Practice Essentials
Magnetic resonance imaging (MRI) is the most powerful, accurate, noninvasive method for diagnosing meniscal tears. It is more accurate than physical examination and has influenced clinical practice and patient care by eliminating unnecessary diagnostic arthroscopies or by identifying an alternative diagnosis whose clinical presentation may mimic meniscal tears. MRI accurately depicts the anatomy and pathology affecting almost every joint in the body. Because MRI is highly accurate, most leading orthopedic surgeons prefer MRI to diagnostic arthroscopy. [1, 2, 3, 4, 5, 6, 7, 8]
The incidence of meniscal tears has been estimated to be about 60 per 100,000, but the true incidence is expected to be much higher. Jarraya et al found that more than 75% of patients with symptomatic osteoarthritis had a meniscal injury. [8, 9, 10]
The International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine (ISAKOS) has classified meniscal tears on the basis of parameters such as tear depth, tear width, radial location, tear pattern, tissue quality, tear length, and tissue excision. [11, 12]
The knee menisci were once thought to be functionless remnants of a leg muscle and expendable components of the knee. Much has been learned through laboratory investigation, clinical experience, and radiologic imaging. The meniscus is now known to play an important role in the complex biomechanics of the knee. For instance, it is involved in joint stability, load sharing and transmission, shock absorption, [13] and nutrition and lubrication of the articular cartilage. [14, 15, 16]
Meniscal injuries are a common problem in sports; they are the most frequent injury to the knee joint. Such injuries are especially prevalent among competitive athletes, particularly those who play soccer, football, basketball, and (sometimes) baseball. As the number of people participating in sports has greatly increased, so has the number of knee injuries. [17]
(Meniscal tears are displayed in the images below.)
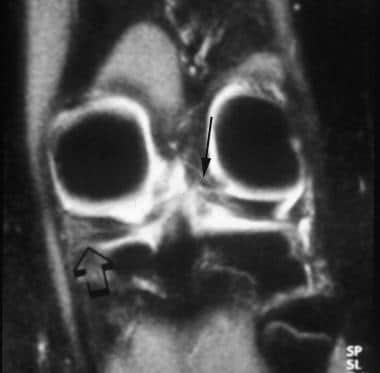
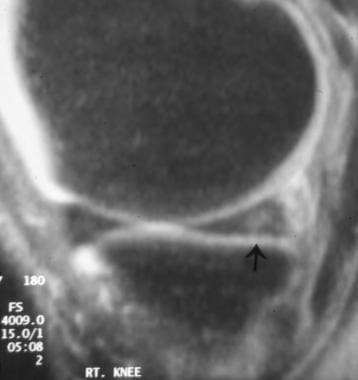
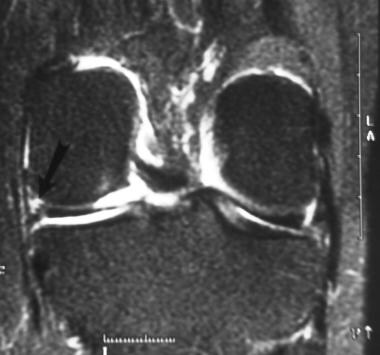 Coronal fat-saturated proton density–weighted image shows the popliteus recess containing joint fluid and located between the lateral aspect of the posterior horn of the lateral meniscus and the joint capsule. An extensive tear is present in the posterior horn of the medial meniscus (arrow). Note the normal oblique upward orientation of the posterior medial horn of the lateral meniscus.
Coronal fat-saturated proton density–weighted image shows the popliteus recess containing joint fluid and located between the lateral aspect of the posterior horn of the lateral meniscus and the joint capsule. An extensive tear is present in the posterior horn of the medial meniscus (arrow). Note the normal oblique upward orientation of the posterior medial horn of the lateral meniscus.
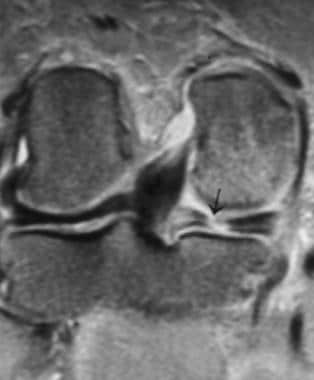 Coronal fat-saturated proton density–weighted image shows the popliteus tendon originating from an undulation of the lateral femoral condyle. From there, it passes through the popliteus recess to insert on the proximal posterior tibial metaphysis. A radial tear (arrow) is present in the posterior horn of the medial meniscus.
Coronal fat-saturated proton density–weighted image shows the popliteus tendon originating from an undulation of the lateral femoral condyle. From there, it passes through the popliteus recess to insert on the proximal posterior tibial metaphysis. A radial tear (arrow) is present in the posterior horn of the medial meniscus.
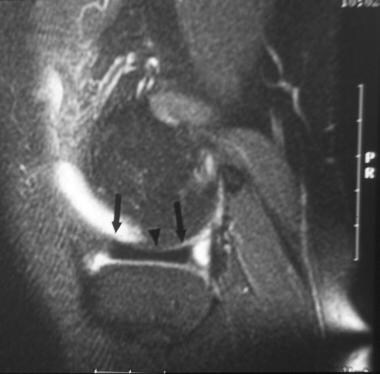
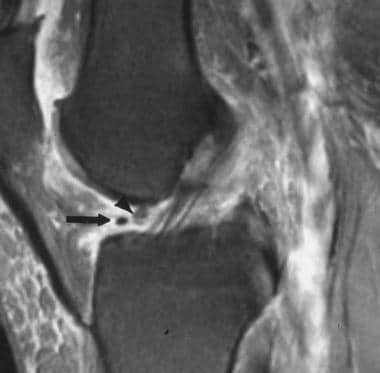
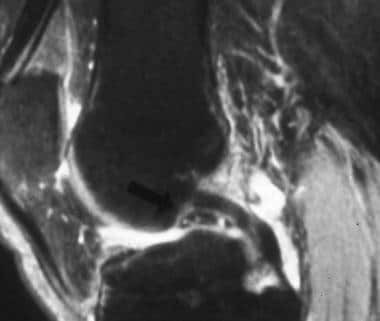
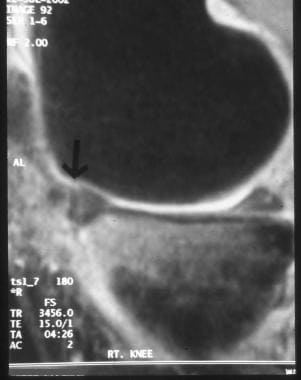 Sagittal fat-saturated proton density–weighted image shows a full-thickness tear to the periphery of the anterior horn of the medial meniscus (MM). Tears in this location have a good likelihood of healing without surgical repair because they occur in the zone with a good blood supply to the meniscus. Also present is a partial thickness tear to the undersurface of the posterior horn of the MM.
Sagittal fat-saturated proton density–weighted image shows a full-thickness tear to the periphery of the anterior horn of the medial meniscus (MM). Tears in this location have a good likelihood of healing without surgical repair because they occur in the zone with a good blood supply to the meniscus. Also present is a partial thickness tear to the undersurface of the posterior horn of the MM.
 Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
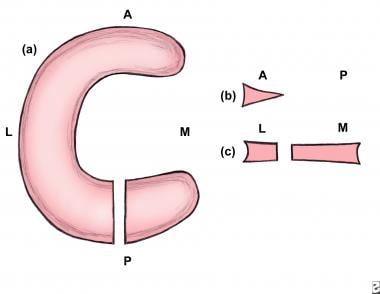
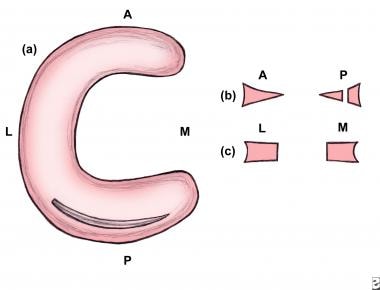 Axial illustration of a full-thickness longitudinal tear of the posterior horn. The meniscus is viewed from above in (a), sagittal in (b), and coronal in (c). For Image 67-70, A = anterior, L = lateral, M = medial, and P = posterior.
Axial illustration of a full-thickness longitudinal tear of the posterior horn. The meniscus is viewed from above in (a), sagittal in (b), and coronal in (c). For Image 67-70, A = anterior, L = lateral, M = medial, and P = posterior.
 Axial illustration of a full-thickness radial tear of the posterior horn. The meniscus is viewed from above.
Axial illustration of a full-thickness radial tear of the posterior horn. The meniscus is viewed from above.
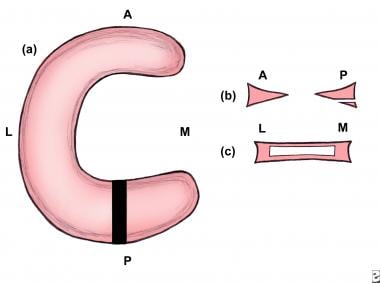 Axial illustration of a full-thickness horizontal tear of the posterior horn. The meniscus is viewed from above.
Axial illustration of a full-thickness horizontal tear of the posterior horn. The meniscus is viewed from above.
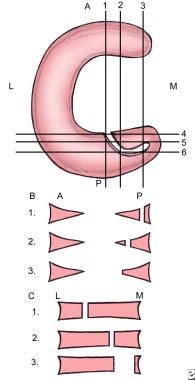 Axial illustration of an oblique (parrot beak) tear of the posterior horn. The meniscus is viewed from above. In B, image 1 is most lateral, image 2 is middle, and image 3 is most medial. In C, image 1 is most anterior, image 2 is middle, and image 3 is most posterior.
Axial illustration of an oblique (parrot beak) tear of the posterior horn. The meniscus is viewed from above. In B, image 1 is most lateral, image 2 is middle, and image 3 is most medial. In C, image 1 is most anterior, image 2 is middle, and image 3 is most posterior.
Clinical examination
Unlike MRI, clinical examination cannot demonstrate the location, shape, or length of a meniscal tear. These factors are important in treatment decisions. Large, blinded prospective studies with diverse patient populations suggest that for experienced clinicians, the sensitivity of physical examination for detecting meniscal tears is 70-90%. [18, 19, 20, 21] The negative predictive value (NPV) is no greater than 67%; therefore, about one third of meniscal tears are missed with clinical screening alone. In situations of multiple knee lesions, the accuracy of clinical examination in diagnosing meniscal tears decreases to 30%. [19, 20]
The clinical diagnosis of meniscal tears becomes more difficult and unreliable in the presence of concurrent acute ligamentous injuries of the knee. With acute anterior cruciate ligament (ACL) tears, the sensitivity for diagnosing medial meniscus (MM) tears is 45% and 58% for lateral meniscus (LM) tears. The sensitivity of joint line tenderness for diagnosing meniscal tears is 75%. The sensitivity of the Apley grinding test for meniscal tears is about 45%. The sensitivity of the Payr test for diagnosing meniscal tears is about 40%. [18, 19, 20] Specificity also decreases, most likely due to the presence of tibial and femoral bone bruises that frequently accompany acute ACL tears. Pain from these bone injuries can cause joint-line tenderness, a finding that otherwise suggests the presence of a meniscal tear. [18, 19, 20, 21]
Advantages of MRI
In many cases, MRI results lead to changes in the proposed management. One study determined that about one third of all diagnostic arthroscopies need not be performed if MRI is used; another study showed that the use of MRI prevented 51% of diagnostic arthroscopic procedures; and a third study showed that with the use of MRI, the morbidity associated with arthroscopy was avoided. [20]
MRIs show many of the essential characteristics of meniscal tears critical to management, such as their location, shape, length, and depth. In this way, MRI helps to make an accurate assessment of stability and of the likelihood of tear propagation, and it enables one to determine whether the meniscal tear can be repaired. It is advantageous to know ahead of time if a given meniscal tear can be repaired, because the additional equipment, surgical assistants, and time needed for repair can be anticipated. Patients also benefit from knowing early on whether surgery is necessary. The recovery time for meniscal repair is longer than that for partial meniscectomy (PM). Patients may want to time surgery to fit in with their other obligations. [1, 20, 22, 23]
When combined with clinical data, such as the patient's age, athletic requirements, and physical findings (eg, possible associated ligamentous injuries), a treatment plan may be developed by assessing the need for and timing of surgery and by determining the type of surgery (meniscal debridement, rasping, repair, partial or total resection, or meniscal transplantation). MRI may be used to identify other injuries, such as ligament tears, especially anterior cruciate ligament tears, the presence of which may also influence the decision whether to perform surgery. [1, 20, 22]
With MRI, physicians may obtain images in several planes, providing multiple perspectives on meniscal and ligamentous injuries. Other advantages include the following:
-
MRI does not expose the patient to ionizing radiation
-
MRI does not normally involve the intravenous administration of contrast material, the use of which is associated with a small but definite number of adverse effects
-
MRI does not require joint manipulation
-
MRI is painless and can be performed in less than 35 minutes
-
MRI does not require the intra-articular injection of iodinated radiographic contrast material, which is needed for arthrography
Arthrography has been supplanted by MRI except for patients who are too large to fit into the MRI unit or for patients who have contraindications to MRI (eg, intracranial aneurysm clips, orbital metallic foreign bodies are present). Magnetic resonance arthrography is used to evaluate residual or recurrent meniscal tears after meniscal surgery. The detection of residual or recurrent meniscal tears following meniscectomy or meniscal repair is difficult with conventional MR images. [24]
Radiography
Plain radiography is extremely limited in the assessment of meniscal tears. Radiographs may be obtained to rule out unsuspected lesions, such as osteochondritis dissecans and loose bodies. In the presence of a discoid meniscus (DM), radiographs may show widening of the medial or lateral joint compartments; hypoplasia of the lateral femoral condyle related to the increased size of the LM; a high fibular head; cupping of the lateral tibial plateau; or a squared-off lateral femoral condyle.
Anatomy
Normal Anatomy on MRIs
Structures in the sagittal plane
Centrally, the normal meniscus is composed of 2 separate triangular structures: the anterior horn and the posterior horn. The apices (free edges or inner margins) appear as sharp points of the triangle facing each other (see the first image below). On the lateral side of the knee, the triangular anterior and posterior horns of the lateral meniscus (LM) are equal in size (see the second image below). On the medial side of the knee, the posterior horn of the medial meniscus (MM) is larger than the anterior horn (see the third image below). [18]
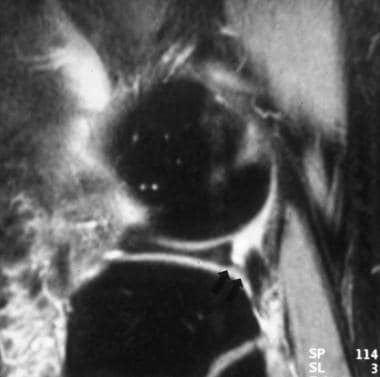
 Coronal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus (MM) extending to the undersurface near the junction with the joint capsule. Such tears may be missed on arthroscopy because that part of the knee joint is difficult to access. Also present is a tear to the posterior medial horn of the lateral meniscus (LM) as it slopes obliquely inward. A false-positive diagnosis of meniscal tear can be made when one evaluates this region because of the magic angle effect. Tears persist when the echo time (TE) is varied and when T2-weighted images are obtained. True tears can also be confirmed by visualizing them on sagittal or axial projections.
