighted sagittal image. Patient presented with pain and no history of significant trauma. The ACL is enlarged with non-fluid-like increased signal separating intact-appearing straight ACL fibrils. The differential diagnosis for this appearance includes mucinous degeneration (not uncommon) and a delaminating partial tear. Detailed history and Lachman test is necessary to differentiate.
While MRI is accurate in differentiating the normal from abnormal ACL, it is less reliable in the diagnosis of partial tears. [90, 116, 120]
Van Dyck et al listed 4 principal presentations of ACL partial tears on MRI images [121] :
-
First, partial tears often resemble a complete tear in all respects on MRI images. [116] Overestimation of tear severity in this setting fortunately should have little effect on outcomes, since most of these higher-grade tears are thought to progress to full tear if the patient returns to previous activity. It should be re-emphasized that secondary signs of ACL tear (eg, pivot-shift bone bruises) are common to both complete and the more pronounced partial tears and therefore cannot striclty differentiate partial from complete tears. [93, 83]
-
Second, partial-tear ACL appearances may resemble mucinous degeneration. The ligament is enlarged with straight, intact-appearing fibrils separated by intermediate-high signal. This represents a delaminating form of injury, less severe than transverse tears; thus, patients may be functional on clinical testing.
-
Third, the partial tear may appear normal on MRI images. Knowing this, the possibility of an MRI-occult partial tear must be considered in the setting of a suggestive injury mechanism when there is laxity on clinical/ arthrometic testing or there are indirect signs of ACL injury on the MRI (such as pivot-shift bone bruises or anterior tibial translation).
-
Fourth, partial tears may present as an isolated bundle tear. However several studies have shown that isolated bundle tears account for only a small percentage of tears that go to arthroscopy. [83, 122] This helps explain why 3-Tesla imaging, despite improved visualization of bundle anatomy, continues to demonstrate limiited overall accuracy in diagnosing partial tears. [79, 121, 83, 122] One may suggest a partial tear even when bundle anatomy is not distinct, when there appears to be partial-thickness abnormal increased signal thinning of the normal tendon, or when there are primary signs of a tear on one slice while an adjacent section shows a normal taut ACL. [116, 3, 123] Clearly, however, such findings have limited specificity for tear. This is due to multiple confounding factors, including intraligamentous degenerative increased signal and partial volume artifacts.
A partially or completely torn ACL may form a stump that angles anteriorly into the anterior intercondylar notch region (the so called "bell-hammer sign" or "preoperative cyclops syndrome"). [85, 86] Lefevre et al have pointed out that while this is a an uncommon tear presentation, it may serve as a tipoff that a partial tear is present in problem diagnostic settings. This sign manifests as either (1) an anteriorly angled ACL stump or (2) a heterogeneous variable-signal nodule projecting anteriorly from the ACL. Histologic evaluation of the nodules has revealed disorganized ACL fibers, fibrosis, inflammation, and hemorrhage, mirroring the histology of post-graft cyclops lesions; as in post-graft patients with arthrofibrosis, these patients usually have restricted extension range of motion.
It is clear that MRI adds some value in the evaluation and management of partial tears, and positive MRI findings should not be ignored, even in the setting of a negative Lachman test. In most cases, the MRI reader should at least be able to classify MRI findings into either a complete versus high-grade tear category (high risk) or a normal versus low-grade tear category (lower risk). [57, 58, 74, 3, 124] Additional problem-solving oblique coronal sequences, [62] isotropic voxel imaging, or flexed-position MRI sequences may be helpful.
Treatment recommendations for patients with partial ACL tears are evolving. Factors favoring conservative treatment include advanced age, a normal or near-normal Lachman result, low athletic demands, and less than 50% involvement of the ACL fibers on arthroscopy. Most young and highly active patients, patients with a clearly abnormal Lachman result, and patients with greater than 50% or posterolateral band involvement on arthroscopy are best treated with ACL reconstruction. [4]
Chronic ACL Tears and Miscellaneous Conditions
Chronic ACL tear
The MRI reader not uncommonly encounters nonacute anterior cruciate ligament (ACL) tears. These injuries are often associated with meniscal tears and secondary osteoarthritis.
MRI signs of chronic ACL tear are similar to those of acute ACL injury, except that bone bruises and edema around the knee are no longer visible as clues for the image reader that a tear is present. [95, 125] In addition, there are several appearances unique to the chronic phase; for example, there may be an "empty notch" sign with an absent ACL and a pristine fat signal evident in the lateral intercondylar notch. [54]
(See the images below.)
 Chronic anterior cruciate ligament (ACL) tear. T1-weighted image of 64-year-old man demonstrating abnormal flattening of the ACL axis relative to the intercondylar roof. Acute phase edema in the intercondylar notch has resolved, with the ACL again surrounded by normal fat signal.
