Practice Essentials
Rheumatoid arthritis (RA) is a chronic multisystemic disease of unknown cause. The characteristic feature is persistent inflammatory synovitis usually involving peripheral joints in a symmetrical distribution. Synovial inflammation causes cartilage destruction and bone erosion. Subsequently, joint deformity occurs. The axial skeleton, with the exception of the cervical spine, is affected later and less frequently. The risk factors for cervical spine involvement include frequency of peripheral joint erosion, rheumatoid factor (RF) positivity, use of corticosteroids, long RA duration, and markers of higher disease activity (erythrocyte sedimentation rate, C-reactive protein, and disease activity score). [1, 2]
Extensive angiogenesis occurs in the synovial tissue, with interactions between vascular endothelial cells, fibroblasts, macrophages, and the extracellular matrix. Synovial fibroblasts and activated immune cells are responsible for the production of inflammatory cytokines, which are believed to play a role in the development and progression of RA. [3, 4]
Clinically, cervical spine involvement in RA patients is reported to be mainly seen in 3 forms: atlantoaxial subluxation (AAS) (65%), superior odontoid migration (SOM) (20%), and subaxial subluxation (SAS) (15%). [5] In cases of AAS, anterior subluxation may be most common (70%), followed by lateral subluxation (20%). Posterior subluxation is seen in 7% of cases, and rotational subluxation is very rarely reported. [6]
Imaging modalities
The mainstay of imaging the rheumatoid spine remains plain radiography to identify anterior atlantoaxial subluxation via the anterior or posterior atlantodental interval; vertical subluxation via the McGregor method or Ranawat index; diameter of the spinal canal; and cervical height index. Flexion/extension views are necessary to assess the level of involvement and any evidence of instability. [5, 7] The need for further imaging by means of CT, MRI, or myelography may also be assessed during radiography. [5] The major role for CT and MRI is in the preoperative assessment.
The correlation of MRI findings with symptoms is crucial before any surgical decisions can be made. There is a close correlation between the severity of cervical myelopathy and the degree of compression as demonstrated by MRI. Besides influencing the selection of patients for spinal surgery, MRIs can help in planning surgical procedures, especially those in patients with more than 2 levels of cord compression. [8, 9, 10]
According to some studies, nuclear imaging modalities such as single-photon emission computed tomography (SPECT) and positron emission tomography (PET) can selectively target molecular markers of angiogenesis and track molecular changes in joints. [3, 11, 12]
Computed tomography allows for a very precise assessment of bone structure of the whole cervical spine. The anatomy of the atlantoaxial joint is more visible than on a plain radiograph, where the image deteriorates because of overlapping bone structures. CT is also considered to be the best method for the visualization of bone erosion, as well as atypical subluxation within the atlantoaxial joint, in particular lateral and rotary subluxation. [13, 14]
(See the images below.)
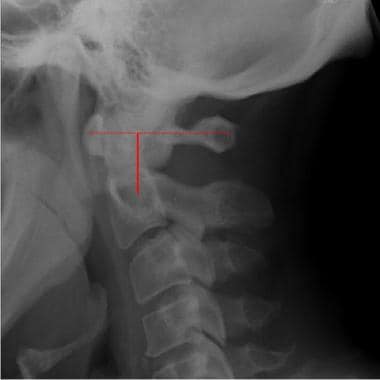
 Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
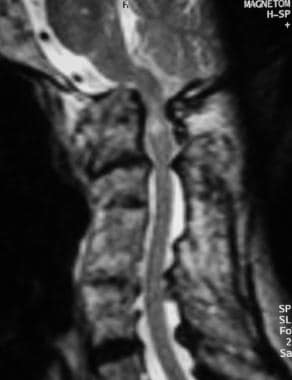
 T1-weighted sagittal MRI of the cervical spine shows basilar invagination with cranial migration of an eroded odontoid peg. There is minimal pannus. The tip of the peg indents the medulla, and there is narrowing of the foramen magnum due to the presence of the peg. Inflammatory fusion of several cervical vertebral bodies is shown.
T1-weighted sagittal MRI of the cervical spine shows basilar invagination with cranial migration of an eroded odontoid peg. There is minimal pannus. The tip of the peg indents the medulla, and there is narrowing of the foramen magnum due to the presence of the peg. Inflammatory fusion of several cervical vertebral bodies is shown.