Coronal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus (MM) extending to the undersurface near the junction with the joint capsule. Such tears may be missed on arthroscopy because that part of the knee joint is difficult to access. Also present is a tear to the posterior medial horn of the lateral meniscus (LM) as it slopes obliquely inward. A false-positive diagnosis of meniscal tear can be made when one evaluates this region because of the magic angle effect. Tears persist when the echo time (TE) is varied and when T2-weighted images are obtained. True tears can also be confirmed by visualizing them on sagittal or axial projections.
 Sagittal fat-saturated proton density–weighted image of the lateral compartment shows the relative equal size of the anterior and posterior horns of the lateral meniscus. The meniscal body has the normal configuration of a bow tie.
Sagittal fat-saturated proton density–weighted image of the lateral compartment shows the relative equal size of the anterior and posterior horns of the lateral meniscus. The meniscal body has the normal configuration of a bow tie.
 Sagittal fat-saturated proton density–weighted image of the medial compartment shows the larger posterior horn (arrowhead) and the smaller anterior horn.
Sagittal fat-saturated proton density–weighted image of the medial compartment shows the larger posterior horn (arrowhead) and the smaller anterior horn.
Peripherally (medially for the medial meniscus and laterally for the lateral meniscus), the menisci have a bow-tie configuration, as shown in the images below. The anterior and posterior horns are taller than the thinner and interposed body of the meniscus.
 Sagittal fat-saturated proton density–weighted image demonstrates the concave superior meniscal surface (arrows), which improves contact with the femoral epicondyles, and a flat undersurface, which improves contact with the tibial plateau. The periphery (outer edges) is thicker than the central portion (arrowhead), allowing for firm attachment to the joint capsule. Note the normal bow-tie appearance of the meniscal body.
Sagittal fat-saturated proton density–weighted image demonstrates the concave superior meniscal surface (arrows), which improves contact with the femoral epicondyles, and a flat undersurface, which improves contact with the tibial plateau. The periphery (outer edges) is thicker than the central portion (arrowhead), allowing for firm attachment to the joint capsule. Note the normal bow-tie appearance of the meniscal body.
 Sagittal fat-saturated proton density–weighted image shows the inferior fascicle. In this location, the superior fascicle is not present. Note the normal bow-tie appearance of the meniscal body.
Sagittal fat-saturated proton density–weighted image shows the inferior fascicle. In this location, the superior fascicle is not present. Note the normal bow-tie appearance of the meniscal body.
 Coronal proton density–weighted image shows extensive grade 2 signal intensity in the anterior and posterior horns of the medial meniscus. However, the signal intensity does not extend to a joint surface.
Coronal proton density–weighted image shows extensive grade 2 signal intensity in the anterior and posterior horns of the medial meniscus. However, the signal intensity does not extend to a joint surface.
Both menisci have anterior and posterior roots, which attach the anterior and posterior horns to the tibial plateau, on either side of the centrally placed tibial spine (see the image below). These attachments are referred to as roots. [25, 26, 27, 28, 29]
 Sagittal proton density–weighted image shows the tibial insertion site of the posterior horn of the medial meniscus (MM).
Sagittal proton density–weighted image shows the tibial insertion site of the posterior horn of the medial meniscus (MM).
Popliteus tendon and sheath
The popliteus tendon and its accompanying sheath course through the posterolateral portion of the posterior horn of the LM in an oblique anterosuperior to posteroinferior direction. It is seen on the more lateral images of the LM (see the images below).
 Coronal proton density–weighted image shows the ligament of Wrisberg originating from the posterior medial horn of the medial meniscus and passing obliquely upwards (arrow) to attach to the posterolateral aspect of the medial femoral epicondyle.
Coronal proton density–weighted image shows the ligament of Wrisberg originating from the posterior medial horn of the medial meniscus and passing obliquely upwards (arrow) to attach to the posterolateral aspect of the medial femoral epicondyle.
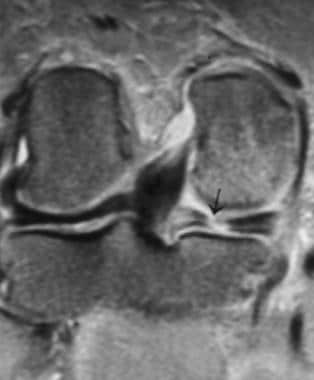 Coronal fat-saturated proton density–weighted image shows the popliteus tendon originating from an undulation of the lateral femoral condyle. From there, it passes through the popliteus recess to insert on the proximal posterior tibial metaphysis. A radial tear (arrow) is present in the posterior horn of the medial meniscus.
Coronal fat-saturated proton density–weighted image shows the popliteus tendon originating from an undulation of the lateral femoral condyle. From there, it passes through the popliteus recess to insert on the proximal posterior tibial metaphysis. A radial tear (arrow) is present in the posterior horn of the medial meniscus.
Two fascicles connect the posterior horn of the LM at the popliteus tendon sheath level to the joint capsule. The inferior fascicle is seen on the more lateral images through the tendon. Here, the superior fascicle is absent. More medially, both superior and inferior fascicles are present. The most medial images through the tendon show the superior fascicle and absence of the inferior fascicle. The thickness of the popliteus tendon sheath varies in size from a thin line to a thick band.
Structures in the coronal plane
The coronal plane is the best plane in which to image the meniscal bodies (see the images below). Each meniscal body looks like a triangle with the pointed apex in the innermost part of the meniscus. The anterior and posterior horns appear as flat slabs. The root of the posterior horn of the LM is directed obliquely upward from a lateral to medial direction. The popliteus recess is located in the outer portion of the lateral joint compartment. It can be identified either by the presence of joint fluid within it or by the popliteus tendon originating from the distal lateral femur, above the joint, and passing through the sheath to insert on the back of the proximal tibia. [18, 30]
 Coronal fat-saturated proton density–weighted image of the mid knee shows the normal appearance of the body of the medial and lateral menisci. The apices (inner portions) are the thinnest part of the meniscus and are more central in the knee joint. The periphery, meniscal bases, outer portion (arrow and arrowhead) is the thickest part and contains the blood vessels supplying the meniscus.
Coronal fat-saturated proton density–weighted image of the mid knee shows the normal appearance of the body of the medial and lateral menisci. The apices (inner portions) are the thinnest part of the meniscus and are more central in the knee joint. The periphery, meniscal bases, outer portion (arrow and arrowhead) is the thickest part and contains the blood vessels supplying the meniscus.
 Coronal fat-saturated proton density–weighted image shows the relative size of the posterior horns of the medial and lateral menisci. The posterior horn of the medial meniscus (left arrow) is thicker than the posterior horn of the lateral meniscus (right arrow). Note the normal dark appearance (relative lack of signal intensity) in the menisci. The medial portion of the posterior horn of the lateral meniscus (ie, the meniscus on top of the fibula) is directed upward obliquely, from a lateral to medial direction. This is its normal course.
Coronal fat-saturated proton density–weighted image shows the relative size of the posterior horns of the medial and lateral menisci. The posterior horn of the medial meniscus (left arrow) is thicker than the posterior horn of the lateral meniscus (right arrow). Note the normal dark appearance (relative lack of signal intensity) in the menisci. The medial portion of the posterior horn of the lateral meniscus (ie, the meniscus on top of the fibula) is directed upward obliquely, from a lateral to medial direction. This is its normal course.
 Coronal fat-saturated proton density–weighted image shows the popliteus recess containing joint fluid and located between the lateral aspect of the posterior horn of the lateral meniscus and the joint capsule. An extensive tear is present in the posterior horn of the medial meniscus (arrow). Note the normal oblique upward orientation of the posterior medial horn of the lateral meniscus.
Coronal fat-saturated proton density–weighted image shows the popliteus recess containing joint fluid and located between the lateral aspect of the posterior horn of the lateral meniscus and the joint capsule. An extensive tear is present in the posterior horn of the medial meniscus (arrow). Note the normal oblique upward orientation of the posterior medial horn of the lateral meniscus.
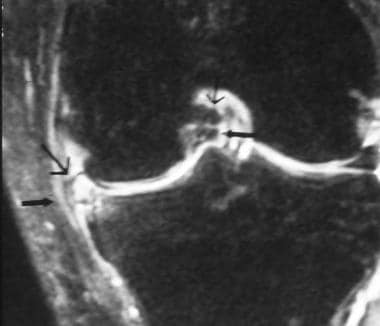
 Coronal fat-saturated proton density–weighted image shows the dark appearing popliteus tendon (arrows) passing through the popliteus recess. The posterior medial horn of the lateral meniscus is directed obliquely upward.
Coronal fat-saturated proton density–weighted image shows the dark appearing popliteus tendon (arrows) passing through the popliteus recess. The posterior medial horn of the lateral meniscus is directed obliquely upward.
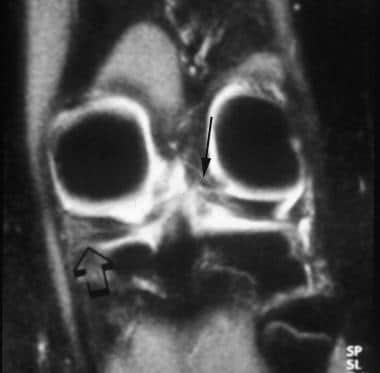 Coronal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus (MM) extending to the undersurface near the junction with the joint capsule. Such tears may be missed on arthroscopy because that part of the knee joint is difficult to access. Also present is a tear to the posterior medial horn of the lateral meniscus (LM) as it slopes obliquely inward. A false-positive diagnosis of meniscal tear can be made when one evaluates this region because of the magic angle effect. Tears persist when the echo time (TE) is varied and when T2-weighted images are obtained. True tears can also be confirmed by visualizing them on sagittal or axial projections.
Coronal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus (MM) extending to the undersurface near the junction with the joint capsule. Such tears may be missed on arthroscopy because that part of the knee joint is difficult to access. Also present is a tear to the posterior medial horn of the lateral meniscus (LM) as it slopes obliquely inward. A false-positive diagnosis of meniscal tear can be made when one evaluates this region because of the magic angle effect. Tears persist when the echo time (TE) is varied and when T2-weighted images are obtained. True tears can also be confirmed by visualizing them on sagittal or axial projections.
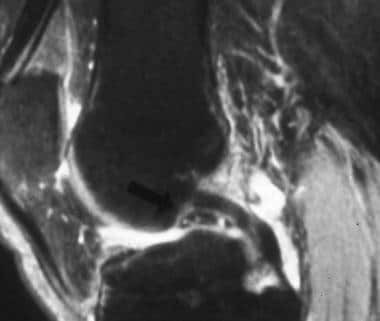
 Coronal fat-saturated proton density–weighted image of the posterior portion of the knee joint. A circular, fluid-filled structure (arrow) is present in the upper portion of the most medial portion of the posterior horn of the medial meniscus; it represents a meniscal cyst.
Coronal fat-saturated proton density–weighted image of the posterior portion of the knee joint. A circular, fluid-filled structure (arrow) is present in the upper portion of the most medial portion of the posterior horn of the medial meniscus; it represents a meniscal cyst.
The insertion of the semimembranosus tendon is located posterior along the subarticular surface of the medial aspect of the proximal tibial metaphysis (see the images below). This is not to be confused with a displaced meniscal fragment.
 Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
 Sagittal fat-saturated proton density–weighted image of the paramedian portion of the lateral joint compartment. The transverse intermeniscal ligament (arrowhead) is about to unite with the anterior horn of the medial meniscus (MM, arrow). Fat is normally present in this region and can mimic a ligament or meniscal tear. By carefully following the course of the ligament on sequential images and by observing a uniformly well-defined, hypointense structure on every image, this pitfall can be avoided. A small, ill-defined, linear soft tissue density is present under the anterior horn. It is separated from the anterior horn by bright fluid. This is a rare tear in this region. The brightness is joint fluid in the tear.
Sagittal fat-saturated proton density–weighted image of the paramedian portion of the lateral joint compartment. The transverse intermeniscal ligament (arrowhead) is about to unite with the anterior horn of the medial meniscus (MM, arrow). Fat is normally present in this region and can mimic a ligament or meniscal tear. By carefully following the course of the ligament on sequential images and by observing a uniformly well-defined, hypointense structure on every image, this pitfall can be avoided. A small, ill-defined, linear soft tissue density is present under the anterior horn. It is separated from the anterior horn by bright fluid. This is a rare tear in this region. The brightness is joint fluid in the tear.
Meniscal roots
The meniscal roots, including the anterior root of the medial meniscus, the anterior root of the lateral meniscus, the posterior root of the medial meniscus, and the posterior root of the lateral meniscus, originate from the anterior and posterior horns of the menisci and anchor the menisci to the tibia. They are critical in maintaining the normal biomechanical functions of the menisci. [31, 25, 32, 26, 27, 28, 33, 29] Root tears involve bony or soft tissue avulsion of the meniscal insertions. [29]
The menisci are attached to the central portion of the tibial plateau by fibers originating from the anterior and posterior horns, the meniscal roots. The anterior root of the medial meniscus has the largest footprint of all the meniscal roots. It inserts broadly into the anterior intracondylar crest. The anterior root of the lateral meniscus inserts on a smaller area posterior to. or on a portion of, the anterior intracondylar crest in front of the lateral tibial tubercle and lateral to the tibial insertion of the ACL, with which it partially blends. The posterior root inserts on a small portion of the posterior slope of the medial tibial tubercle, which is posterior to the insertion of the posterior root of the lateral meniscus.
Most of the posterior root inserts on the horizontal part of the posterior intracondylar area, but some of the fibers attach to the posterior slope of the lateral tubercle and along the intertubercular longitudinal crest that connects the medial and lateral tibial tubercles.
Meniscal flounce
A meniscal flounce is an uncommon meniscal variant characterized by a single symmetrical fold along the free edge of the meniscus. It appears as an S-shaped fold along the free edge on sagittal images and is associated with a truncated but normal meniscus on coronal images.
Normal meniscal signal intensity
The normal meniscus shows uniform, low signal intensity on T1- and T2-weighted images obtained with both conventional and fast-spin echo (FSE) sequences. The low signal is related to a lack of mobile protons in the meniscal fibrocartilage. Subsequent dephasing of hydrogen nuclei results in T2 shortening, contributing to the low signal intensity on all pulse sequences.
Fascicles of the posterior horn of the LM are best evaluated on T2-weighted sagittal images. This is due to the bright fluid in the popliteus tendon sheath and joint space contrasting with the low signal intensity of the fascicles. [34]
Discoid meniscus
Differentiation between a true discoid meniscus (DM) and a slightly larger but normal meniscus may be difficult. The 3 types of discoid menisci are complete, incomplete, and Wrisberg variant. Complete and incomplete discoid menisci vary in their degree of tibial plateau coverage. The Wrisberg variant is the least common and lacks the normal posterior coronary ligament and capsular attachments. This ligament is mobile and can sublux. [35, 36, 37, 38, 39, 31] Discoid menisci most commonly involve the lateral meniscus, with clinical presentation ranging from asymptomatic to snapping, pain, swelling, and reduced range of knee movement. [38]
On sagittal images, the DM has a thickened, bow-tie appearance on 3 consecutive sagittal images. The anterior and posterior horns of the normal meniscus are seen on several images near the intercondylar notch. With a complete DM, no distinct anterior or posterior horn is present. The normal meniscus rapidly tapers from the outer periphery to the center. The presence of equal or nearly equal meniscal height on 2 adjacent peripheral 5-mm-thick images indicates a DM. The anterior and posterior horns of the LM are normally equal in height. An asymmetric discoid LM may have an abnormally large anterior or posterior horn. [40]
On coronal views, the abnormal meniscal body extends more medially toward the intercondylar notch (see the image below).