Chronic anterior cruciate ligament (ACL) tear. T1-weighted image of 64-year-old man demonstrating abnormal flattening of the ACL axis relative to the intercondylar roof. Acute phase edema in the intercondylar notch has resolved, with the ACL again surrounded by normal fat signal.
 Chronic tear of the ACL with empty notch sign. T1-weighted coronal MRI shows only fat in the lateral intercondylar notch; the ACL is absent. A normal posterior cruciate ligament (PCL) is present in the medial aspect of the notch (arrow). This is a frequent MRI appearance of a chronic ACL tear after the resolution of acute edema and hemorrhage.
Chronic tear of the ACL with empty notch sign. T1-weighted coronal MRI shows only fat in the lateral intercondylar notch; the ACL is absent. A normal posterior cruciate ligament (PCL) is present in the medial aspect of the notch (arrow). This is a frequent MRI appearance of a chronic ACL tear after the resolution of acute edema and hemorrhage.
 Chronic tear of the ACL with proximal, focal hyperintense disruption. Sagittal T2-weighted fast spin-echo MRI shows focal fluid-intensity interruption of the proximal ACL (arrow). Absence of surrounding edemalike signal intensity is consistent with the chronic nature of the tear, as confirmed by history and subsequent endoscopy.
Chronic tear of the ACL with proximal, focal hyperintense disruption. Sagittal T2-weighted fast spin-echo MRI shows focal fluid-intensity interruption of the proximal ACL (arrow). Absence of surrounding edemalike signal intensity is consistent with the chronic nature of the tear, as confirmed by history and subsequent endoscopy.
 Chronic tear of the ACL, false-negative result on MRI. The radiologist interpreted this sagittal T2-weighted fast spin-echo fat-saturated MRI, and other images, as normal. In retrospect, the axis of the ACL is abnormally horizontal relative to the roof of the intercondylar notch. Arthroscopy revealed a chronically and grossly insufficient ACL with a few fibers inserting on posterior cruciate ligament (PCL). A chronically torn ACL, with low-signal fibrous healing, can appear misleadingly normal on MRI.
Chronic tear of the ACL, false-negative result on MRI. The radiologist interpreted this sagittal T2-weighted fast spin-echo fat-saturated MRI, and other images, as normal. In retrospect, the axis of the ACL is abnormally horizontal relative to the roof of the intercondylar notch. Arthroscopy revealed a chronically and grossly insufficient ACL with a few fibers inserting on posterior cruciate ligament (PCL). A chronically torn ACL, with low-signal fibrous healing, can appear misleadingly normal on MRI.
 Chronic tear of the ACL, with false-negative MRI report. The proximal ACL appears slightly attenuated; however, in the absence of other primary or secondary signs of tear, this appearance lacks specificity for an ACL tear. Images in other planes appeared normal in this patient; however, endoscopy revealed a chronic incompetent ACL. This case again demonstrates that chronic ACL tears may present a challenge to the MR-reader.
Chronic tear of the ACL, with false-negative MRI report. The proximal ACL appears slightly attenuated; however, in the absence of other primary or secondary signs of tear, this appearance lacks specificity for an ACL tear. Images in other planes appeared normal in this patient; however, endoscopy revealed a chronic incompetent ACL. This case again demonstrates that chronic ACL tears may present a challenge to the MR-reader.
Secondly, a chronically torn ACL stump may angle anteriorly and enlarge into a nodule: the "pseudo-cyclops" appearance. Thirdly, the torn stump may flop posteriorly and attach to the posterior cruciate ligament (PCL). [39] The authors, however, have noted that the PCL attachment is most often an endoscopic observation and is less frequently appreciated on MRI, even in retrospect. These patients may have a clinical endpoint of anterior translation of the tibia with Lachman testing, resulting in a false-negative clinical examination.
The chronic nondisplaced ACL tear unfortunately may appear entirely normal, presumably because hypointense mature collagenous scarring cannot be distinguished from normal collagenous hypointense ligament. [95, 5] The MRI reader must be especially diligent in the nonacute injury setting to avoid underdiagnosis. T1 sequences are more frequently informative in these patients and should be inspected diligently. Problem-solving additional MRI sequences or clinical correlation may be pivotal in diagnosis.
Mucoid degeneration and ganglion cysts of the ACL
Mucoid degeneration of the ACL can mimic a delaminating ACL tear. [126, 127] The etiology of this entity is uncertain, but it may lie along a continuum of senescent degeneration of the ligament. [127] It is increasingly evident to this author and others that mucoid degeneration of the ACL is a fairly common entity. [128]
Patients are usually older than 30 years. They may be asymptomatic, but they frequently have pain and limited flexion of the knee. The knee is stable, with a negative Lachman test result.