After the metacarpophalangeal joints, the most common region to be involved in RA is the cervical spine. This can lead to severe pain and disability, as well as various neurologic manifestations, although some patients with significant radiographic evidence of disease may be entirely asymptomatic. The frequency of radiographic signs of involvement of the cervical area is 44-86%, depending on the duration of the disease. [13]
RA activity in the cervical spine begins early, with 83% of patients in prospective studies developing anterior atlantoaxial subluxation within 2 years of disease onset. Activity in the cervical spine progresses clinically and radiologically in tandem with peripheral joint involvement. In fact, the severity of the peripheral erosive damage is strongly correlated with the degree of structural damage in the cervical spine. Features of spinal involvement in RA include erosive synovitis, ligamentous subluxation, osteopenia, and vertebral-body fracture. [15]
Radiography
Anterior atlantoaxial subluxation
Only half of patients with radiographic evidence of atlantoaxial subluxation (AAS) are actually symptomatic. The role of plain radiography is to establish whether there are risk factors for cord compression. AAS is defined as an anterior atlantodental interval (AADI) greater than 2.5 mm in adults. This distance is measured as the interosseous distance between the posterior aspect of the arch of the atlas and the anterior aspect of the odontoid process. The point of measurement of the joint is a subject of debate; the inferior point is the most popular.
(See the images below.)
 Plain lateral radiograph of the normal cervical spine taken in extension shows measurement of anterior atlantodental interval (yellow line) and posterior atlantodental interval (red line).
Plain lateral radiograph of the normal cervical spine taken in extension shows measurement of anterior atlantodental interval (yellow line) and posterior atlantodental interval (red line).
There may be a slight variation in normal measurements between men and women. More importantly, it should be noted that an atlantodental interval of less than 2.5 mm, which changes considerably on flexion and extension, may also be abnormal. An AADI of 3-6 mm indicates early instability and implies transverse ligament damage. [16] An AADI greater than 6 mm indicates that the alar ligaments are also damaged. Some authors consider an AADI greater than 9 mm to be an indication for surgical stabilization.
Posterior atlantodental interval
Studies suggest that the posterior atlantodental interval (PADI) is a better method of assessing AAS because the PADI directly measures the spinal canal and therefore shows how much is narrowed by the subluxation. The PADI is the distance between the posterior surface of the odontoid and the anterior margin of the posterior ring of the atlas. At all cervical spinal levels, the cord requires a minimum canal width of 10 mm; CSF, 2 mm; and dura, 2 mm. Therefore, a minimum PADI of 14 mm is required to avoid cord compression. The normal spinal canal measures 17-29 mm at C1.
Boden et al investigated the predictive value of the PADI and found that a value of less that 14 mm on plain radiographs had a 97% ability to detect patients with neurologic deficit. [17] Also, neurologic recovery from surgery was unlikely if the PADI fell beneath 10 mm. Moreover, complete motor recovery occurred if the surgery was performed while the PADI was greater than 14 mm.
Detecting vertical subluxation
Regarding the McGregor method, vertical subluxation (VS) has been defined as the protrusion of the odontoid tip by more than 4.5 mm above the McGregor line. [18] This is drawn between the posterosuperior aspect of the hard palate and the most caudal aspect of the occiput. However, it is not the most accurate measurement in the rheumatoid spine because of odontoid erosion and often marked osteoporosis.
The Ranawat index is used to assess VS by detecting settling of C1 on C2. The measurement is made from the center of the pedicles of C2 to a line connecting the midpoint of the anterior and posterior arches of C1. Normal values are 15 mm or greater for men and 13 mm or greater for women. Anything less than this confirms VS.
(See the images below.)
 Lateral radiograph of a normal cervical spine shows the McGregor line. The odontoid tip should not protrude more than 4.5 mm above the line, which is drawn from the posterior edge of the hard palate to the most caudal point of the occiput.
Lateral radiograph of a normal cervical spine shows the McGregor line. The odontoid tip should not protrude more than 4.5 mm above the line, which is drawn from the posterior edge of the hard palate to the most caudal point of the occiput.
 Normal lateral magnified radiograph of the cervical spine shows the Ranawat method of detection of cranial settling. This method is used to measure the distance from the center of the pedicles (sclerotic ring) of C2 to a line drawn connecting the midpoints of the anterior and posterior arches of C1. (Normal values are 15 mm or greater for males and 13 mm or greater for females.)