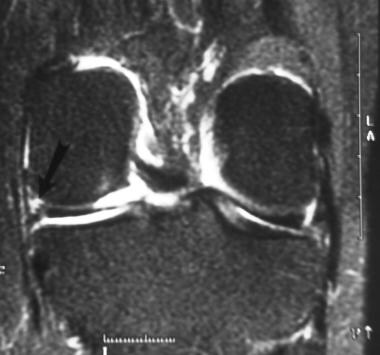
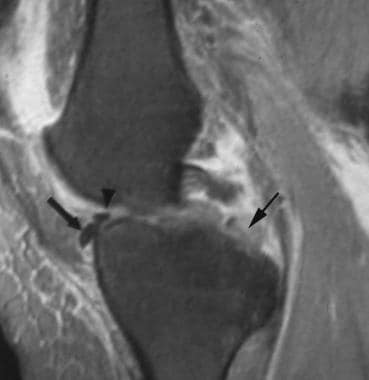
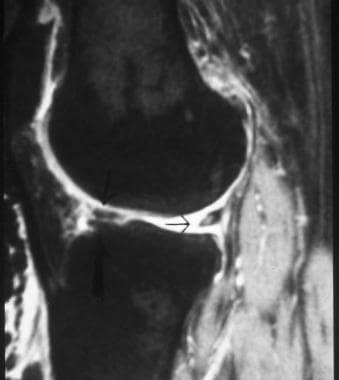
 Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
The posteromedial horn of the MM and the anterior horn of the MM near the roots may have a normal speckled appearance (see the images below).
 Sagittal fat-saturated proton density–weighted image of the paramedian portion of the medial knee. The transverse intermeniscal ligament is about to insert on the anterior horn of the medial meniscus (MM). The anterior horn is normally speckled. The anterior horn is partially displaced off the anterior surface of the tibia by a radial tear more laterally (picture is not shown). A tear involves the posterior horn of the MM (arrow).
Sagittal fat-saturated proton density–weighted image of the paramedian portion of the medial knee. The transverse intermeniscal ligament is about to insert on the anterior horn of the medial meniscus (MM). The anterior horn is normally speckled. The anterior horn is partially displaced off the anterior surface of the tibia by a radial tear more laterally (picture is not shown). A tear involves the posterior horn of the MM (arrow).
 Sagittal fat-saturated proton density-weighted image shows a well-defined, soft tissue density in front of the posterior cruciate ligament (PCL). It is speckled and looks like the normal posterior medial horn of the medial meniscus (MM), but it is in the wrong place. This finding represents a displaced meniscal tear involving the posterior medial horn. The position of the meniscus is referred to as a double PCL because it looks like 2 of these ligaments are present.
Sagittal fat-saturated proton density-weighted image shows a well-defined, soft tissue density in front of the posterior cruciate ligament (PCL). It is speckled and looks like the normal posterior medial horn of the medial meniscus (MM), but it is in the wrong place. This finding represents a displaced meniscal tear involving the posterior medial horn. The position of the meniscus is referred to as a double PCL because it looks like 2 of these ligaments are present.
Coronal images show the smallest width of the meniscal body, making this plane the most sensitive for showing meniscal enlargement. An asymmetric DM with an enlarged body may have a wide meniscal body on coronal images but normal anterior and posterior horns on sagittal images, emphasizing the need for coronal images. Incomplete DM may not extend into the intercondylar notch.
In children, grade 2 signal is frequently seen within the posterior meniscal horns. This is thought to represent normal vasculature, seen in the meniscus of a child. This disappears in adulthood.
Regarding the meniscofemoral ligaments, either the anterior or posterior ligament is present on 33% of MRIs. Both ligaments are present on 3% of examinations. One of the 2 ligaments predominates. The ligament of Humphry is best seen on sagittal images. It is occasionally seen on coronal images. The ligament of Wrisberg is best seen on posterior coronal images. [40, 41]
Discoid meniscus is the most frequent congenital malformation of the menisci and primarily affects the lateral meniscus. It is been noted to be most prevalent in Asian populations. Milewski et al found that Asian children had 2.41 times the odds of surgery for discoid meniscus than white patients. In addition, Hispanic/Latino children had 2.36 times the odds of surgery for discoid meniscus compared with white patients. [42, 39]
Meniscal degeneration
Local increases in the degree of freedom of trapped water molecules within the substance of the meniscus occurs with age, resulting in increased T2 times. The appearance is that of increased signal intensity within the substance of the meniscus on short-TE images. [34]
Meniscal stability
The stabilizers of the medial meniscus include the medial collateral ligament. The deep fibers of the ligament are attached to the meniscus. [43]
The lateral meniscus is stabilized by the coronary ligament, the meniscofemoral ligament, the arcuate ligament, and, possibly, the meniscotibial ligament. [44]
Both menisci are additionally stabilized by the transverse ligament. If any of these supporting ligaments or the meniscus itself degenerates or is torn, the meniscus may become unstable.
The meniscocapsular ligaments comprising the meniscofemoral and meniscotibial ligaments attach the menisci to the posterior femur and posterior tibial plateau, respectively. [45]
Descriptions and Classifications
MRI systems of low, medium, and high field strength can all produce accurate, diagnostic images for identifying meniscal abnormalities. In units with lower field strength, the number of signals averaged may need to be increased to obtain an adequate signal-to-noise ratio. This adjustment, however, increases the imaging time, which increases the risk of patient motion. Even a small amount of motion can degrade the images, jeopardizing the ability to diagnose meniscal tears. [18, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57] An extremity coil is used to optimize the signal-to-noise ratio. A surface coil may be used for better detail in evaluating subtle lesions or suspicious areas. [58]
Protocols and imaging planes
The knee is usually positioned in extension with slight external rotation to facilitate imaging the anterior cruciate ligament (ACL).
High spatial resolution is required to show subtle tears. This requires a field of view of 16 cm or less, a section thickness of 5 mm or less (3-4 mm is preferred), and a matrix of at least 192 X 256 steps in the phase- and frequency-encoding directions. A skip of 0.5 to 1 mm is used between imaging sections. These parameters can be achieved by using a solenoid surface coil. An extremity coil is used to optimize the signal-to-noise ratio. [18, 1, 59]
If subtle lesions or suspicious areas are identified by using the standard extremity coil, high-resolution images can be obtained by using a surface coil, provided that the area of interest is superficial enough to be encompassed by the surface coil with the small field of view. Scanning parameters in this situation include the following: field of view as small as 10 X 10 cm, matrix 256 X 512 (displayed at 512 X 512), section thickness of 3 mm with a 0.3-mm intersection gap, and 3 signals acquired. [58]
Images must be obtained in both the sagittal and coronal planes. Sagittal images are obtained with the knee externally rotated to permit imaging in the plane of the ACL. Meniscal and ACL injuries frequently coexist. Axial images are also obtained to study the supporting ligaments around the knee. Changing coils during an MRI examination is not part of the standard examination, but it is similar to changing transducers during ultrasonography to look at deeper or more superficial structures. In a small or remote radiology practice, the attending radiologist may not be available to supervise the MRI examination. In this situation, the patient can be called back for additional imaging with the surface coil. [58]
Several factors should be considered in optimizing the imaging protocols. Imaging in all 3 planes is useful; however, not every sequence must be performed in every plane. Fluid-sensitive sequences are mandatory for detecting subtle areas of edema. Typically, some T2-weighted sequence is performed, usually in the sagittal and axial planes. Experience with a particular sequence may outweigh any theoretical improvements from a pulse sequence unfamiliar to the imager. [59]
A repetition time (TR) between 2200 and 2800 ms is needed to generate enough sections to image both menisci in the sagittal plane. Short echo times (TEs) are important when PD–weighted imaging is performed. With a TE of less than 26 ms, more than 90% of all meniscal tears can be detected. If the TE is increased to greater than 60 ms, less than 30% of tears are detected. [59]
For reviewing MRIs of the knee, the use of meniscal windows has become popular. This method consists of a region of interest, centered on the meniscus, zoomed to 1.5-2X magnification. A window width of 100 to 150 and a window level of approximately 1000 are used. Data indicate no significant differences in detecting meniscal tears by using these narrow compared with conventional window widths. [59]
Sequences
T1-weighted images are not as sensitive as PD-weighted images for diagnosing meniscal tears. Gradient-recalled echo (GRE) sequences are as accurate as conventional spin-echo images for diagnosing meniscal tears. [20] However, GRE imaging is more limited in diagnosing ligament, muscle, tendon, bone marrow, and articular cartilage abnormalities. It is also less specific for meniscal tears as a consequence of spurious signal from artifacts or degeneration without a tear. [59]
Fat suppression can be applied to meniscal-sensitive sequences to rid the image of distracting high signal originating from the fatty marrow in the bones and the fat in the soft tissues. With fat suppression, the dynamic range signal of the menisci is increased, making meniscal tears more conspicuous. [4, 5] No evidence indicates that fat suppression increases the accuracy in diagnosing meniscal tears, but this practice is gaining widespread acceptance. [4, 5]
Turbo or fast spin-echo (FSE) pulse sequences are not as effective as conventional spin-echo sequences for diagnosing meniscal tears, because images with a short effective TE, as seen with FSE imaging, sacrifice high-spatial-frequency information for speed. Images of the menisci may appear blurred. Rubin and colleagues postulated that the presence of ghosting artifact (secondary to phase differences between even and odd echoes in the echo train) or the loss of meniscal signal intensity in meniscal tears from an increased magnetization transfer (as seen with FSE sequences) may be responsible for the lower sensitivity of this sequence. [18, 40, 60]
A review of 6 studies, including the author's, showed a distinct discrepancy between the sensitivities of FSE and conventional spin-echo sequences. The sensitivities of fast spin-echo techniques for detecting a meniscal tear was approximately 80%, whereas the sensitivities for conventional spin-echo sequences averaged approximately 90%. The authors postulated that abnormal meniscal signal may appear to extend to the meniscal surface secondary to blurring and may be incorrectly interpreted as a tear.
Alternatively, the increased blurring and decreased resolution associated with FSE imaging can contribute to false negative results. Blurring is most evident with short TE sequences, but short TE sequences are most proficient for detecting meniscal abnormalities. Blurring is also most conspicuous with long echo-train lengths, such as those incorporated with FSE imaging protocols. The authors urged abandoning FSE imaging because a loss of greater than 10% in sensitivity is unacceptable. [36]
When FSE sequences are used, an echo train length of 4-6 should be used to reduce blurring. The sensitivity of FSE sequences for diagnosing meniscal tears is about 80% in all reports, whereas the sensitivity of conventional spin-echo techniques is at least 90%. If the sensitivity decreases from over 90% to 80% and if all that is gained is 2-3 minutes in imaging time, the use of FSE sequences for imaging the menisci is hardly justified. [4, 5, 61]
The use of FSE sequences with high performance gradients is accurate as conventional spin-echo imaging in diagnosing meniscal tears. The following parameters are used: a TR of 1500 ms and an effective TE of 20 m, with K space centered on the second echo at 2X minimal interecho spacing and a length of 4. [61]
Grading system for meniscal degeneration
An MRI grading system has been developed and correlated with a histologic model. Regions of degeneration show increased signal intensity in a spectrum of patterns or grades based on the distribution (morphology) of signal intensity relative to an articular surface of the meniscus. This basis is exclusive of the peripheral capsular margin of the meniscus, which is considered nonarticular. [40]
Grade 1
Grade 1 is a nonarticular, focal or diffuse region of increased signal intensity within the substance of the meniscus (see the image below). This finding is correlated with early meniscal degeneration and chondrocyte-deficient or hypocellular region. The terms mucinous, myxoid, and hyaline degeneration are used interchangeably to describe the production and accumulation of an increased amount of mucopolysaccharide ground substance in stressed areas of the fibrocartilage of the meniscus. Such changes are a response to repetitive mechanical loading.
 Sagittal fat-saturated proton density–weighted image of the lateral compartment shows the relative equal size of the anterior and posterior horns of the lateral meniscus. The meniscal body has the normal configuration of a bow tie.
Sagittal fat-saturated proton density–weighted image of the lateral compartment shows the relative equal size of the anterior and posterior horns of the lateral meniscus. The meniscal body has the normal configuration of a bow tie.
This appearance is found in healthy volunteers and asymptomatic athletes and is not clinically significant.
Grade 2
Grade 2 is a horizontal, linear area of increased signal intensity within the substance of the meniscus that extends to, but does not involve, the inferior surface (see the image below). Such regions of abnormal signal are more extensive than in grade 1 degeneration, and no distinct cleavage plane or tear is present. Grade 2 is a continuation of progressive degeneration from grade 1 changes. Patients are usually asymptomatic.
 Sagittal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus, which appears to extend close to the inferior surface. This represents grade 2C changes in signal intensity. It can be difficult to differentiate grade 2 and grade 3 changes. Injuries causing grade 2C signal intensity can progress to degenerative tears.
Sagittal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus, which appears to extend close to the inferior surface. This represents grade 2C changes in signal intensity. It can be difficult to differentiate grade 2 and grade 3 changes. Injuries causing grade 2C signal intensity can progress to degenerative tears.
Grade 2 signal may be of 3 types. [62] Type 2A is a linear signal not in contact with an articular surface. Grade 2B is abnormal signal in contact with an articular surface on only a single image. Grade 2C is an extensive wedged-shaped signal abnormality not in contact with an articular surface.
Histologically, there is microscopic collagen fragmentation and clefting within the hypercellular region of the fibrocartilaginous matrix. The middle perforating collagen bundle, which divides the meniscus into superior and inferior halves, is the site of preferential accumulation of mucinous ground substance. It also represents the shear plane of the meniscus and is also the site of origin of horizontal degenerative meniscal tears.
The posterior horn of the MM is the most common location. It also is the most common site for grade 3 meniscal tears. The presence of grade 2 signal-intensity changes is not predictive of future progression to grade 3 meniscal tears. Grade 2 represents a point of potential structured weakening. Grade 3 tears, when they develop, are adjacent to, or are in continuity with, areas of grade 2 changes.
Grade 2C is a subcategory in which linear signal intensity extends to the articular surface on a single image. When found in symptomatic patients, about 50% have a tear. There are no additional features that can discriminate a torn meniscus from an intact meniscus with grade 2C signal intensity.