(See the image below.)
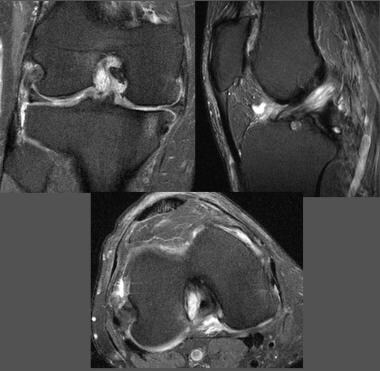 Suspected mucoid degeneration or intraligamentous ganglion cyst of the anterior cruciate ligament (ACL). Patient had no history of trauma and no instability on physical examination. High-signal focal enlargement of the proximal ACL is noted. The proximal splaying apart of fibers with "celery-stalk" appearance suggests mucoid degeneration; however, involvement of only the proximal ACL is more typical of intraligamentous ganglion cyst. Before diagnosing either of these entities, secondary MR signs of ACL tear should be excluded and the patient should be confirmed as having a negative Lachman test result.
Suspected mucoid degeneration or intraligamentous ganglion cyst of the anterior cruciate ligament (ACL). Patient had no history of trauma and no instability on physical examination. High-signal focal enlargement of the proximal ACL is noted. The proximal splaying apart of fibers with "celery-stalk" appearance suggests mucoid degeneration; however, involvement of only the proximal ACL is more typical of intraligamentous ganglion cyst. Before diagnosing either of these entities, secondary MR signs of ACL tear should be excluded and the patient should be confirmed as having a negative Lachman test result.
On arthroscopy, the ACL is enlarged and often impinges on the intercondylar notch sidewalls or roof. Histologic examination of the ligament demonstrates extensive, patchy, yellow, internal deposits, which represent a mixture of fibrous elements and mucoid degeneration.
Treatment has consisted of mainly meticulous piece-by-piece debulking of the yellowish material. Some fascicles of the ACL may be sacrificed in this procedure. Notchplasty may also be performed to reduce ACL-notch impingement.
MRI appearances are characteristic. The ACL is enlarged with diffusely increased non–fluid-like increased signal internally that splays apart intact ACL fascicles. The splayed linear ACL fascicles have a "celery-stalk" appearance. As noted, the reader must also consider a delaminating tear with this appearance. A nontraumatic history, a negative Lachman test, and a lack of secondary signs of an ACL tear should suggest the correct diagnosis. [39, 126, 127, 129, 130, 131]
Intraligamentous and extraligamentous ganglion cysts of the ACL are a related but distinct entity. The extraligamentous cysts are extremely common but do not present a diagnostic problem. These appear as well-defined, lobular, often septated cysts immediately adjacent to the ACL. These cysts are usually asymptomatic incidental findings, although a variety of symptoms have been reported. The smaller cysts may be difficult to differentiate from normal synovial recesses. [129]
Ganglion cysts in the substance of the ACL are less common but have been reported in all age groups. [132, 133, 134, 135, 136]
On MRI, ganglion cysts appear as fusiform, well-defined cysts oriented along the long axis of the substance of an otherwise normal-appearing ACL. When the cysts are small, this appearance may be mistaken for that of a partial ACL tear, [133] but differentiation is usually not difficult.
(See the image below.)
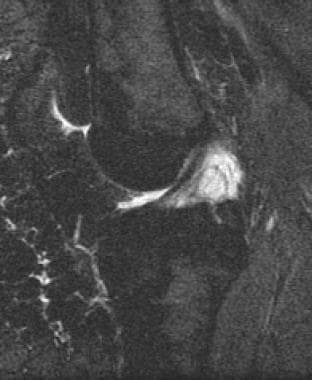 Ganglion cyst of the intercondylar notch (unproven). Cystic focal signal abnormality immediately posterior to the proximal aspect of the ACL. The fibers of the ACL proper appeared to be uninvolved on all sequences. Fluid-signal ganglion cysts (vs synovial cysts or joint recesses) are extremely commonly visualized in the pericruciate regions on MR scans of the knee.
Ganglion cyst of the intercondylar notch (unproven). Cystic focal signal abnormality immediately posterior to the proximal aspect of the ACL. The fibers of the ACL proper appeared to be uninvolved on all sequences. Fluid-signal ganglion cysts (vs synovial cysts or joint recesses) are extremely commonly visualized in the pericruciate regions on MR scans of the knee.