Normal lateral magnified radiograph of the cervical spine shows the Ranawat method of detection of cranial settling. This method is used to measure the distance from the center of the pedicles (sclerotic ring) of C2 to a line drawn connecting the midpoints of the anterior and posterior arches of C1. (Normal values are 15 mm or greater for males and 13 mm or greater for females.)
Confirming subaxial subluxation
The diameter of the spinal canal is actually a better predictor of the development of paralysis than the degree of subluxation of one vertebral body on another. The normal sagittal diameter from C3 to C7 is 14-23 mm. A spinal canal sagittal diameter of at least 14 mm is critical at all levels in the cervical spine, as this is the minimum space required for the cord, CSF, and dura.
The cervical height index (CHI) is a method for assessing subaxial subluxation that takes into account the contribution of subluxations at multiple levels, together with loss of disk height and bony collapse. The CHI is calculated by first measuring the distance from the center of the sclerotic ring of C2 (as used in the Ranawat method) to the tip of the spinous process of C2. This distance is then divided into the distance from the center of the C2 sclerotic ring to the midpoint of the inferior border of C7 vertebral body. A CHI of less than 2 has a sensitivity and specificity approaching 100% in predicting neurologic compromise.
(See the image below.)
 Lateral radiograph of the cervical spine shows how the cervical height index (CHI) is calculated. The distance from the center of the sclerotic ring of C2 to the tip of the spinous process of C2 (dotted line) is measured. This is then divided into the distance from the center of the sclerotic ring of C2 to the mid-point of the inferior border of the body of C7. A CHI of less than 2 mm is a sensitive predictor of neurologic deficit.
Lateral radiograph of the cervical spine shows how the cervical height index (CHI) is calculated. The distance from the center of the sclerotic ring of C2 to the tip of the spinous process of C2 (dotted line) is measured. This is then divided into the distance from the center of the sclerotic ring of C2 to the mid-point of the inferior border of the body of C7. A CHI of less than 2 mm is a sensitive predictor of neurologic deficit.
These plain radiographic measurements, along with dynamic flexion-extension views, provide a reliable and efficient means of assessing spinal involvement of rheumatoid disease and targeting at-risk patients, as well as selecting those who warrant further radiologic studies with a view to surgical stabilization.
Thoracic and lumbar spinal involvement
RA changes in the apophyseal joints of the thoracic and lumbar spine are reported only infrequently. Alterations at the discovertebral junctions have also been noted. Intervertebral disk-space narrowing, irregularity of the subchondral margins of the vertebral bodies, erosion, and sclerosis can be evident on radiography. Patients with RA who are receiving corticosteroid medication are predisposed to ischemic necrosis of bone. Although the femoral head is the usual site for this, vertebral bodies in the thoracic and lumbar regions of the spine can be affected. On radiography, this may be seen as vertebral collapse and fragmentation. Radiolucent fracture lines, which may accumulate gas from surrounding tissues, are an important clue to the diagnosis.
Magnetic Resonance Imaging
The major role for CT and MRI is in the preoperative assessment of the 2 main indications for surgical intervention: neurologic deficit and severe pain. [19, 20] The subluxations that are of a degree likely to result in paralysis need to be identified, as better outcomes have been reported with earlier interventions. The effect of pannus and intracanal granulations on the cord cannot be accurately assessed on plain images, despite the fact that a posterior atlantodental interval (PADI) of less than 14 mm is a sensitive indicator of paralysis risk. [5, 14, 21]
(See the images below.)
 T1-weighted sagittal MRI of the cervical spine shows basilar invagination with cranial migration of an eroded odontoid peg. There is minimal pannus. The tip of the peg indents the medulla, and there is narrowing of the foramen magnum due to the presence of the peg. Inflammatory fusion of several cervical vertebral bodies is shown.
T1-weighted sagittal MRI of the cervical spine shows basilar invagination with cranial migration of an eroded odontoid peg. There is minimal pannus. The tip of the peg indents the medulla, and there is narrowing of the foramen magnum due to the presence of the peg. Inflammatory fusion of several cervical vertebral bodies is shown.