This is not a very common occurrence, appearing in only 3% of patients in one study. Most patients with grade 2C signal are not treated with arthroscopy because they do not have symptoms referable to the site of abnormality, but about 50% of patients with grade 2C signal and knee symptoms have meniscal tears. Grade 2C signal might represent more extensive degeneration than seen with grade 2 signal and can progress to degenerative tears. [63]
Grade 3
Grade 3 is a region of abnormal signal intensity within the meniscus extending to and communicating with at least 1 articular surface of the meniscus. Multiple foci of grade 3 signal-intensity changes may be present in 1 meniscus.
About 5% of grade 3 tears are actually intrasubstance cleavage tears. These are closed meniscal tears and diagnosed only with surgical probing of the meniscus. They may be missed on routine arthroscopy if surface extension is not identified. [34]
False-negative correlations with arthroscopy have been described. This commonly occurs in the LM, either peripheral or posterior when an associated ACL tear is present. [64] The improved spatial resolution and signal-to-noise ratio achieved with a surface coil may improve diagnostic accuracy in this situation and be related to spurious interpretation of areas of fraying as meniscal tears. Such lesions may present with pain related to edema and ingrowth of the synovium within the tear because the meniscus is an enervated structure. [30, 58]
Criteria for meniscal tears
Two MRI criteria have been established for diagnosing meniscal tears. If prior surgery has not been performed on the meniscus, the accuracy in diagnosing tears is 90%. [1]
Criterion 1
Criterion 1 is increased internal signal intensity in the meniscus. An article discussed the concept of the "Two-Slice-Touch Rule." The authors described a positive predictive value of 94% for meniscal tears for the medial meniscus and 96% for the lateral meniscus when the tear is present on 2 consecutive images. The positive predictive value was 55% and 36% for medial and lateral meniscal tears, respectively, when seen on only 1 slice. [1, 30, 65]
The abnormal signal intensity must be in contact with 1 articular surface, either the superior or interior surface or at the tip (free edge) of the meniscus. If the contact with the articular surface appears on 2 or more consecutive images, the accuracy of the diagnosis of meniscal tear increases. [1, 34]
The need for short TEs is important. Most other tissue disorders are characterized by an increase in free water and unbound protons. In meniscal tears, hydrogen nuclei are bound to macromolecules. The bound protons have a shorter T2 relaxation than do protons in free water. Meniscal tears also result in the absorption of synovial fluid in the margins of the tear. This may be related to the loss of the normal tight collagen spiral, resulting in an increased mobility of water molecules. Water molecules are trapped, increasing the local spin density. The increased meniscal signal within the tear probably results from an increase in the local spin density and not from an increase in the T2 signal. [1]
The rate of proton rotation is shortened by the interaction of synovial fluid and large macromolecules, resulting in shortening of T1 and T2 values, increasing the sensitivity of PD-weighted images in revealing meniscal pathology. Such changes cause a local increase in the degree of freedom of trapped water molecules, resulting in increased T2 times, allowing the detection of increased signal with short-TE sequences. Increased signal within the meniscus is best seen on short-TE images obtained by using PD-weighted or GRE sequences. [34]
Although most meniscal tears are seen well on PD-weighted images, they are not visualized as well on T2-weighted images, unless there is a wide cleft at the site of the meniscal tear that freely communicates with joint fluid. If such a situation is present, confidence in diagnosing a meniscal tear is high. However, this finding is not common.
Criterion 2
Criterion 2 is an abnormal meniscal shape. Comprehensive knowledge of the normal MRI anatomy of the menisci is required. Meniscal tears are more confidently diagnosed when they are seen on both sagittal and coronal images. The presence of a meniscal tear on both these views decreases the rate of false-positive diagnoses. However, some tears at the meniscocapsular junction can be seen only on 1 of these views.
In writing the MRI report about a meniscal tear, the radiologist should understand the use of standard nomenclature for meniscal tears and describe the location, plane, shape, completeness, length, and number of tears. [59]
Sizes, shapes, and patterns
Multiple cross-sectional representations of a meniscal tear have to be translated into a 3-dimensional (3D) description for the benefit of the arthroscopist. [1, 22]
Meniscal tears occur in 2 primary planes: vertical and horizontal. The 3 basic meniscal tear shapes are longitudinal, radial, and horizontal. Meniscal tears are either partial thickness or full thickness.
Vertical tears are aligned perpendicular to the coronal plane of the meniscus and can be subdivided into longitudinal and radial tears. They occur as traumatic lesions in younger patients. [66] A full-thickness vertical tear contacts both the superior and inferior articular meniscal surfaces, completely dividing the torn part of the meniscus into an inner and outer portion. Such tears can lead to the development of bucket-handle tears. [18, 67]
Longitudinal tears separate the meniscus into inner and outer fragments and occur parallel to the outer margin of the meniscus (perpendicular to the tibial plateau and propagate parallel to the circumferential axis of the meniscus). These tears are equidistant from the outer (peripheral) meniscal margin throughout their entire course.
Longitudinal tears are more commonly traumatic in etiology and occur in younger and more physically active patients. They are also commonly found in patients who have also acutely torn their ACL. Such meniscal tears are located in the posterior horn of the LM, central to the popliteus tendon. [18] In addition, these tears do not involve the free-edge (the inner part) of the meniscus on any image. They are often located in the middle or outer third of the meniscus and usually begin in the posterior horn. [1] A partial-thickness longitudinal tear contacts only the superior or inferior articular meniscal surface, but not both.
Short tears, or those confined to the posterior horn, may be visible only on sagittal images. Longer tears propagate into the body of the meniscus. These are seen on both sagittal and coronal images.
Bucket-handle tears
Bucket-handle tears are displaced vertical longitudinal tears and usually involve the MM (see the images below). The separated central (inner) fragment, when viewed axially, resembles the handle of a bucket. The remaining larger peripheral portion of the meniscus resembles the bucket. These tears account for about 10% of all meniscal tears. [4, 5, 59, 68]
 Coronal proton density–weighted image shows a full-thickness, vertical bucket handle tear (arrow) through the base of the medial meniscus (MM).
Coronal proton density–weighted image shows a full-thickness, vertical bucket handle tear (arrow) through the base of the medial meniscus (MM).
 Sagittal proton density–weighted image shows a vertical bucket handle tear (arrow) through the periphery of the posterior horn of the medial meniscus (MM). Tears in this location do not usually heal spontaneously because this portion of the meniscus lacks blood supply.
Sagittal proton density–weighted image shows a vertical bucket handle tear (arrow) through the periphery of the posterior horn of the medial meniscus (MM). Tears in this location do not usually heal spontaneously because this portion of the meniscus lacks blood supply.
The central fragment is often well visualized on coronal images and poorly visualized on sagittal images. Central fragments of bucket-handle tears of the posterior horn of the LM are often displaced anteriorly, so that the torn and displaced fragment lies on top of the anterior horn of the LM. This occurs because the ACL prevents the meniscal fragment from completely migrating into the intercondylar notch. In this situation, the "height" of the anterior horn of the LM is almost twice its normal height. This is best seen on sagittal views. [34]
An absent bow-tie sign is helpful for diagnosis of bucket-handle tears of the meniscal body (see the image below). The normal body of the meniscus is 9-12 mm in width and should be seen on 2 consecutive sagittal images and, as described in normal MRI anatomy, has the shape of a bow tie. When a bucket-handle tear is present, part of the free edge of the meniscus is missing. The inner portion of the meniscal body will be absent. Confirmation almost always occurs in the form of a displaced meniscal fragment that is visualized elsewhere in the knee joint.
 Sagittal proton density-weighted image of the outer portion of the lateral side of the knee shows an absence of the body of the lateral meniscus (LM, arrow). The body of the meniscus should be visualized peripherally. The normal appearance of the meniscus has the appearance of a bow tie; the bow tie is absent here.
Sagittal proton density-weighted image of the outer portion of the lateral side of the knee shows an absence of the body of the lateral meniscus (LM, arrow). The body of the meniscus should be visualized peripherally. The normal appearance of the meniscus has the appearance of a bow tie; the bow tie is absent here.
When no displaced fragments are found, an absent bow-tie sign may be related to a normal but small meniscus. In this situation, both the medial and LM are small; bucket-handle tears of both the medial and LM, occurring at the same time, are rare. Another cause of an absent bow-tie sign is a normal postoperative meniscus in patients who have undergone PM.
These injuries may be further classified as single, vertical longitudinal tears, displaced bucket-handle tears, broken bucket-handle tears, and double and triple vertical longitudinal bucket-handle tears. They are 3 times more frequent in the MM than in the LM and may be associated with ACL tears. Bucket-handle tears are commonly seen in young adults with a history of locking, extension block, or slipping of the joint due to displacement of the central fragment toward the intercondylar notch.
Radial tears (transverse tears)
Radial tears are vertical tears and propagate perpendicular to the main axis of the meniscus. These injuries are devastating because a full-thickness tear destroys meniscal integrity (ie, the ability of the meniscus to distribute hoop stress; hoop stress is the normal outward force generated in the meniscus in all directions as a result of weight bearing).
The force is distributed in the meniscus by collagen fibers, located around the circumference of the meniscus from apex to periphery. The collagen preserves the normal shape and integrity of the meniscus in weight bearing. Radial tears transect these fibers. The meniscus is normally attached to the tibia at the anterior and posterior ends.
During weight bearing, the meniscocapsular attachments pull the meniscus outward. A radial tear occurring between the tibial attachment points causes the free, unattached edges of the meniscus at the point of the tear to temporarily pull outward, expanding the width of the tear, exposing a bare spot on the adjacent tibia and femur, allowing abnormal stresses on the unprotected articular cartilage and bony surfaces, and resulting in articular cartilage destruction and subsequent bone alteration, leading to accelerated degenerative disease.
A complete radial tear extends all the way through the meniscus from the apex to the periphery. When it involves the meniscal body, the meniscus is split into an anterior and posterior fragment. The middle third of the LM is a common location. This injury begins at the free edge (inner margin) and extends a variable distance toward the periphery. [18]
Small tears may be difficult to recognize on MRIs. Missed radial tears constitute a large proportion of errors made in image interpretation of meniscal pathology. The key feature of recognition is that they involve the free edge of the meniscus. Thus, the inner point of the meniscal triangle is absent or blunted on 1 or more images. Radial tears of the meniscal body are best seen on sagittal images. They disrupt the normal bow-tie configuration of the meniscus on 1 or more images.
Like longitudinal tears, radial tears are commonly traumatic and occur in younger, more physically active patients. Tears in the MM usually occur in the posterior horn and are more common in older patients. Small tears of 3 mm or less may be asymptomatic.
Tears located near the posterior horn of the LM are associated with ACL tears. [64] They may be associated with more complex meniscal tears, such as vertical longitudinal tears or peripheral horizontal cleavage tears. They are devastating because the circumferential fibers are disrupted. The meniscus is prevented from developing the necessary hoop stress that normally helps dissipate forces across the knee. It is common to see a radial tear as one component of a complex tear.
Oblique (parrot beak) tears or flap tears are a form of radial tears. They begin at the free (inner) edge, like other radial tears, but then curve into a longitudinal orientation, similar to longitudinal meniscal tears, as the tear extends toward the meniscal periphery. As the tear is traced on sequential images, it moves closer to the outer portion of the meniscus and then remains equidistant from the outer meniscal margin on subsequent images, as seen on longitudinal tears. Oblique tears are the most common meniscal tears. [1, 22, 40]
A high prevalence of radial tears is present in postoperative patients who have had partial meniscectomy. Magee et al indicated a 32% prevalence when viewing 100 postoperative MRIs. This may be related to altered biomechanics of knee function after partial meniscus removal. Stresses may be redistributed that predispose to radial tears. [52]
Horizontal tears
Horizontal tears are also called cleavage or fish-mouth tears. They divide the meniscal tear into a top (superior) portion and a bottom (inferior) portion. They usually begin on the undersurface of the meniscus. [18]
Although horizontal tears may appear to extend deep into the meniscal substance on MRIs, the tears, as seen at arthroscopy, may extend only a few millimeters into the meniscus from the point where the abnormal signal contacts the meniscal surface. When it extends to the periphery of the meniscus, the cleft between the fragments can allow the egress of joint fluid to the meniscosynovial border, where it may become trapped, forming a meniscal cyst. Most are degenerative, occurring in older patients with osteoarthritis.
Miscellaneous tears
Other tear shapes may be thought of as combinations of longitudinal, radial, and horizontal tears. Multiple tears can present simultaneously in a meniscus, involving different portions of or the same region. A single meniscal tear, containing a combination of longitudinal, radial, or horizontal cleavage planes, is called a complex tear (see the image below). A common type of complex tear is composed of horizontal and radial components. Nearly all of these tears are degenerative in origin. [1, 22]
 Sagittal proton density–weighted image of the mid portion of the medial compartment shows a full-thickness horizontal tear of the posterior horn of the medial meniscus extending from the base to the superior surface. In addition, image shows amputation of the inferior apex of the posterior horn. The combination of these 2 tears involving the same part of the meniscus makes this injury a complex tear.
Sagittal proton density–weighted image of the mid portion of the medial compartment shows a full-thickness horizontal tear of the posterior horn of the medial meniscus extending from the base to the superior surface. In addition, image shows amputation of the inferior apex of the posterior horn. The combination of these 2 tears involving the same part of the meniscus makes this injury a complex tear.
Fraying or fibrillation of the free edge of the meniscus is seen as an area of increased signal intensity at the apex of a normally shaped meniscus. If abnormal morphology (truncation and foreshortening) is present, a tear is likely. Fraying can occur anywhere along the meniscal surface (see the image below). [40]
 Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
Indirect signs of an LM tear include an abnormal or absent superior popliteal-meniscal fascicle, and the presence of pericapsular edema posterolaterally is associated with a tear to the posterior horn of the LM. However, caution is needed in this setting. Johnson and De Smet reported that the superior popliteal-meniscal fascicle was not seen in 2 of 66 patients with intact menisci. De Smet and Asinger showed that 2 of 13 patients with posterior pericapsular edema did not have LM tears. [30, 69]
Meniscal avulsion
The tibial plateau articular cartilage normally completely covers the posterior horn of the menisci. If fluid is located beneath the meniscus, especially the posterior horn, detachment should be considered. This is called a floating meniscus. These menisci are usually intact without evidence of a tear. Arthroscopy requires infusion of saline into the joint. This may relocate a displaced but otherwise normal meniscus into normal alignment. It is imperative that the orthopedist be alerted to the presence of this entity to avoid the pitfall of misdiagnosis.
Displaced meniscal fragments
Displaced meniscal fragments occur in 9-24% of meniscal tears. Any shape of a meniscal tear can result in a displaced fragment (see the images below). [70] MRI diagnosis depends on visualizing the torn, deficient meniscus or the displaced inner meniscal component. [4] Displaced meniscal fragments are often clinically significant lesions requiring surgery because of pain and knee locking. [71]
 Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
 Sagittal fat-saturated proton density-weighted image shows a well-defined, soft tissue density in front of the posterior cruciate ligament (PCL). It is speckled and looks like the normal posterior medial horn of the medial meniscus (MM), but it is in the wrong place. This finding represents a displaced meniscal tear involving the posterior medial horn. The position of the meniscus is referred to as a double PCL because it looks like 2 of these ligaments are present.