Several authors have described ACL ganglion cysts that developed in young patients after trauma. [132, 137] As in diffuse mucoid degeneration of the ACL, the knee is stable with a negative Lachman result. However, symptoms may be clinically significant, and patients often benefit from arthroscopic probing with release of the mucinous material, with or without partial debridement. [38, 129]
Ganglion cysts of the ACL can be difficult to appreciate on standard arthroscopy. Therefore, diagnosis may depend on MRI; the MRI reader who recognizes the abnormality may alert the arthroscopist to probe the ACL or add a posterior portal approach. [127, 129, 130]
Congenital abnormalities
The ACL may be congenitally absent or hypoplastic. This usually occurs in association with intercondylar notch osseous stenosis and/or local or distant bone dysplasias, but it is rarely an isolated finding. Most patients are asymptomatic (despite physical exam laxity) until an injury disturbs knee homeostasis. [138] [139]
Calpur et al reported 2 patients with a markedly widened deltoid (triangular) distal ACL at the tibial insertion. [140] Symptomatic impingement of the intercondylar-notch structures was reported, and successful trimming of the distal ACL (ligamentoplasty) was performed in both patients.
Summary
One must become familiar with normal and abnormal appearances of the ACL in all planes. On sagittal images, the MRI reader should critically evaluate the ACL axis relative to the intercondylar roof. The proximal and distal aspects of the ACL should also be carefully evaluated, as tears or osseous avulsions may be readily overlooked in these locations. Axial sequences are especially useful in evaluating the proximal ACL. One should be alert for the secondary signs of ACL tear, including the often-subtle MRI findings of Segond fractures.
One should be aware of the lower accuracy of MRI for partial tears. Interstitial tears may rarely present with an appearance similar to mucinous degeneration of the ACL. Anteriorly angled ACL fibers, the "bell-hammer" or pseudo-cyclops appearance, may uncommonly be the only tipoff of a partial tear (or chronic tear). Chronic ACL tears are also apt to be missed. Subtle flattening of the ACL axis or slight angulation of the ligament may be the only sign of a chronic tear. Chronic tears may also present with an "empty notch sign."
Regarding generation of images, it is recommended that sagittal images be obtained in the true orthogonal plane, rather than performing obliqued imaging. In equivocal tear cases, one may perform an additional problem-solving sequence. Often helpful is the oblique coronal sequence prescribed along the long axis of the ligament on a sagittal image. Flexed-knee sagittal imaging may show the proximal ligament to advantage.
Finally, satisfaction-of-search errors should be avoided. When the ACL is torn, the interpreter should look diligently for other internal derangements, especially peripheral meniscal tears and lateral collateral ligament (LCL) injuries.
-
Kissing anterior bone bruises indicative of hyperextension mechanism in a patient with an ACL tear (ACL not shown). Sagittal T1-weighted MRI shows apposing ill-defined hypointense bone contusions of the anterior femur and adjacent tibial plateau. T2-weighted imaging is more sensitive than T1-weighted imaging for detecting acute bone bruises. A small, linear incomplete subchondral fracture is superimposed on the tibial bone bruise.
-
Posterior cruciate ligament (PCL) tear in a patient with a hyperextension-dislocation injury and an anterior cruciate ligament (ACL) tear. Sagittal T1-weighted MRI shows focally enlarged, hypointense torn PCL (arrow).
-
(Same patient as in previous image.) Acute hyperextension-dislocation tear of the ACL. Sagittal T1-weighted image shows ill-defined edema/hemorrhage in the intercondylar notch in the usual location of the ACL; no normal ACL fibers are identified. This is a common appearance of an acute ACL tear on MRI images. Some combination of ACL, posterior cruciate ligament, and lateral collateral ligament tears are often present with hyperextension-dislocation injuries of the knee.
-
(Same patient as in previous image.) Fibular collateral ligament tear in a patient with a hyperextension-dislocation injury. Coronal T1-weighted MRI shows a torn, displaced fibular collateral ligament (FCL) (arrow). The fibular collateral ligament is a major component of the lateral collateral ligament complex. Some combination of lateral collateral ligament, anterior cruciate ligament, and posterior cruciate ligament tears are often present in patients with hyperextension injuries to the knee.
-
Prescribing sagittal images. Images are prescribed on a scout axial image off a line tangent to the femoral condyle posterior margins (the bicondylar line). Most centers now generate images perpendicular to the bicondylar line. Slightly oblique images may be obtained but should be no more than 10 degrees off perpendicular. Prescribing images along the axial plane long axis of the ACL is discouraged; this will usually lead to overly oblique sagittal images with degraded visualization of the menisci and other knee structures.
-
Example of prescribed sagittal images on axial scout image. In this case, images were obtained oblique to a line perpendicular to the bicondylar line. Care should be taken to avoid over-obliquity of sagittal images.
-
Anterior cruciate ligament (ACL) anatomy in the sagittal plane. Sagittal T1-weighted image. The ACL arises from the posterior aspect of the medial surface of the lateral femoral condyle, high in the intercondylar notch. It courses obliquely anterior, bands diverging distally, to insert on the tibia well posterior to the anterior margin. The ligament is low signal in nature due to its collagenous nature, but higher signal than the posterior cruciate ligament (PCL).