 Sagittal T2-weighted MRI of the cervical spine in the same case as in Image above. The compromised foramen magnum is easily appreciated, and there is increased signal intensity within the upper cord; this is consistent with compressive myelomalacia. Further narrowing of the canal is seen at multiple levels.
Sagittal T2-weighted MRI of the cervical spine in the same case as in Image above. The compromised foramen magnum is easily appreciated, and there is increased signal intensity within the upper cord; this is consistent with compressive myelomalacia. Further narrowing of the canal is seen at multiple levels.
Although CT scanning can document bone damage and alignment abnormalities, especially with more detailed multiplanar reconstruction, MRI has become the preferred modality for evaluation of the spinal cord and neural elements. [8] It demonstrates the presence and effect of pannus on the spinal cord and is useful in assessing its resolution following posterior fusion and stabilization. On MRI, the direct relationships of the odontoid to the medulla and brainstem can be documented. Spinal cord signal can be assessed; edematous changes in the cord are associated with a poor clinical status, as well as a poor prognosis and a poor postoperative outcome. [9]
The major indications for MRI in RA are abnormal measurements on plain radiographs, [22] unremitting suboccipital/cervical pain, progressive/severe subluxations, symptoms of cord/brainstem compression, and vertebral artery compression.
Dynamic MRI has been used with the patient in a flexed or extended position and in the traditional neutral position. Roca et al suggested that functional (flexed position) MRIs be obtained in patients with RA in whom cervical subluxation is suspected when routine MRI findings in the neutral position are normal. [23] Others recommend functional MRI as a preoperative examination. [24]
Pathologic series have suggested that cord atrophy in rheumatoid cervical myelopathy results from repeated traction injury as a result of compression, stretch, and movement as opposed to an inflammatory process per se. This is unsurprising considering that the atlantoaxial joint is the most mobile segment of the cervical spine.
In a study looking at the features of rheumatoid cervical myelopathy on MRI that were associated with subsequent deterioration, it was determined that in cases in which axial compression or impingement was identified on MRI, 60% of patients experienced deterioration resulting in death or surgical intervention over a median period of 12 months.
When functional imaging is performed, patient monitoring is advised, and rapid sequences are desirable because patients may find the flexed position uncomfortable. Some authors suggest that functional MRI is unnecessary and even contraindicated in patients in whom medullary or spinal cord compression is discovered on studies made in the neutral position.
Questions & Answers
-
Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
-
Plain lateral radiograph of the normal cervical spine taken in extension shows measurement of anterior atlantodental interval (yellow line) and posterior atlantodental interval (red line).
-
Lateral flexion view of the cervical spine shows atlantoaxial subluxation.
-
T1-weighted sagittal MRI of the cervical spine shows basilar invagination with cranial migration of an eroded odontoid peg. There is minimal pannus. The tip of the peg indents the medulla, and there is narrowing of the foramen magnum due to the presence of the peg. Inflammatory fusion of several cervical vertebral bodies is shown.
-
Sagittal T2-weighted MRI of the cervical spine in the same case as in Image above. The compromised foramen magnum is easily appreciated, and there is increased signal intensity within the upper cord; this is consistent with compressive myelomalacia. Further narrowing of the canal is seen at multiple levels.
-
Lateral radiograph of the same patient as in the two images above. Midcervical vertebral-body fusions are shown. The eroded peg is difficult to visualize, but inferior subluxation of the anterior arch of C1 is shown.
-
Lateral radiograph of a normal cervical spine shows the McGregor line. The odontoid tip should not protrude more than 4.5 mm above the line, which is drawn from the posterior edge of the hard palate to the most caudal point of the occiput.
-
Normal lateral magnified radiograph of the cervical spine shows the Ranawat method of detection of cranial settling. This method is used to measure the distance from the center of the pedicles (sclerotic ring) of C2 to a line drawn connecting the midpoints of the anterior and posterior arches of C1. (Normal values are 15 mm or greater for males and 13 mm or greater for females.)
-
Lateral radiograph of the cervical spine shows how the cervical height index (CHI) is calculated. The distance from the center of the sclerotic ring of C2 to the tip of the spinous process of C2 (dotted line) is measured. This is then divided into the distance from the center of the sclerotic ring of C2 to the mid-point of the inferior border of the body of C7. A CHI of less than 2 mm is a sensitive predictor of neurologic deficit.