Sagittal fat-saturated proton density-weighted image shows a well-defined, soft tissue density in front of the posterior cruciate ligament (PCL). It is speckled and looks like the normal posterior medial horn of the medial meniscus (MM), but it is in the wrong place. This finding represents a displaced meniscal tear involving the posterior medial horn. The position of the meniscus is referred to as a double PCL because it looks like 2 of these ligaments are present.
 Coronal fat-saturated proton density-weighted image shows speckled displaced meniscal fragment (inner arrows). Also present is an extensive horizontal tear to the body of the medial meniscus (MM) with a lot of hyperintensity at the periphery (outer arrows). This represents a meniscal cyst. Repair of the cyst without repair of the underlying meniscal tear results in recurrence of the cyst.
Coronal fat-saturated proton density-weighted image shows speckled displaced meniscal fragment (inner arrows). Also present is an extensive horizontal tear to the body of the medial meniscus (MM) with a lot of hyperintensity at the periphery (outer arrows). This represents a meniscal cyst. Repair of the cyst without repair of the underlying meniscal tear results in recurrence of the cyst.
Bucket-handle tears are the most common pattern, occurring in 10% of meniscal tears. They result from vertical, longitudinal, or oblique tears. These tears often involve the entire meniscus but isolated tears of the anterior horn, posterior horn, or (more commonly) the posterior horn and body.
The most reliable sign is visualization of the displaced fragment. Typical locations of the displaced fragment include the intercondylar notch anterior and parallel to the posterior cruciate ligament, or PCL (double PCL sign), and ventrally or horizontally juxtaposed to the anterior horn. An absent bow-tie sign indicates the meniscal body is absent. Any meniscal segment, however, can be involved. [5]
A flap tear is a short-segment horizontal meniscal tear with either superior or inferior displacement of the meniscal fragment. This type is less frequent; superior displacement is more common.
Horizontal tears become displaced either by the top or bottom portion flipping over to lie above or below the remainder of the meniscus or by sliding toward the inner part of the knee. These tears usually involve the MM. [70]
Inferomedial displaced tears from the MM are uncommon. When the displaced fragment extends inferior and medial to the tibial plateau, deep to the MCL, it may go unnoticed by the arthroscopist because the meniscus surface may appear intact.
Inward displacement of the free edge of an oblique tear results in a displaced parrot-beak tear and can precipitate mechanical symptoms, such as locking, catching, and giving way. Displaced fragments can prevent closed reductions of knee dislocations. The fragment can completely separate from the rest of the meniscus to become a free fragment. [66]
A meniscal body appearing unusually small should prompt a careful search for a displaced fragment. [4]
Several signs may be present in the same patient. [72] An absent bow-tie sign may be identified on sagittal images and represents a torn meniscal body segment. When present, it is indicative of a free meniscal fragment in 97% of patients. [4, 72]
Bucket-handle tears with centrally displaced fragments into the intercondylar notch may also be present. A double-PCL sign is seen in 39% of patients, and the notch-fragment sign is seen in 51% of patients. In this setting, the fragment is adjacent to but not at the same level as the PCL on sagittal images. The fragment is slightly more medial in location. It originates from the MM. A disproportionate posterior horn sign is seen in 21% of patients. A larger central portion of the posterior meniscus, when compared with the smaller periphery of the same posterior meniscus, indicates a displaced meniscal fragment. The meniscal tear usually originates from the anterior horn. [72]
Bucket-handle tears with an anteriorly displaced meniscal fragment can be observed. The flipped-meniscus sign is seen in 63% of patients. The criterion is a tear or nonvisualization of the posterior meniscus with the maximum height of the anterior horn of the involved meniscus greater than 8 mm. [61, 72]
 Sagittal fat-saturated proton density–weighted image shows soft tissue (arrows) lying on top of the anterior horn of the medial meniscus (MM), separated from it by high signal intensity (bright joint fluid). This finding represents a displaced meniscal fragment. The posterior horn of the MM is abnormally shaped and has abnormal signal intensity. This is the origin of the displaced fragment. The height of the combination of the displaced fragment and the anterior meniscus is greater than 8 mm. The height of the meniscal tissue equal to or greater than this number is a good sign of a displaced meniscal fragment.
Sagittal fat-saturated proton density–weighted image shows soft tissue (arrows) lying on top of the anterior horn of the medial meniscus (MM), separated from it by high signal intensity (bright joint fluid). This finding represents a displaced meniscal fragment. The posterior horn of the MM is abnormally shaped and has abnormal signal intensity. This is the origin of the displaced fragment. The height of the combination of the displaced fragment and the anterior meniscus is greater than 8 mm. The height of the meniscal tissue equal to or greater than this number is a good sign of a displaced meniscal fragment.
Pseudohypertrophy of the anterior horn of a meniscus occurs when an anterior meniscal horn appears abnormally large. The meniscal body or posterior horn is unusually small. This indicates a portion of the torn body or posterior horn has flipped anteriorly and lies behind the anterior horn. The abnormal meniscal fragment and the adjacent normal meniscus are separated by joint fluid, which has increased signal intensity on T2-weighted images.
The differential diagnosis includes the following: ligament of Humphry, loose bodies, osteophytes, and fracture fragments.
Stable versus unstable tears
The stability of tears is determined by a number of factors, including the length, location, and completeness of the tear. Probing the meniscal tear during arthroscopy is critical for determining stability.
A stable vertical longitudinal tear occurs when the central (inner) fragment of a meniscal tear cannot be displaced more than 3 mm from the intact meniscal periphery. Any meniscal tear with a displaced fragment is unstable.
Longitudinal tears that are relatively long are unstable; their length is assessed on multiple 3- to 4-mm sections in either plane, and they extend through the full thickness of the meniscus or contain fluid on T2-weighted images.
Some meniscal tears do not show a free fragment at the time of MRI. However, it is considered an unstable tear whenever the inner margin of the tear can be displaced to a position where it can be entrapped between the rotating femur and tibia when probed at arthroscopy.
Meniscal contusion
Meniscal contusion occurs when the meniscus gets trapped between the tibia and femur, usually as a result of trauma. A contused meniscus demonstrates increased signal within its substance that might resemble a tear. The signal is in contact with an articular surface but is less discrete than the abnormal signal seen with tears—indistinct and amorphous, rather than the sharp and discreet signal seen in a tear. It is less well defined than the signal seen with meniscal degeneration. Often, there is an adjacent bone contusion. [4, 62]
The cause of the abnormal signal might be related to blood products from a compressive injury to the vascular zone of the meniscus that track along the meniscal fibers, resulting in increased signal.
Meniscocapsular separation
Meniscocapsular separation (MCS) is a tear of the periphery of the meniscus at the meniscosynovial junction. The attachment of the MM is more commonly involved due to its firmer contact with the joint capsule. The site more frequently involved is the capsular attachment of the posterior horn of the MM at the tibia, at the meniscotibial (coronary) ligament. MCS is frequently associated with ligamentous injuries about the knee. They rarely propagate into the meniscal periphery, though they can be an extension of a full-thickness tear.
An abnormal superior meniscal fascicle is highly associated with a lateral meniscal tear, but the LM can rarely be normal in this setting. Such a finding should intensify the evaluation of the LM for possible tears. The presence of posterior pericapsular edema is another indirect, but nonspecific, sign that when coupled with an abnormal superior popliteal meniscal fascicle should alert the imager to the possibility of a lateral meniscal tear. [30, 73]
MCS of the LM can occur at the superior or inferior popliteal-meniscal fascicle adjacent to the popliteus tendon. Disruption of the fascicular attachments between the popliteus tendon and the LM can result in gross instability and is associated with a tear of the posterior horn of the LM. [30]
Spontaneous healing is common because of the rich blood supply in the meniscal periphery.
MRI findings include an increased distance between the periphery of the meniscus and the tibia and fluid between the MCL and the medical meniscus. [74]
Meniscal cysts
Meniscal cysts occur more frequently in the medial compartment than elsewhere because meniscal tears are more common in the MM. This observation contrasts with previous reports, indicating that they are more common in the lateral compartment. There are 3 reasons for this discrepancy [75] :
-
First, reports indicating a lateral compartment preference were written before the use of MRI. MRI is more sensitive than PE in the detection of small meniscal cysts. There is a relatively scant amount of fatty soft tissue on the lateral aspect of the knee as compared to the medial aspect. This may explain why more lateral cysts were reported, because in that region, cysts are more apt to appear as a palpable mass.
-
Second, other diagnostic methods, such as knee arthrography, lead to underestimations of the true incidence of meniscal cysts. Diagnosing meniscal cysts with arthrography requires the extravasation of contrast material through the meniscal tear and cyst, but this does not always happen.
-
Third, meniscal cysts are occasionally overlooked at arthroscopy because visualization of the posterior horn of the MM can be difficult. Thus, cysts in the posterior medial compartment were underdiagnosed.
Medial parameniscal cysts are more symptomatic that other conditions because of their location adjacent to the MCL. The incidence is between 1-2% and 7-8%, and these cysts most commonly occur in men aged 20-40 years. Medial meniscal cysts are most commonly adjacent to the posterior horn. [18]
LM cysts are most commonly located adjacent to the anterior horn or body. MM cysts are twice as common as LM cysts, and MM tears are twice as common as LM tears. The tears are most commonly formed when horizontal tears extend to the meniscal periphery, allowing joint fluid to escape into the parameniscal soft tissue. The fluid subsequently encapsulates and becomes symptomatic due to mass effect. Occasionally, the cyst can be confined to the meniscus. This is referred to as an intrameniscal cyst.
Parameniscal cysts located adjacent to the anterior horn of the lateral meniscus are less likely to have an underlying meniscal tear than cysts in other meniscal locations. [76]
It is important to recognize the association between meniscal cysts and meniscal tears. If the cyst is resected without addressing the tear, the cyst may recur.
The MRI appearance is a fluid-filled region adjacent to a horizontal meniscal tear.
Meniscal ossicles
Meniscal ossicles are rare and often mistaken for intra-articular loose bodies.
These appear as circumscribed ossification with fatty bone marrow in the center. The fatty marrow helps distinguish this entity from intra-articular loose bodies. Meniscal ossicles are usually located in the posterior horn of the MM. [77] They may be symptomatic because of mass effect or an associated meniscal tear. [78]
Chondrocalcinosis
Chondrocalcinosis is calcification of the menisci, synovium, and/or articular cartilage due to the deposition of calcium pyrophosphate dihydrate crystals, dicalcium phosphate dihydrate, calcium hydroxyapatite, or any combination of these crystals. It is seen in conditions such as gout, degenerative disease, hemochromatosis, crystal deposition disease, and hypercalcemia. These intra-articular crystals are weakly positive fringent monourate crystals under polarized light.
The prevalence is 5-14% and increases with age. A multitude of conditions and mechanisms are implicated in the pathogenesis.
Intrameniscal calcium can demonstrate increased signal intensity, which can mimic a meniscal tear on T1-weighted, intermediate PD-weighted, or T2-weighted images. Correlation with plain radiographs, especially in patients with the associated conditions, reduces the incidence of error. [18]
Meniscal extrusion
Meniscal tears eliminate the hoop stress of the meniscus. Sustained compressive forces within the knee can cause displacement or extrusion.
Meniscal extrusion has been reported in older patients with symptomatic knee osteoarthritis. In this group, meniscal extrusion preceded the development of degenerative joint disease. Laxity of the soft tissue attachments, meniscal tears, and degenerative changes within the meniscus have all been implicated as predisposing conditions. [79]
After meniscal extrusion, the unimpaired impaction of cartilage leads to osteoarthritis.
Other factors contributing to meniscal extrusion include tibial femoral cartilage damage and knee malalignment. Malalignment could increase the load transmitted to the meniscus, which could lead to extrusion. Varus and valgus angulation are associated with medial and lateral meniscal extrusion, respectively. [79]
Indirect signs of meniscal tears
Indirect signs of meniscal tears include meniscal and parameniscal cysts, joint effusion, medial collateral ligament edema, and bone marrow edema. Bone marrow edema can be 1 of 3 types: (1) perivascular edema occurs around vascular channels and does not extend to the joint surface, (2) linear subchondral marrow edema occurs adjacent to the meniscus and probably reflects hyperemia and increased fluid at the cortical-chondral-meniscal interface, and (3) nonlinear subchondral marrow edema is associated with abnormalities at the adjacent cartilage surface. The presence of this type of edema reflects cartilage loss, chronicity, and extent of meniscal tear. [80]
Ramp lesions
Ramp lesions can be characterized as tears that occur at the posterior meniscocapsular junction. In various studies, incidence of ramp lesions has ranged from 9 to 40%, with chronic ACL injury being a significant risk factor. [29, 81, 82, 83, 84, 85, 86] According to Seil et al, ramp lesions may be expected in about 25% of patients undergoing ACL reconstruction, especially in cases of contact injuries in the presence of complete ACL tears. [85]
Diagnostic Accuracy
Isolated meniscal tears
When only prospective, double-blind studies of at least 200 menisci are considered, the sensitivity for detecting medial meniscal (MM) tears is 86-96%, with a specificity of 84-94%. For lateral meniscus (LM) tears, the sensitivity decreases to 68-86%, and the specificity is 92-98%. The NPV is 91%, indicating that if a properly obtained MRI of the knee does not show a meniscal tear and if the patient's symptoms necessitate surgery, the likelihood of finding a meniscal tear at arthroscopy is less than 10%. [20, 30, 34, 87, 88, 89]
If the abnormal meniscal signal contacts the articular surface on a single section in a single imaging plane, the accuracy of diagnosing tears in the MM is 55%, and the accuracy for tears in the LM is 30%. The accuracy rate approaches 100% if the meniscal tear is seen on at least 2 consecutive images. [30]
Fast spin-echo (FSE) images are less sensitive than conventional spin-echo images for diagnosing meniscal tears, even when the imaging parameters are optimized. Two prospective studies in a large number of menisci examined with FSE imaging showed a sensitivity of 83% for meniscal tears; this is lower than most studies using conventional spin-echo techniques.
With 3D fast MRI, there is 95% concurrence between MRI and arthroscopy in detecting meniscal tears and 100% concurrence for detecting meniscal degeneration.
MRI is accurate for predicting repairable meniscal tears and sensitive for determining nonrepairable tears. One study showed 89% (103 of 116) of meniscal tears were categorized the same at MRI and arthroscopy with respect to repairable verus nonrepairable groups. The same study, however, showed that MRI had a variable accuracy for predicting meniscal tear configuration found at arthroscopy.