-
ACL anatomy in the coronal plane. Coronal T1-weighted MRI shows the lateral position of the ACL in the intercondylar notch (arrow), surrounded by high-signal fat. Note the slanted course of the ligament. The ACL bundles diverge distally at their tibial insertion medial to the anterior intercondylar eminence.
-
Anterior cruciate ligament (ACL) anatomy in the axial plane. A fat-saturated neutral-weighted MRI shows the collagenous low-signal ACL positioned in the lateral aspect of the intercondylar notch (arrow). Distally (not shown) the ACL moves away from the wall and diverges into a horseshoe-array of multiple fascicles.
-
Partial-volume inclusion of the lateral femoral condyle causing a false appearance of an ACL tear. T1-weighted sagittal MRI shows an ill-defined pseudomass about the proximal ACL that could be taken as evidence for ACL injury. With evaluation of adjacent images and other imaging planes, this should not cause problems in interpretation.
-
Nonvisualization as a primary sign of ACL tear. Complete (or near-complete) nonvisualization of the ACL on sagittal images with ill-defined edema and hemorrhage in the usual location of the ACL is a very common presentation of an acute tear. Note: the normal ACL is sometimes poorly seen on low–echo-time (T1 or gradient echo) sagittal images; this usually does not present a problem in interpretation if T2 images, and images in other planes are carefully correlated.
-
Nonvisualization of the ACL as a primary sign of a tear in a T2-weighted sequence. Sagittal T2-weighted fat-saturated fast spin-echo (FSE) image shows replacement of the ACL in the intercondylar notch by extensive edema-fluid signal intensity.
-
Focal interruption as a primary sign of anterior cruciate ligament (ACL) tear. T2-weighted image shows focal hyperintense edema and/or fluid involving the proximal ACL.
-
Primary signs of an ACL tear. Sagittal image (top left) demonstrates high-signal disruption of the ACL with multifragmented appearance. Coronal T2 (top right) and T1 (below) images show nonvisualization of ACL fibers and abnormal increased edema and fluid in the lateral intercondylar notch.
-
Angulation/nonlinearity as a primary sign of anterior cruciate ligament (ACL) tear. T1-weighted sagittal MRI shows an abruptly angulated mid ACL (arrow). The normal ACL occasionally has a gently curved, convex-inferior appearance, but a wavy or sharply angulated appearance is abnormal.
-
Abnormal flat axis of the ACL as a primary sign of an ACL tear. T1-weighted sagittal image shows markedly flattened axis of the distal ACL relative to the intercondylar roof. This finding has high specificity for an ACL tear.
-
Flattened axis of the distal ACL as a primary sign of ACL tear. This sign has very high specificity for ACL injury. Visualization of the proximal ACL is poor, further confirming tear.
-
Subtle flattened axis as a primary sign of ACL tear. Sagittal T2-weighted image MRI shows axis of the ACL (arrowhead) to be slightly more horizontal than that of the intercondylar roof, or Blumensaat line (arrow), in this patient with arthroscopically proven ACL tear.
-
ACL tear on an axial image. Neutral-weighted fast spin-echo (FSE) fat-saturated MRI shows an abnormally truncated, small ACL remnant in the upper intercondylar notch (arrow). Surrounding edema is present.
-
ACL tear on axial image. T2-weighted fat-saturated fast spin-echo axial image shows nonvisualization of the ACL in the upper intercondylar notch (arrow). A large knee effusion and a Baker cyst are noted incidentally.
-
Pivot shift bone bruises of the femur and tibia as a secondary sign of an ACL tear. Sagittal T2-weighted fast spin-echo fat-saturated MRI shows typical pivot-shift subchondral bone bruises of the posterior lateral tibial plateau and lateral femoral condyle near the anterior horn meniscus. The probability of an ACL tear is very high if both pivot shift bone bruises are present, only slightly lower if either the tibial or femoral bone bruise is seen in isolation.
-
Pivot-shift osteochondral fracture of the lateral femoral condyle. This is a sagittal gradient-echo MRI in 17-year-old boy with an arthroscopically proven ACL tear. The fracture is manifest by focal cortical indentation of lateral femoral condyle (arrow), near the anterior horn lateral meniscus. This fracture was accompanied by typical femoral and tibial pivot-shift bone bruises, as best demonstrated on T2-weighted sequences.
-
Contrecoup medial bone bruise of the tibia in a patient with an ACL tear. High-signal bone bruise in the posteromedial aspect of the tibial plateau (arrow). This is a common finding in patients with ACL tears with pivot-shift/twisting mechanisms. This bone bruise is a marker for a pronounced twisting injury. As such, nearby medial meniscal tears are exceptionally frequent. (Even when no meniscal tears are seen, occult medial meniscal-meniscocapsular junction tears are not uncommonly present.)
-
Severe medial contrecoup bone bruise of the posteromedial tibia with associated impaction fracture. Patient is a 26-year-old man with an arthroscopically proven ACL tear.
-
Anterior translation of tibia as a secondary sign of an ACL tear. Sagittal T1-weighted image in a patient with an arthroscopically proven ACL tear shows mild anterior translation of the tibia. As a result, a tangent line to the posterior margin of the tibia passes through the posterior horn lateral meniscus (uncovered meniscus sign). In normal knees, this line passes posterior to the meniscus. This sign should be sought on an image through the midportion of the lateral femoral condyle. Both chronic and acute ACL tears often demonstrate anterior translation of the tibia.
-
ACL insufficiency in a pediatric patient secondary to tibial avulsion fracture. Sagittal T2-weighted MRI shows a minimally displaced fracture of the tibia at the insertion of the ACL (arrow). Such avulsions are more common in children than in adults.
-
Posterior cruciate ligament (PCL) redundancy as a secondary sign of an anterior cruciate ligament (ACL) tear. T1-weighted sagittal MRI shows an unusually arched PCL (arrow). This is a relatively unreliable secondary sign of ACL tear. Many patients with this finding do not have an ACL tear and some patients with an ACL tear do not demonstrate a redundant PCL. However, this patient did have an arthroscopically proven ACL tear.
-
Segond fracture in a patient with an ACL tear. T1 coronal image demonstrates stereotypical elongate fracture fragment along the proximal and lateral margin of the tibia (arrow). This fracture has a very high statistical association with ACL tear. (Torn ACL is visualized in intercondylar notch.)
-
Segond fracture in a patient with an ACL tear. Fat-saturated proton-weighted fast spin echo image shows stereotypical elongate tibial fracture fragment (arrow). (Retracted, discontinuous ACL fibers are visible in the intercondylar notch.)
-
Segond fracture. Anteroposterior (AP) knee radiograph shows a linear fracture fragment that parallels the proximal lateral surface of the tibia (arrow). The probability of an ACL tear is very high in patients with a Segond fracture.
-
Osteochondral fracture of the lateral femoral condyle as secondary sign of a tear of the ACL. A mild indentation is frequently seen in this location (the condylopatellar groove) in normal knees. A pronounced or irregular contour alteration, as seen here (arrow), strongly suggests a pivot-shift osteochondral fracture in association with an ACL tear.
-
Patient with an osteochondral fracture of lateral femoral condyle similar to that shown in the previous image. Note the exaggerated condylopatellar groove in this patient with arthroscopically proven tear of the ACL.
-
Anterior cruciate ligament (ACL) insufficiency secondary to distal tibial bony avulsion. An avulsion fracture (arrow) is seen at the expected region of the distal insertion of the ACL near the tibial spines. This finding should suggest the possibility of ACL insufficiency/injury because the ACL inserts just lateral to the tibial spine. This is often an isolated injury (with or without ACL compromise) in children. In adults, however, such fractures imply great force; the fractures are often more extensive than expected and are usually accompanied by other internal derangements.
-
Partial ACL tear. T2 sagittal image shows attenuated appearance of ACL and question of subtle flattening of the axis of the ACL.
-
(Same patient as in the previous image.) Partial tear of the ACL. Axial images show abnormally small, high-signal fragmentary appearance of the ACL.
-
(Same patient as in the previous image.) Partial tear of the anterior cruciate ligament (ACL). Axial image showing poorly visualized, high-signal, fragmented ACL.
-
(Same patient as in the previous image.) Partial ACL tear. Sagittal T2-weighted image shows typical ACL-tear related pivot-shift bone bruises of the lateral femoral condyle and the posterolateral tibia. Patient had a normal Lachman test. These images demonstrate that secondary signs of ACL tear (eg, pivot-shift bone bruises) can occur with partial ACL tears and that high-grade partial tears are difficult to distinguish from complete tears.
-
Partial tear of the ACL. T1-weighted sagittal MRI image shows disrupted ACL fibers proximally compatible with an ACL tear.
-
(Same patient as in previous image.) Partial tear of the ACL. T1-weighted sagittal MRI slice, immediately adjacent to the previous image, shows a normal-appearing ACL. Arthroscopy confirmed a partial tear of the ACL. Partial ACL tears may be suggested in the proper clinical setting when primary signs of ACL tear are present, but at least one slice shows a normal, taut-appearing ACL.