Errors in diagnosing meniscal tears can be classified as unavoidable (discordance between MRI and arthroscopy), equivocal (interobserver differences in interpretation), or interpretive (normal MRI variants mistaken for meniscal tears)
Accuracy for diagnosing meniscal tears in adolescents is similar to that in adults. One group found a 92% sensitivity and 87% specificity for the medial meniscus and a 93% sensitivity and 95% specificity for the LM. [90]
In a meta-analysis of the diagnostic accuracy of MRI for ACL and meniscal tears of the knee, sensitivity and specificity of MRI were 87% (95% CI 77-94%) and 93% (95% CI 91-96%), respectively, for ACL tears; 89% (95% CI 83-94%) and 88% (95% CI 82-93%), respectively, for medial meniscal tears; and 78% (95% CI 66-87%) and 95% (95% CI 91-97%), respectively, for lateral meniscal tears. [91]
False-negative errors in diagnosing LM tears
False-negative errors accounted for the largest number of errors in several studies and usually involve the body or posterior horn. The tears are usually small and stable and do not require PM or repair. They often go undiagnosed at arthroscopy unless the meniscus is probed or compressed. [34, 30, 87]
False-negative diagnoses outnumber false-positive diagnoses by about 3 to 1. False-negative tears of the posterior horn of the LM are associated with ACL tears. The reason may be related to the anatomy of the posterior horn of the LM. It has a shorter radius of curvature than the MM. The posterior horn is oriented obliquely upward. Such obliquity could result in volume averaging that could blur the connection of intrameniscal signal to the articular surface. Of these results, 40% were unavoidable, even when they were retrospectively evaluated. [34, 30, 87]
Characteristics of missed lateral meniscus tears are a longitudinal peripheral pattern with a vertical tear orientation. [92]
False-positive tears of the LM
Most of the findings involve vertical or horizontal degenerative tears in the posterior horn. There has been a gradual decrease in the number of false-positive diagnoses as a result of better recognition of normal anatomy and postsurgical variations and improved arthroscopic techniques.
The presence of either meniscal distortion or abnormal signal contacting the joint surface on only one view is not specific for a LM tear as confirmed by arthroscopy because healed tears can have an MR appearance similar to that of an acute tear. [73]
False-negative tears of the MM
Most of these results are in the outer half of the posterior horn or the inner third of the meniscal body. Two thirds of these tears are small, stable, and treated conservatively. Like the LM, most are not diagnosed directly at arthroscopy; rather, the diagnosis is made on the basis of the behavior of the meniscus to probing or compression.
Closed or confined intrasubstance tears may be misdiagnosed on MRI as grade 2 signal-intensity changes. These tears may also be missed at arthroscopy if the meniscal surface is not probed. This may contribute to a higher rate of false-negative diagnoses. [34, 30, 87]
False-positive tears of the MM
False-positive tears are more common than false-negative diagnoses of MM tears and almost always involve the posterior horn. [30, 34, 87]
Causes include (1) chondrocalcinosis in the meniscus mimicking a tear and (2) healed meniscal tears that often continue to show increased signal intensity that contacts a meniscal surface.
Regarding limitations in the criterion standard (ie, arthroscopy), most MM tears present on MRIs but are not identified at arthroscopy. These tears occur on the undersurface of the posterior horn. This location is an arthroscopic blind spot.
Although additional viewing portals and angled arthroscopies may be used, there are still some areas of the MM that cannot be visualized. False-positive findings include vertical, degenerative oblique, horizontal, and meniscocapsular tears. Justice and Quinn reported that 20% of false-positive tears were described as frayed on arthroscopy and not frankly torn, as seen on MRIs. [87]
Most false-positive MRI diagnoses of medial meniscus tears are apparent longitudinal tears of the posterior horn. [93]
Causes of false-positive MRIs
Causes of false-positive MRI results include the following:
-
Truncation artifacts
-
Vacuum-joint phenomenon
-
Magic-angle phenomenon
-
Increased conspicuity of intrameniscal signal intensity (grade 2 signal intensity) on GRE images
-
Misinterpretation of normal anatomic structures and anatomic variants
-
Errors related to previous meniscectomy
-
Errors related to misinterpreting changes after meniscal repair as evidence of a new tear
-
Tears missed on arthroscopy
-
Intra-articular loose bodies, which can obscure the meniscal margins and mimic a tear.
-
Intrameniscal signal intensity in patients with osteoarthritis who later went on to develop grade 3 signal-intensity abnormalities in the same region (the initial MRI changes are postulated to represent early separation of the meniscus and may be an early and symptomatic precursor of a horizontal cleavage tear)
Risk factors for false-negative MRI findings in cases of meniscal tear, according to one study, included short time from injury to MRI diagnosis, meniscal tear location within the posterior one-third, and peripheral longitudinal tear pattern. [94, 95]
Causes of variation between MRI and arthroscopy
Causes of variation between the accuracy rate of MRI and arthroscopy in diagnosing meniscal tears are varied.
Radiologists have different learning curves for interpreting knee MRIs, and arthroscopists have different levels of experience. Casscells has noted that "some surgeons learn arthroscopy slowly or not at all, and some are not very capable in this (diagnostic arthroscopy) respect." The accuracy of arthroscopy in diagnosing meniscal tears has been reported to be between 68-98%, depending on the experience of the examiner and the location of the tear. Nonetheless, surgeons generally regard arthroscopy as a standard of reference. [96]
Differences in descriptive terminology concerning meniscal damage are another factor. To one arthroscopist, a free-edge abnormality may be described as fraying and, to a radiologist, the same abnormality may be diagnosed as a small tear. Different types of MRI equipment, surface coils, and field strengths cause variability.
Arthroscopy may not detect intrasubstance degenerative cleavage tears. The medial femoral condyle might interfere with arthroscopic visualization of the posterior horn of the MM. The periphery of the meniscus at the meniscocapsular junction is difficult to image on MRIs. Most false-positive MRI findings occur in the posterior horns of both menisci. These regions are acknowledged to be the most difficult for arthroscopists to examine.
The validity of the assumption that arthroscopy is the most reliable method for assessing the outer third of the posterior horns and the inner third of the body of both menisci has been questioned. The inferior surface of the MM and, to a lesser extent, of the LM, cannot be routinely seen arthroscopically.
NPV of MRI for diagnosing meniscal tears
The negative predictive value (NPV) provides an estimate of the patient's likelihood of having no meniscal tear at arthroscopy when MRI indicates no tear. NPV is 100% for the MM and 91% for the LM. Because of the high NPV, a negative MRI can be useful to exclude patients from unnecessary arthroscopy.
Screening MRI can be performed in patients with clinically suspected knee injuries before a diagnostic arthroscopy is considered. If MRI results are normal, conservative treatment can be instituted. Arthroscopy can be reserved for patients with persistent symptoms in spite of treatment. [21]
The prevalence of meniscal tears in asymptomatic patients increases with age. One study showed an incidence of 13% in patients younger than 35 years and 36% in patients older than 45 years.
The sensitivity of MRI in detecting displaced meniscal tears depends on the size of the displaced meniscal fragment. When less than one third of the meniscus is torn, the displaced fragment will most likely not be seen on MRIs. Conversely, when the displaced fragment involves more than two thirds of the meniscus, it will be identified.
Regarding the accuracy of MRI of the menisci in adolescents, Major and Beard found a sensitivity and specificity of 92% for MM tears and a 93% sensitivity and 95% specificity for LM tears. [90]
Isointensity in the meniscus relative to fluid on T2-weighted MRIs, has a sensitivity of 60% and specificity of 92% for diagnosing new or recurrent meniscal tears. The accuracy of MR arthrography in diagnosing recurrent meniscal tears is 88%; that of routine MRI is 66%. The greater the amount of meniscus removed, the higher the accuracy of MR arthrography and the lower the accuracy of routine MRI.
In patients with minimal meniscal resection, the accuracy of both techniques was 89%. When only a small meniscal remnant is present, the accuracy of MR arthrography improved further to 100%, while that of routine MRI decreased to 50%. [97]
Regarding sensitivity, specificity, and accuracy for diagnosing meniscal tears in the presence of chondrocalcinosis, for the LM, sensitivity is 78%, specificity is 71%, and accuracy is 78%. For the MM, sensitivity is 89%, specificity is 72%, and accuracy is 81%. [98]
Using 4 criteria, VandeBerg reported sensitivities of 18-54% and specificities of 92-100% in diagnosing unstable meniscal tears. The criteria were the following: (1) presence of a displaced meniscal fragment, (2) visibility on more than 3 coronal sections of 3-mm thickness and 2 sagittal sections of 4-mm thickness, (3) more than 1 orientation plane or more than 1 pattern (contour irregularity, peripheral separation, or tear), and (4) intrameniscal high signal intensity on T2-weighted spin-echo images. [99]
Positive predictive values (PPVs) were 92-100%. NPVs ranged between 39% and 52%. Regarding bucket-handle tears, sensitivity has been reported as low as 44-64%. Sensitivity of the absent bow-tie sign has been reported to be as high as 97% and as low as 77%. [100]
For meniscal tears occurring with ACL tears, the accuracy of diagnosing meniscal tears with MRI decreases, but there is a greater decrease with clinical diagnosis. The sensitivity of MRI for diagnosing MM tears is between 84% and 88%. For the LM, it is between 68% and 83%. [30, 100]
Regarding reasons for decreased sensitivity with MRI, there is a different distribution of meniscal tears between knees with intact and torn ACLs. With ACL tears, meniscal tears are often in the periphery of the posterior horn of the LM. This is a difficult region to evaluate arthroscopically. Fortunately, meniscal tears in this region do not often require surgical treatment.
Finding a severe injury like an ACL tear may distract the radiologist from identifying more subtle, but equally important meniscal injuries. Subluxation of the knee from combined ligament tears may result in unusual anatomic appearance of the menisci, distorting their appearance, making recognition of meniscal tears more difficult. Patients with more severe injuries, such as concomitant ACL tears and meniscal tears, are less likely to remain motionless during MRI examinations because of pain. Patient motion results in poorer diagnostic images.
For meniscal tears with more severe ligamentous injuries, the accuracy is further decreased. One study showed that the sensitivity for diagnosing MM tears is 57% when 2 or more knee ligaments are torn. The sensitivity for diagnosing LM tears is 57%. With MCS, Rubin et al and Pfirrmann indicated that none of the MRI findings correlated with the arthroscopic results. The PPV for medial MCS was only 9%, and that for the lateral MCS was 13%. One reason is that many MCS injuries heal by the time arthroscopy is performed as a result of the rich vascularity of this region. Another reason is that such injuries may not be visible arthroscopically. Saw et al, however, found excellent correlation between MRI and arthroscopy. [1]
For DM tears, MRI does not have a high PPV for diagnosing meniscal tears (57%) when the standard criterion of abnormal meniscal shape is applied. However, Jung and colleagues reported that intra-meniscal signal change in symptomatic DM tears was an accurate predictor of arthroscopic tear. [37]
Regarding the predictability of MRI in determining meniscal tear reparability: MRI is only moderately reliable in predicting the reparability of a meniscal tear. Routine use of MRI for determining this is not indicated. Accuracy rates vary between 69% and 74%. The type of meniscal tear is an important parameter, affecting tear reparability. The accuracy of MRI in determining reparability according to tear type varies between 14% and 64% in the study by Mataya et al. The specificity in predicting reparability is between 74% and 97%. The sensitivity is 29%. The PPV is 50%, and the NPV is 80%. [23]
Concerning the predictability of MRI in determining meniscectomy, values are as follows: sensitivity, 68%; specificity, 75%; PPV, 90%; and NPV, 43%. The total false-positive rate for diagnosing meniscal tears is about 1.5%. The total false-negative rate for diagnosing meniscal tears is about 4.8%, which compares with a false-negative rate of 2-13% for arthrography and 5-10% for arthroscopy. The accuracy for MRI diagnosis of meniscal tears is nearly 90%. [101]
Pitfalls
Effect of echo time and the magic-angle phenomenon
Meniscal tears become less visible when echo time (TE) values are longer than 16-20 ms. Using TEs of shorter than 16 ms may result in increased signal within the normal meniscus. This signal intensity is not in contact with the meniscal surface. [18, 19, 24, 40, 77, 87, 102]
Short TEs needed for meniscal imaging may result in artificially increased signal intensity in the meniscus because of the magic-angle phenomenon. This is most common in the posterior medial horn of the LM where the main magnetic field (b0) is orientated along the head-to-foot axis of the patient (typical for most superconducting, high field-strength systems).
The normal posterior horn of the lateral meniscus (LM) slopes obliquely upward from lateral to medial, as it ascends from the lateral tibial plateau to its insertion on the posterior tibial eminence. On coronal images, it often achieves an angle of 55° relative to the long axis of the leg. This is the angle where the magic-angle phenomenon occurs when short TEs are used. This orientation leads to shortening of the apparent T1 relaxation time, resulting in an increase in signal intensity within the posterior horn, which may simulate a tear or grade 2 signal-intensity change.
This finding can be differentiated from true meniscal tears by increasing the TE; magic-angle findings disappear. True meniscal tears remain visualized. This finding can also be eliminated by imaging the knee in slight abduction, which alters the orientation of the posterior horn of the LM in relation to Bo.
Change in the normal shape of the meniscus
Any change in the normal meniscal shape, in the absence of prior surgery, indicates a tear, with 2 exceptions: (1) the DM, and (2) buckling of the MM producing a wavy appearance. This is similar to a phenomenon called meniscal flounce seen occasionally during arthroscopy. This last finding is normal.
Effects on GRE images
On GRE images, high signal intensity is present within the normal meniscus. Caution is needed to avoid using a window for which the images are too bright because this can lead to overdiagnosing the presence of meniscal tears. GRE images are vulnerable to susceptibility artifacts occurring in the vicinity of any ferromagnetic substance (microscopic metal shavings from prior surgery) or gas occurring during a normal vacuum phenomenon in the knee. [18, 19, 24, 40, 77, 87]
Mimics
Entities that may mimic meniscal tears include the origin of the meniscofemoral ligaments from the posterior horn of the LM, the popliteus tendon passing next to the posterior-lateral corner of the LM, and the attachment points of the intermeniscal ligament to the anterior meniscal horns. These errors can be avoided by following the anatomic structures on subsequent images.
The obliquely orientated meniscomeniscal ligament may be confused with a meniscal fragment in the intercondylar notch region. Careful attention to axial and coronal images will avoid this pitfall.
Structures of high signal intensity in the anterior root of the LM are caused by normal contributions of the root from the ACL. Such striations do not actually contact the meniscal surface and should not be confused with meniscal tears. [103]
Small radial tears may be difficult to diagnose; they may be seen in only 1 plane. Radial tears of the posterior meniscal roots can be overlooked. On sagittal images, distortion of the usual triangular shape of the posterior meniscus may be visible only on the image adjacent to the posterior cruciate ligament (PCL). A torn ACL, loose bodies, an intercondylar osteophyte, or prominent meniscofemoral ligament may mimic a displaced meniscal fragment. [104]
Regarding grade 2 versus grade 3 signal-intensity change in the meniscus, determining whether the signal intensity in the meniscus extends to the articular surface can be difficult. Evaluating for any change in the morphology of the meniscus at this site may be helpful. If the meniscus is distorted or abnormally shaped, the signal intensity is likely grade 3.
The transverse intermeniscal ligament and surrounding fat is another mimic. In 30% of cases, the fat surrounding the transverse intermeniscal ligament may mimic a meniscal tear. On sagittal images, the ligament crosses between the tibial attachment of the ACL and the Hoffa infrapatellar fat pad. Axial 3D Fourier-transformed sections of 1 mm or thinner may demonstrate the normal course of the ligament if a meniscal tear is still uncertain after standard MRI.
Tears of the anterior horn of the LM are rare. The central anterior ligamentous attachment of the anterior horn of the LM is rhomboid and normally directed upward on sagittal images. It frequently contains increased internal signal intensity. On serial sagittal images, the ligament may be traced from the anterior horn of the LM to the anterior horn of the MM.