-
Partial ACL tear (arthroscopically proven). Images show unusually attenuated appearing ACL surrounded by increased high-signal edema/hemorrhage. With subtle/equivocal primary signs of ACL injury, one must look for other secondary signs of ACL injury and correlate with clinical history/Lachman test findings. One could also consider problem-solving additional MRI sequences.
-
Chronic tear of the ACL with empty notch sign. T1-weighted coronal MRI shows only fat in the lateral intercondylar notch; the ACL is absent. A normal posterior cruciate ligament (PCL) is present in the medial aspect of the notch (arrow). This is a frequent MRI appearance of a chronic ACL tear after the resolution of acute edema and hemorrhage.
-
Chronic tear of the ACL with proximal, focal hyperintense disruption. Sagittal T2-weighted fast spin-echo MRI shows focal fluid-intensity interruption of the proximal ACL (arrow). Absence of surrounding edemalike signal intensity is consistent with the chronic nature of the tear, as confirmed by history and subsequent endoscopy.
-
Chronic tear of the ACL, false-negative result on MRI. The radiologist interpreted this sagittal T2-weighted fast spin-echo fat-saturated MRI, and other images, as normal. In retrospect, the axis of the ACL is abnormally horizontal relative to the roof of the intercondylar notch. Arthroscopy revealed a chronically and grossly insufficient ACL with a few fibers inserting on posterior cruciate ligament (PCL). A chronically torn ACL, with low-signal fibrous healing, can appear misleadingly normal on MRI.
-
Chronic tear of the ACL, with false-negative MRI report. The proximal ACL appears slightly attenuated; however, in the absence of other primary or secondary signs of tear, this appearance lacks specificity for an ACL tear. Images in other planes appeared normal in this patient; however, endoscopy revealed a chronic incompetent ACL. This case again demonstrates that chronic ACL tears may present a challenge to the MR-reader.
-
Suspected mucoid degeneration or intraligamentous ganglion cyst of the anterior cruciate ligament (ACL). Patient had no history of trauma and no instability on physical examination. High-signal focal enlargement of the proximal ACL is noted. The proximal splaying apart of fibers with "celery-stalk" appearance suggests mucoid degeneration; however, involvement of only the proximal ACL is more typical of intraligamentous ganglion cyst. Before diagnosing either of these entities, secondary MR signs of ACL tear should be excluded and the patient should be confirmed as having a negative Lachman test result.
-
Ganglion cyst of the intercondylar notch (unproven). Cystic focal signal abnormality immediately posterior to the proximal aspect of the ACL. The fibers of the ACL proper appeared to be uninvolved on all sequences. Fluid-signal ganglion cysts (vs synovial cysts or joint recesses) are extremely commonly visualized in the pericruciate regions on MR scans of the knee.
-
Vertically oriented lateral collateral ligament (LCL) as a secondary sign of anterior cruciate ligament (ACL) injury. The entire fibular collateral ligament is visualized on a single coronal image. This ligament is ordinarily oblique to the coronal plane but is verticalized in the setting of ACL tear-related anterior tibial translocation.
-
Osseous avulsion of the anterior cruciate ligament (ACL) insertion. Gradient echo sagittal image demonstrates a displaced tibial fracture fragment at the distal ACL insertion. The MRI reader must be vigilant as these fractures are often subtle and easily missed. In indeterminate cases, plain films or CT may be beneficial.
-
Normal double bundle anterior cruciate ligament (ACL) anatomy. Axial and coronal proton density-weighted fat-saturation 3-Tesla images demonstrate normal anteromedial and posterolateral bundles in 2 different patients.
-
Deep lateral femoral notch (sulcus) sign as a secondary sign of anterior cruciate ligament (ACL) injury. A lateral radiograph demonstrates an unusually pronounced lateral condylopatellar groove. Such appearances should suggest to the reader the possibility of a pivot-shift impaction injury.
-
Chronic anterior cruciate ligament (ACL) tear. T1-weighted image of 64-year-old man demonstrating abnormal flattening of the ACL axis relative to the intercondylar roof. Acute phase edema in the intercondylar notch has resolved, with the ACL again surrounded by normal fat signal.
-
Normal anterior cruciate ligament (ACL) in the axial plane. T2-weighted images in 21-year-old woman. A. Proximal ACL. The ACL is low signal and cigar-shaped. It hugs the lateral wall of the high posterior intercondylar notch. B. Mid ACL. The ligament is coursing through the notch in anterior and medial direction. C. Distal ACL. The ACL diverges into a horseshoe-shaped array of fascicles near its insertion on the tibia. The distal ligament here is more difficult to critically evaluate.
-
Acute anterior cruciate ligament (ACL) tear. T2-weighted sagittal image in 22-year-old woman. Females have a variably increased incidence of ACL injury per hour of participation in activities at risk.
-
Pivot-shift twisting mechanism lateral bone bruises in a patient with anterior cruciate ligament (ACL) tear. T2-weighted sagittal image in 22-year-old woman. This pattern of lateral bone bruises occurs with lateral rotation of the femur relative to the tibia and indicates a very high likelihood of an associated ACL injury. This patient had meniscal and medial collateral ligament (MCL) injuries in addition to an ACL tear.
-
Hyperextension anterior "kissing" bone bruises in patient with anterior cruciate ligament (ACL) tear. Sagittal T2-weighted image in 25-year-old man. Anterior bone bruises of this nature indicate a hyperextension mechanism of injury. The reader should thus be alert for the possibility of ACL, posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and neurovascular injuries. (This patient had ACL and LCL tears.)
-
Biceps femoris (lateral collateral ligament complex) injury in patient with anterior cruciate ligament (ACL) tear. Coronal T2-weighted image. Orthopedic surgeons often opt to operate earlier than customary in ACL-injured patients who also have a lateral collateral ligament (LCL) tear. This highlights the importance of accurate diagnosis of comorbid injuries in the ACL-injured patient.
-
Kissing anterior cruciate ligament (ACL)/posterior cruciate ligament (PCL)/fibular collateral (FCL). Grade 2. Medial collateral ligament (MCL). Axial.
-
Kissing anterior cruciate ligament (ACL)/posterior cruciate ligament (PCL)/fibular collateral (FCL). Grade 2. Medial collateral ligament (MCL). Sagittal.
-
Hyperextension anterior "kissing" bone bruises as a secondary sign of anterior cruciate ligament (ACL) tear. Sagittal T2-weighted image in 52-year-old woman. This pattern of bone bruises is reported to be associated with ACL tear in about 50% of patients. Patient had clinical history of subluxation and other images showed posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and medial collateral ligament (MCL) injuries.
-
Partial tear versus mucinous degeneration of the anterior cruciate ligament (ACL) (unproven case). T2-weighted sagittal image. Patient presented with pain and no history of significant trauma. The ACL is enlarged with non-fluid-like increased signal separating intact-appearing straight ACL fibrils. The differential diagnosis for this appearance includes mucinous degeneration (not uncommon) and a delaminating partial tear. Detailed history and Lachman test is necessary to differentiate.
-
Anterior cruciate ligament (ACL) tear in a 25-year-old patient with biceps femoris tear. Kissing bone bruises. Hyperextension.
-
Normal anterior cruciate ligament (ACL) in coronal plane. T2-weighted image in 25-year-old woman. In this plane, the normal ACL often appears much more attenuated than in the sagittal plane. Again, however, the ACL manifests as one or several straight, nonangulated, distally diverging low-signal bands. In this patient, the anteromedial and posterolateral bundles are readily differentiated. Note the lateral position of the ACL in the intercondylar notch. Note also the predominant fat signal surrounding the ACL: this is usually replaced by edema in the setting of an acute tear.
-
Normal anterior cruciate ligament (ACL) in sagittal plane. T2-weighted image in 25-year-old woman. The robust ligament demonstrates uninterrupted low-signal linear bands. It is nonangulated and either ruler-straight or demonstrating minimal convex-inferior sagging. The long axis of a normal ligament should be at least as steep as the nearby intercondylar roof.
-
Arcuate fracture of the fibular head as a secondary sign of possible anterior cruciate ligament (ACL) (and lateral collateral ligament [LCL]/posterior cruciate ligament [PCL]) injury. Forty-year-old man with a history of knee dislocation. A. Lateral radiograph shows several fibular head avulsion fracture fragments. B. Coronal T2-weighted MRI shows several subtle fibular head low-signal fracture fragments (arrow) and associated marrow edema of the fibular head. The LCL is absent/torn. The PCL and ACL were also torn. A fibular head avulsion fracture is suggestive (although not diagnostic) of a hyperextension/varus injury, which, in turn, may cause a combination of PCL, LCL, and ACL injuries.
-
Problem-solving oblique coronal sequence. This additional sequence may be helpful in equivocal ACL-tear cases. On a sagittal scout image, the MRI technologist prescribes thin (3mm or less) T2-weighted or proton-density-weighted fat suppression images along the long axis of the ACL.
-
Problem-solving oblique coronal sequence. Note how the entire proximal-to-distal ACL is visible on one coronal image. On conventional coronal images, the ACL is visualized on multiple successive slices. Note: we ordinarily perform this extra sequence with a smaller field-of-view than evident here.
-
Problem-solving sequence with knee in flexed position. This sequence may be helpful when conventional MRI sequences demonstrate an equivocal proximal ACL tear near its origin off the femur. This patient is actually status post ACL graft reconstruction. Note the helpful separation of the anterior aspect of the proximal ACL from the intercondylar roof, allowing optimal evaluation.