A prominent vessel from the lateral geniculate artery rarely produces a pseudotear adjacent to the anterior horn of the LM. The lateral inferior geniculate artery, arising from the popliteal artery at the level of the knee joint, courses anteriorly around the lateral aspect of the knee and participates in the rich collateral circulation in this area. It is closely applied to the LM through its course. It lies within a region of periarticular fat between the meniscus and the LCL. When the artery lies adjacent to the anterior horn of the LM, it can appear as a tear on sagittal images. The artery can be traced on adjacent sagittal images so as not to be confused with a tear.
The junctional region between the posterior horn of the MM and the joint capsule contains peripheral vessels. The signal intensity here can mimic the appearance of a meniscocapsular detachment. Edema from MCS is more diffuse and ill defined. [105]
It may be difficult to differentiate between meniscal fraying and meniscal tearing.
The semimembranosus tendon can be mistaken for a displaced meniscus (see the image below).
 Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
The popliteus tendon sheath may be mistaken for a tear in the posterior horn of the LM. True tears of the periphery of the LM in this region usually have a different orientation than that of the tendon sheath. When in doubt, this structure can be traced on subsequent sagittal images and normalcy can be confirmed by using PD- and T2-weighted axial images.
A vertical tear of the posterior horn of the LM may, however, parallel the popliteus tendon sheath. Here, the popliteus tendon must be used as a landmark to find the peripheral edge of the meniscus.
After lateral meniscectomy, the low-signal popliteus tendon may be mistaken for a retained posterior horn meniscal remnant.
The normal concave edge of the periphery of the meniscus may demonstrate grade 2 signal on peripheral sagittal images through the body of the meniscus. This is more commonly seen in the MM and is caused by partial volume averaging of fat and the neurovascular structures in the soft tissues adjacent to the concavity of the meniscus. This is seen in up to 20% of MMs and 6% of LMs. Thin-section coronal images show a normal meniscus and its normal concave margin.
A speckled pattern of increased signal within the anterior horn of the LM near its central attachment on sagittal images is a normal finding. It represents the intimate relationship between the meniscus and the fibers of the ACL at its insertion. The medial most portion anterior horn of the MM may also exhibit this appearance. [104]
The meniscal insertion of the meniscofemoral ligament may mimic a vertical tear through the posterior horn of the LM. This appearance is caused by the interposition of fat between the ligament and its meniscal attachment. The fat signal intensity disappears on fat-suppressed images. This pseudotear extends obliquely from the superior meniscal surface and is directed posteroinferiorly toward the inferior meniscal surface. The pseudotear less commonly appears as a vertical line parallel with the meniscal periphery.
Distention of a bursa between the deep and superficial fibers of the MCL or distention of the deep portion of the semimembranosus MCL bursa can mimic fluid between the joint capsule and the meniscus. [18, 40, 19, 24, 77, 87]
Vacuum phenomena
Vacuum phenomena cause magnetic susceptibility artifacts. Intra-articular gas can normally occur when traction is applied to the joint. Gas, normally present in tissues, comes out of solution as a result of reduced pressure. This leads to magnetic susceptibility artifacts, which appear as low signal intensity on T1-weighted MRIs or as a blooming artifact on GRE images.
This gas may be mistaken for a meniscal tear. Gas collecting in the medial joint space between the articular cartilage of the femur and tibia can appear as a triangular signal void that simulates meniscal tears or an abnormal volume of meniscal tissue resembling a DM, or a displaced torn meniscal fragment.
Magnetic susceptibility is the ratio of the intensity of magnetization of the applied magnetic field. Bone, air, gas, and ferromagnetic materials have a susceptibility markedly different from that of soft tissue. Ferromagnetic materials have the greatest difference; bone, air, and gas have a lower difference.
Artifacts occur when there is a great and abrupt difference between the magnetic susceptibility of adjacent tissues. Such differences are caused by inhomogeneities in the magnetic field resulting from intrinsic magnetic field gradients generated in such a region. These gradients result in the misregistration of spatial information in the frequency encoding direction because pixel information is associated with the wrong frequency. The result is areas of artifactually high and low signal intensity.
These artifacts are also seen with GRE imaging because the spin dephasing is not fully refocused by means of gradient reversal techniques. They are worse with low readout gradients, as seen in a large field of view. The artifact is maximal when the region of varying susceptibility is perpendicular to the main magnetic field. [18, 40, 19, 24, 77, 87]
Truncation artifacts
Truncation artifacts are lines that traverse the menisci that can be confused with tears and are problematic when a 128 X 128 matrix is used with a 128 phase-encoded axis orientated in the superior to inferior direction.
Truncation artifacts result from the use of Fourier transformation methods used to construct MRIs of high-contrast boundaries, such as the interface between the articular cartilage and the meniscus. When an attempt to recreate the boundary is made, an inaccurate representation is produced. The image exhibits a series of overshoots and undershoots (a sine-integral function), occurring in alternate pixels as one moves away from the boundary. This appears as lines of increased or decreased signal intensity.
The size of the artifact is the difference between the degree of overshooting and undershooting. Such a line of high signal within the low signal of the meniscus may mimic a tear. One manifestation is the ringing artifact (Gibbs phenomenon), which occurs near highly contrasting interfaces.
These artifacts are subtle, uniform in thickness, and run parallel to the meniscal surface, 2 pixels away from the articular cartilage. The lines extend beyond the boundary of the meniscus and can be attenuated if the phase-encoded axis in a 128 X 256 matrix is orientated anterior to posterior instead of superior to inferior. Alternatively, they can be affected by data extrapolation algorithms or image filtering. The most effective way of diminishing the artifact is to use an acquisition matrix of 192 X 256 or 256 X 256. [18, 40, 19, 24, 77, 87]
Chondrocalcinosis
Calcification of the menisci and/or articular cartilage due to the deposition of calcium pyrophosphate dihydrate crystal, dicalcium phosphate dihydrate, calcium hydroxyapatite, or any combination of these substances (see the image below). Calcium pyrophosphate dihydrate crystal is the most common crystalline arthropathy. These intra-articular crystals are weakly positive birefringent monourate crystals under polarized light microscopy. [18, 40, 19, 24, 77, 87]
 Oblique radiograph of the right knee demonstrates bright triangular lines on either side of the joint. This finding represents calcium in the triangular menisci, which represents chondrocalcinosis. A globular calcium opacity (arrow) is above the periphery of the body of the lateral meniscus; this might represent a calcified loose body, either in the joint proper or in the popliteus recess. The presence of chondrocalcinosis can result in a false-positive diagnosis of a meniscal tear.
Oblique radiograph of the right knee demonstrates bright triangular lines on either side of the joint. This finding represents calcium in the triangular menisci, which represents chondrocalcinosis. A globular calcium opacity (arrow) is above the periphery of the body of the lateral meniscus; this might represent a calcified loose body, either in the joint proper or in the popliteus recess. The presence of chondrocalcinosis can result in a false-positive diagnosis of a meniscal tear.
The prevalence is 5-14% and increases with age. A multitude of conditions and mechanisms are implicated in the pathogenesis. Intrameniscal calcium can demonstrate increased signal intensity that can mimic a meniscal tear on T1-, PD-, and T2-weighted MRIs. No single theory has satisfactorily explained the cause of the high signal intensity of calcium on MRIs. [18, 40, 19, 24, 77, 87]
Correlation with plain radiographic results reduces the incidence of this error.
Other pitfalls
Separate portions of the posterior horn of the LM may be mistaken for a bucket-handle tear on coronal images. Normal meniscal signal is present on the sagittal images.
The bursa of the medial collateral ligament (MCL) is located between the periphery of the body of the MM and the MCL. Fluid within the bursa may be mistaken for a peripheral meniscocapsular tear on T2W1.
Aliasing occurs when all the anatomic structures of a desired body segment are not included in the field of view of the imaging section. This can be eliminated by increasing the field of view, oversampling by applying saturation pulses outside the region, or using surface coils.
Chemical-shift artifacts are found at the interface between fat and other structures. These increase with field strength and are more pronounced in images acquired with a narrow bandwidth.
Motion artifacts arise from flow in pulsating blood vessels, and reduced levels of patient cooperation, which is sometimes related to pain and apprehension.
Inhomogeneous fat saturation is caused by a nonuniform magnetic field. It is more pronounced on frequency-selective, T2-weighted, spin-echo images. It is also found in the presence of metallic artifacts.
Treatment & Management
Repair or resection of meniscal injuries is one of the most common orthopedic operative procedures. Meniscal injuries have a tremendous physical and financial impact on the population. It has been estimated that more than 1.7 million patients undergo meniscal surgery every year.
Various treatment options have been used for meniscal repair and reconstruction. The optimal treatment of meniscal lesions remains controversial. With the evolution of diagnostic MRI, it is no longer sufficient for the orthopedist to simply know that a meniscal tear is present. Treatment depends on knowledge of the exact type, location, and extent of the meniscal tear.
A study of 220 patients with meniscal tear and knee osteoarthritis (OA) reported that patients with MRI findings of less intra-articular damage had greater pain improvement after arthroscopic partial meniscectomy (APM) and physiotherapy (PT) compared to PT alone. The researchers concluded that MRI findings of intra-articular damage may be helpful in treatment planning for patients with meniscal tears and OA. [106]
Severe damage, loss, or removal of the menisci frequently leads to joint instability and, later, accelerated degenerative joint disease (DJD), resulting in further disability and joint replacement.
Factors associated with poor clinical outcomes after partial meniscotomy include a great severity of cartilage loss and bone marrow edema in the same compartment of the meniscal tear. [107] A greater severity of meniscal extrusion and longer meniscal tears on preoperative MRI are associated with poor clinical outcomes. Poorer clinical outcomes are also associated with meniscal root tears because these are often associated with meniscal extrusion.
Sequelae of Meniscal Tears
There is an increased risk of developing cartilaginous lesions after meniscal tears. Medial meniscal tears are associated with diffuse cartilaginous defects, and lateral meniscal tears are associated with focal cartilaginous tears. The difference may be related to meniscal loading and differences in meniscal rotation. [108]
The clinical course of knees with initially asymptomatic meniscal tears, compared with that of knees without meniscal tears, is characterized by an increased frequency of complaints 2-3 years post injury. The severity of pain and functional impairment, however, remains low. [109]
Horizontal and oblique tears appear to cause symptoms only when associated with collateral ligament lesions or bone marrow edema.
The question of stability of a torn meniscus is important in deciding whether to resect or repair a meniscus or leave it alone. [110] In a study by Boxheimer et al, all missed meniscal tears were associated with an ipsilateral collateral ligament injury of grade 2 or 3. Patients with displaced meniscal tears had more pain than patients with nondisplaced tears. [99] Certain types of meniscal tears are associated with displacement. Horizontal and oblique tears are present only in the nondisplaced menisci, whereas longitudinal tears are exclusively present in displaced tears. [110]
-
Sagittal fat-saturated proton density–weighted image demonstrates the concave superior meniscal surface (arrows), which improves contact with the femoral epicondyles, and a flat undersurface, which improves contact with the tibial plateau. The periphery (outer edges) is thicker than the central portion (arrowhead), allowing for firm attachment to the joint capsule. Note the normal bow-tie appearance of the meniscal body.
-
Coronal fat-saturated proton density–weighted image shows the relative size of the posterior horns of the medial and lateral menisci. The posterior horn of the medial meniscus (left arrow) is thicker than the posterior horn of the lateral meniscus (right arrow). Note the normal dark appearance (relative lack of signal intensity) in the menisci. The medial portion of the posterior horn of the lateral meniscus (ie, the meniscus on top of the fibula) is directed upward obliquely, from a lateral to medial direction. This is its normal course.
-
Axial fat-saturated proton density–weighted image demonstrates the transverse (intermeniscal) ligament (arrows) connecting the anterior portions of the medial and lateral menisci.
-
Coronal proton density–weighted image shows the intermeniscal ligament (arrow) connecting the anterior horns of the medial and lateral menisci.
-
Coronal fat-saturated proton density–weighted image shows the popliteus recess containing joint fluid and located between the lateral aspect of the posterior horn of the lateral meniscus and the joint capsule. An extensive tear is present in the posterior horn of the medial meniscus (arrow). Note the normal oblique upward orientation of the posterior medial horn of the lateral meniscus.
-
Coronal fat-saturated proton density–weighted image shows the dark appearing popliteus tendon (arrows) passing through the popliteus recess. The posterior medial horn of the lateral meniscus is directed obliquely upward.
-
Sagittal proton density–weighted image of the lateral knee compartment. It shows the superior fascicle (arrow) attaching the posterior horn of the lateral meniscus with the joint capsule. Hyperintense (bright) fluid is present in the popliteus recess. The inferior fascicle is not yet visualized.
-
Sagittal fat-saturated proton density–weighted image shows the inferior fascicle. In this location, the superior fascicle is not present. Note the normal bow-tie appearance of the meniscal body.
-
Coronal proton density–weighted image shows the ligament of Wrisberg originating from the posterior medial horn of the medial meniscus and passing obliquely upwards (arrow) to attach to the posterolateral aspect of the medial femoral epicondyle.
-
Coronal fat-saturated proton density–weighted image shows the popliteus tendon originating from an undulation of the lateral femoral condyle. From there, it passes through the popliteus recess to insert on the proximal posterior tibial metaphysis. A radial tear (arrow) is present in the posterior horn of the medial meniscus.
-
Coronal proton density–weighted image posterior to the knee joint shows the normal junction of the popliteus tendon and muscle passing obliquely downwards to insert on the posterior tibial metaphysis. There is a tear to the conjoint tendon of the biceps muscle and lateral collateral ligament (LCL, arrow).
-
Coronal proton density–weighted image of the popliteus tendon (outer arrows), which passes obliquely caudal, left to right, becoming the popliteus muscle (lower central arrow) and inserting on the proximal posterior metaphysis.
-
Coronal fat-saturated proton density–weighted image of the mid knee shows the normal appearance of the body of the medial and lateral menisci. The apices (inner portions) are the thinnest part of the meniscus and are more central in the knee joint. The periphery, meniscal bases, outer portion (arrow and arrowhead) is the thickest part and contains the blood vessels supplying the meniscus.
-
Coronal fat-saturated proton density–weighted image of the anterior knee shows the horizontal attachment of the anterior horn of the lateral meniscus (arrow) attaching near the intercondylar eminence.
-
Coronal fat-saturated proton density–weighted image shows the attachment of the anterior horn of the lateral meniscus. In this patient, the anterior horn attachment is near the tibial attachment of the anterior cruciate ligament (ACL, arrow).
-
Sagittal fat-saturated proton density–weighted image of the lateral compartment shows the relative equal size of the anterior and posterior horns of the lateral meniscus. The meniscal body has the normal configuration of a bow tie.
-
Sagittal fat-saturated proton density–weighted image of the medial compartment shows the larger posterior horn (arrowhead) and the smaller anterior horn.
-
Sagittal proton density–weighted image of the medial compartment. The thin apex of the meniscal body connects the large anterior and posterior horns at this level, giving the appearance of a bow-tie configuration (arrow).
-
Sagittal proton density–weighted shows a small amount of abnormal signal intensity in the anterior horn of the medial meniscus (arrow). This represents a grade 1 change in signal intensity.
-
Coronal proton density–weighted image shows extensive grade 2 signal intensity in the anterior and posterior horns of the medial meniscus. However, the signal intensity does not extend to a joint surface.
-
Sagittal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus, which appears to extend close to the inferior surface. This represents grade 2C changes in signal intensity. It can be difficult to differentiate grade 2 and grade 3 changes. Injuries causing grade 2C signal intensity can progress to degenerative tears.
-
Coronal fat-saturated proton density–weighted image of the knee shows a bucket tear of the posterior horn of the medial meniscus. It is a full-thickness tear involving both the superior and inferior articular surfaces. The wide separation of the margins of the tear usually results in poor outcomes with surgical repair. Also present is a horizontal tear of the meniscal body extending from the margin of the bucket handle tear to the meniscal base. Such tears usually occur in older patients and are not usually amenable to surgical repair.
-
Coronal fat-saturated proton density–weighted image of the knee shows a full-thickness radial tear. The ability of fat saturation to remove the high signal intensity of fat from the signal intensity bone marrow and subcutaneous tissue makes it an excellent way to highlight meniscal tears.
-
Sagittal proton density–weighted image of the mid portion of the medial compartment shows a full-thickness horizontal tear of the posterior horn of the medial meniscus extending from the base to the superior surface. In addition, image shows amputation of the inferior apex of the posterior horn. The combination of these 2 tears involving the same part of the meniscus makes this injury a complex tear.
-
Sagittal proton density–weighted image shows an amputated inferior base of the posterior horn of the lateral meniscus; this represents a partial tear.
-
Sagittal proton density–weighted image shows almost complete disappearance of the posterior horn of the medial meniscus. The loss of the normal shock-absorbing function of the meniscus predisposes the person to the loss of cartilage and subsequent bone abnormalities typical of degenerative arthritis.
-
Sagittal fat-saturated proton density–weighted image shows amputation of the apex of the posterior horn of the lateral meniscus. The anterior horn is deformed, and the image shows irregularity and deformity of the adjacent portion of the femur, which may have occurred with the injury to the anterior horn.
-
Sagittal proton density–weighted image shows an enlarged, abnormal, globular posterior horn of the medial meniscus with abnormal signal intensity. The abnormal appearance is related to edema from the meniscal tear.
-
Image shows a uniform decrease in the size of the body of the medial meniscus (arrow). The superior apex of the body of the lateral meniscus (arrowhead) has been amputated.
-
Image shows amputation of much of the inferior portion of the apex and part of the base of the body of the medial meniscus.
-
Coronal proton density–weighted image shows that most of the posterior horn of the lateral meniscus has been amputated (vertical arrow). An extensive partial-thickness tear is present on the undersurface of the body of the medial meniscus and extends to the meniscal base (oblique arrow).
-
Sagittal fat-saturated proton density-weighted image of the medial compartment showing a large area of increased signal intensity (arrow) representing joint fluid which, occupies the site where the normal meniscus should be located. This cleft within the meniscus represents a large, full-thickness radial tear of the meniscal body. It is full thickness because the tear involves the superior and inferior articular surfaces of the meniscus. The radial tear divides the meniscal body into anterior and posterior portions.
-
Sagittal fat-saturated proton density–weighted image, slightly more medial in the knee joint. Image shows the horizontal tear in the posterior horn of the medial meniscus (arrow). The amputation of the apex of the inferior horn is more evident on this image than on the other one. When a meniscal tear is visualized on at least 2 consecutive images, the accuracy that the tear is real and not an artifact approaches 100%. Its presence is almost always verified on arthroscopy.
-
Coronal fat-saturated proton density–weighted image shows abnormal signal intensity in the posterior horn of the medial meniscus (MM) extending to the undersurface near the junction with the joint capsule. Such tears may be missed on arthroscopy because that part of the knee joint is difficult to access. Also present is a tear to the posterior medial horn of the lateral meniscus (LM) as it slopes obliquely inward. A false-positive diagnosis of meniscal tear can be made when one evaluates this region because of the magic angle effect. Tears persist when the echo time (TE) is varied and when T2-weighted images are obtained. True tears can also be confirmed by visualizing them on sagittal or axial projections.
-
Sagittal proton density–weighted image shows the tibial insertion site of the posterior horn of the medial meniscus (MM).
-
Sagittal fat-saturated proton density–weighted image shows the tibial insertion of the posterior horn of the medial meniscus (MM). This portion of the meniscus has a normal, speckled appearance.
-
Sagittal fat-saturated proton density–weighted image of the posterior knee compartment shows the normal insertion (arrow) of the semimembranosus tendon. The insertion site is near the posterior horn of the medial meniscus (MM), and it is not to be mistaken for a displaced meniscal fragment.
-
Sagittal fat-saturated proton density–weighted image shows a full-thickness tear to the periphery of the anterior horn of the medial meniscus (MM). Tears in this location have a good likelihood of healing without surgical repair because they occur in the zone with a good blood supply to the meniscus. Also present is a partial thickness tear to the undersurface of the posterior horn of the MM.
-
Coronal proton density–weighted image shows a full-thickness, vertical bucket handle tear (arrow) through the base of the medial meniscus (MM).
-
Coronal fat-saturated proton density–weighted image shows the tibial insertion of the anterior horn of the lateral meniscus (LM, arrows) and the intimate association sometimes seen between the insertion of the meniscus and the tibial insertion of the anterior cruciate ligament (ACL). Normal interdigitations of the ACL are present at this site. Fat is also present and appears hyperintense on T1- and proton density–weighted images. This is not to be confused with a meniscal or ACL tear.
-
Coronal fat-saturated proton density–weighted image shows irregularity to the upper (femoral) surface of the body of the lateral meniscus (LM, outer arrow), indicating fraying. Fraying usually occurs at the meniscal apex. Soft tissue densities (inner arrow) are present under the apex of the meniscus, indicating debris or a free meniscal fragment at this level. The body of the LM is unusually thick and longer than usual, indicating a discoid meniscus. The normal-sized medial meniscal body is present for comparison. Discoid menisci occur about 5 times more often here than in the LM, and they are more prone to injury.
-
Sagittal proton density–weighted image shows a vertical bucket handle tear (arrow) through the periphery of the posterior horn of the medial meniscus (MM). Tears in this location do not usually heal spontaneously because this portion of the meniscus lacks blood supply.
-
Sagittal fat-saturated proton density–weighted image of the paramedian portion of the lateral joint compartment. The transverse intermeniscal ligament (arrowhead) is about to unite with the anterior horn of the medial meniscus (MM, arrow). Fat is normally present in this region and can mimic a ligament or meniscal tear. By carefully following the course of the ligament on sequential images and by observing a uniformly well-defined, hypointense structure on every image, this pitfall can be avoided. A small, ill-defined, linear soft tissue density is present under the anterior horn. It is separated from the anterior horn by bright fluid. This is a rare tear in this region. The brightness is joint fluid in the tear.
-
Sagittal fat-saturated proton density–weighted image of the paramedian portion of the medial knee. The transverse intermeniscal ligament is about to insert on the anterior horn of the medial meniscus (MM). The anterior horn is normally speckled. The anterior horn is partially displaced off the anterior surface of the tibia by a radial tear more laterally (picture is not shown). A tear involves the posterior horn of the MM (arrow).
-
Sagittal proton density–weighted image shows a full-thickness horizontal tear of the posterior horn of the lateral meniscus (LM, arrow) involving the superior articular surface.
-
Sagittal fat-saturated proton density-weighted image shows a well-defined, soft tissue density in front of the posterior cruciate ligament (PCL). It is speckled and looks like the normal posterior medial horn of the medial meniscus (MM), but it is in the wrong place. This finding represents a displaced meniscal tear involving the posterior medial horn. The position of the meniscus is referred to as a double PCL because it looks like 2 of these ligaments are present.
-
Coronal fat-saturated proton density-weighted image shows speckled displaced meniscal fragment (inner arrows). Also present is an extensive horizontal tear to the body of the medial meniscus (MM) with a lot of hyperintensity at the periphery (outer arrows). This represents a meniscal cyst. Repair of the cyst without repair of the underlying meniscal tear results in recurrence of the cyst.
-
Sagittal fat-saturated proton density–weighted image shows soft tissue (arrows) lying on top of the anterior horn of the medial meniscus (MM), separated from it by high signal intensity (bright joint fluid). This finding represents a displaced meniscal fragment. The posterior horn of the MM is abnormally shaped and has abnormal signal intensity. This is the origin of the displaced fragment. The height of the combination of the displaced fragment and the anterior meniscus is greater than 8 mm. The height of the meniscal tissue equal to or greater than this number is a good sign of a displaced meniscal fragment.
-
Coronal fat-saturated proton density-weighted image of the same patient as in the previous image shows a different view of the meniscal fragment and the anterior horn. As in the previous image, an appearance of a double anterior meniscus is shown.
-
Coronal fat-saturated proton density–weighted image of the posterior knee Shows an extensive horizontal tear involving the undersurface of the posterior meniscus. Also present is a flap on the undersurface of the meniscus that has been displaced medially and that is now directed vertically and inferiorly. Note the normal insertion site of the semimembranosus tendon (arrow) that might be confused for a displaced meniscal fragment.
-
Anterior image of the same patient as in the previous image shows the tear to the undersurface of the posterior horn of the medial meniscus (MM, large solid arrow). Image also shows a displaced meniscal fragment lying on top of the body of the lateral meniscus (LM, small solid arrow). The lateral meniscal tear was located more anterior in the body (picture not shown). Open arrow indicates abnormal signal at the origin of the popliteus tendon, representing a partial tear.
-
Sagittal proton density-weighted image of the outer portion of the lateral side of the knee shows an absence of the body of the lateral meniscus (LM, arrow). The body of the meniscus should be visualized peripherally. The normal appearance of the meniscus has the appearance of a bow tie; the bow tie is absent here.
-
Sagittal fat-saturated proton density–weighted image shows an unusually tall anterior meniscal horn. On closer inspection, a separation is present between the upper (arrowhead) and lower (arrow) portions. The upper portion is a displaced meniscal fragment from the posterior meniscus lying on top of the anterior horn. Most of the posterior meniscus is absent from its usual location. When the height of a meniscus is greater than 8 mm, it likely represents the combination of a displaced meniscal fragment and a normal meniscus.
-
Coronal fat-saturated proton density–weighted image of the posterior portion of the knee joint. A circular, fluid-filled structure (arrow) is present in the upper portion of the most medial portion of the posterior horn of the medial meniscus; it represents a meniscal cyst.
-
Axial fat-saturated proton density–weighted image shows the location of the cyst in the most medial portion of the medial meniscus.
-
Sagittal fat-saturated proton density–weighted image shows the cyst (arrow) in a different projection.
-
Coronal fat-saturated proton density–weighted image obtained more posteriorly. Abnormal signal intensity (small arrows) is present medial to the base of the posterior horn of the medial meniscus (MM). No medial collateral ligament (MCL) is discernible at this level; this appearance indicates a tear. This is fluid of the meniscus from its normal attachment with the MCL, representing meniscocapsular separation. The insertion of the semimembranosus tendon (large arrow) has abnormal signal intensity; this finding indicates a tear.
-
Coronal fat-saturated proton density-weighted image obtained more posteriorly than in the previous image. The separation of the base of the meniscus from the medial collateral ligament (MCL, large solid arrow) is evident. Image shows interruption and abnormal signal intensity in the MCL (small arrows), indicating a tear. Large open arrow indicates a soft tissue density, either blood products or a free meniscal fragment below the joint space between the tibia and MCL. It is easy to see how inferomedial displaced tears from the medial meniscus (MM) can go unnoticed on arthroscopy. The tear is hidden,, and it is difficult to bend the arthroscope around the tibia to see below the joint. A fracture is present in the central portion of the articular surface of the tibia (oblique central arrow in the tibia),, and another tear is present in the posterior medial horn of the medial meniscus near the tibial insertion site.
-
Image in a different patient shows a cyst in the body of the medial meniscus (MM) with meniscocapsular separation. At this level, the medial collateral ligament (MCL, arrow) is intact.
-
Sagittal proton density–weighted image obtained from the outer portion of the lateral aspect of the knee. Image shows interruption of the inferior fascicle (arrow) of the lateral meniscus (LM). No pericapsular edema is present.
-
Sagittal proton density–weighted image of the same patient as in the previous image but slightly more medial. Image shows abnormal signal intensity with interruption of the superior fascicle of the lateral meniscus (LM). No pericapsular edema is present.
-
Sagittal proton density–weighted image of a patient who underwent partial meniscectomy of the body and posterior horn of the medial meniscus (MM). Image shows slight hypertrophy and increased signal intensity to the posterior femur, indicating secondary degenerative arthritis related to removal of the meniscus.
-
Coronal fat-saturated proton density–weighted image of the posterior aspect of the knee. A soft tissue density (arrow) lies between the lateral portion of the medial femoral epicondyle and the posterior cruciate ligament (PCL). This represents the notch fragment. A horizontal tear is present on undersurface of the body of the medial meniscus (MM). The difference between the notch fragment sign and the double PCL sign is merely one of position of the meniscal fragment. The fragment is more medial with the notch fragment sign than in the double PCL sign.
-
Oblique radiograph of the right knee demonstrates bright triangular lines on either side of the joint. This finding represents calcium in the triangular menisci, which represents chondrocalcinosis. A globular calcium opacity (arrow) is above the periphery of the body of the lateral meniscus; this might represent a calcified loose body, either in the joint proper or in the popliteus recess. The presence of chondrocalcinosis can result in a false-positive diagnosis of a meniscal tear.
-
Coronal fat-saturated proton density–weighted image of the posterior aspect of the knee shows the normal vertically oblique course of the popliteus recess. Immediately medial to the recess is a longitudinally oblique area of high signal intensity (arrow) located in the posterior horn of the lateral meniscus (LM), communicating with the recess and representing an oblique tear.
-
Coronal proton density–weighted image shows a displaced medial meniscal body (arrow) bowing the medial collateral ligament (MCL). The thin meniscus apex is pointing upward, and the thicker base is more caudal in position, indicating meniscocapsular separation with reorientation of the position of the meniscus. In addition, the meniscus has twisted 180° because the concave femoral surface is directed toward the femur. If it had simply flipped upward, it would face the MCL.
-
Axial illustration of a full-thickness longitudinal tear of the posterior horn. The meniscus is viewed from above in (a), sagittal in (b), and coronal in (c). For Image 67-70, A = anterior, L = lateral, M = medial, and P = posterior.
-
Axial illustration of a full-thickness radial tear of the posterior horn. The meniscus is viewed from above.
-
Axial illustration of a full-thickness horizontal tear of the posterior horn. The meniscus is viewed from above.
-
Axial illustration of an oblique (parrot beak) tear of the posterior horn. The meniscus is viewed from above. In B, image 1 is most lateral, image 2 is middle, and image 3 is most medial. In C, image 1 is most anterior, image 2 is middle, and image 3 is most posterior.







