Practice Essentials
The distal radius fracture (DRF) is the most common fracture of the forearm and accounts for approximately 16% of all skeletal fractures. It is usually caused by a fall onto an outstretched hand (FOOSH). It can also result from direct impact or axial forces. The description of these fractures is based on distal radial angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones. Distal radius fractures with articular involvement are more likely to require surgical management. Treatment decisions are generally based on radiographic findings. Functional outcome measures of DRF treatment and rehabilitation are most commonly made by range of motion (ROM), grip strength (Grip), and the Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH). [1, 2, 3, 4]
(See the images below.)
 Posteroanterior radiograph demonstrates a comminuted fracture of the distal radius. Note should be made of angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones.
Posteroanterior radiograph demonstrates a comminuted fracture of the distal radius. Note should be made of angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones.
 Lateral radiograph demonstrates a comminuted fracture of the distal radius. Note should be made of angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones.
Lateral radiograph demonstrates a comminuted fracture of the distal radius. Note should be made of angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones.
Most distal radius fractures are diagnosed by conventional radiography. Computed tomography (CT) and magnetic resonance imaging (MRI) are used in the evaluation of complex distal radial fractures, for the assessment of associated injuries, and for preoperative and postoperative management. [5, 6, 7] The use of ultrasound as a point-of-care triage tool to select the children with wrist trauma who need radiographs has been suggested as a means of reducing radiation exposure. [8]
Wrist injuries that result in pain, edema, crepitus, deformity, or ecchymosis should be evaluated for distal radial fractures. Delayed diagnosis of a distal radial fracture can lead to significant morbidity.
Classification systems
There are numerous classification systems that describe fractures of the distal radius, traditionally chosen by the clinician based on preference. [9, 5, 10] Classification systems should be based on the following 2 principles:
-
The classification should dictate the treatment.
One example is the Universal Classification of Distal Radial Fractures (see Table 1). This system differentiates between extra-articular and intra-articular fractures, as well as between stable and unstable fractures; it was created as a treatment-based algorithm.
Table 1. Universal Classification of Distal Radial Fractures (Open Table in a new window)
Classification |
Description |
I |
Nonarticular, nondisplaced |
II A B C |
Nonarticular, displaced Reducible, stable Reducible, unstable Irreducible |
III |
Articular, nondisplaced |
IV A B C D |
Articular, displaced Reducible, stable Reducible, unstable Irreducible Complex |
Other classification systems for DRF include Frykman, Melone, Mayo Clinic, and Fernandez. [10]
Frykman classification:
-
I: Extra-articular
-
II: Extra-articular with fracture of the distal ulna
-
III: Radiocarpal joint involved
-
IV: Radiocarpal joint involved with fracture of the distal ulna
-
V: Distal radioulnar joint involved
-
VI: Distal radioulnar joint involved with fracture of the distal ulna
-
VII: Radiocarpal and distal radioulnar joints both involved
-
VIII: Radiocarpal and distal radioulnar joints both involved with fracture of the distal ulna
Melone classification:
-
I: Undisplaced, no or minimal comminution
-
II: ’Die punch’ fracture with moderate to severe displacement (IIa: reducible; IIb: irreducible)
-
III: Spike fragment present
-
IV: Wide separation of intra-articular fragments
-
V: Explosion fracture with severe comminution, transverse split, and rotational displacement
Mayo Clinic classification:
-
I: Intra-articular, undisplaced
-
II: Intra-articular, displaced, involving significant portion of articular surface
-
III: Intra-articular, displaced, often presents as ‘die punch’ fracture of lunate fossa
-
IV: Intra-articular, displaced, involving both radioscaphoid joint surfaces and usually sigmoid fossa of distal radioulnar joint, usually comminuted
Fernandez classification:
-
I: Bending of the metaphysis
-
II: Shearing fractures of the joint surface
-
III: Compression of the joint surface
-
IV: Avulsion or radiocarpal fracture dislocations
-
V: Combined fractures with high-velocity injuries
Imaging modalities
Posteroanterior (PA), lateral, and oblique radiographs of the injured wrist should be obtained. [16] Oblique views may reveal intra-articular involvement that is not apparent on the other views. The semisupinated, oblique view demonstrates the dorsal facet of the lunate fossa, whereas the partially pronated, oblique PA view allows visualization of the radial styloid. [17]
Radial height is assessed on the PA view. It is a measurement between 2 parallel lines that are perpendicular to the long axis of the radius. One line is drawn on the articular surface of the radius, and the other is drawn at the tip of the radial styloid. The normal radial height is 9.9 to 17.3 mm. [18] Measurements of less than 9 mm in adults suggest the presence of comminuted or impacted fractures of the distal radius. Comparison with the contralateral normal wrist is recommended if the diagnosis is unclear (see images below).
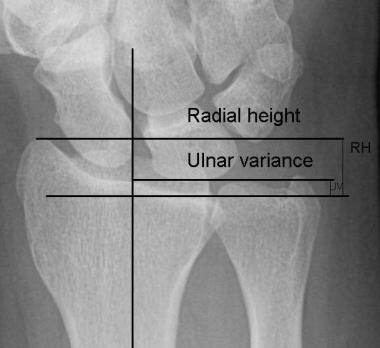 Radial height (RH) is measured by drawing 2 parallel lines perpendicular to the long axis of the radius. Shortening of RH may indicate impaction of the distal radius when compared with a normal contralateral wrist. Ulnar variance (UV) is measured here by using the method of perpendiculars, in which 2 lines are drawn perpendicular to the long axis of the radius. One line is drawn on the ulnar-side articular surface of the radius, and the other is drawn on the ulnar carpal surface. This image demonstrates ulnar plus variance.
Radial height (RH) is measured by drawing 2 parallel lines perpendicular to the long axis of the radius. Shortening of RH may indicate impaction of the distal radius when compared with a normal contralateral wrist. Ulnar variance (UV) is measured here by using the method of perpendiculars, in which 2 lines are drawn perpendicular to the long axis of the radius. One line is drawn on the ulnar-side articular surface of the radius, and the other is drawn on the ulnar carpal surface. This image demonstrates ulnar plus variance.
 Posteroanterior view of an adult left wrist demonstrates an impacted distal radial fracture. Measurement of radial shortening and comparison with the contralateral normal wrist aids in the diagnosis.
Posteroanterior view of an adult left wrist demonstrates an impacted distal radial fracture. Measurement of radial shortening and comparison with the contralateral normal wrist aids in the diagnosis.
Radial inclination is measured on the PA view; this is a measurement of the radial angle. A line is drawn along the articular surface of the radius perpendicular to the long axis of the radius, and a tangent is drawn from the radial styloid. The normal angle is 15 to 25º. [19, 20] Abnormal inclination of the distal radius may be a reflection of an impaction fracture of the distal radius (see image below).
 The radial inclination is measured by drawing a line perpendicular to the long axis of the radius and a tangential line from the radial styloid to the ulnar corner of the lunate fossa.
The radial inclination is measured by drawing a line perpendicular to the long axis of the radius and a tangential line from the radial styloid to the ulnar corner of the lunate fossa.
The volar tilt, or volar inclination, is measured on the lateral view. A line perpendicular to the long axis of the radius is drawn, and a tangent line is drawn along the slope of the dorsal-to-volar surface of the radius. The normal angle is 10 to 25º. [19, 20] A negative volar tilt indicates dorsal angulation of the distal, radial articular surface (see image below). [21]
 The volar tilt, or palmar/volar inclination, is an angle between a line drawn perpendicular to the long axis of the radius and a tangential line drawn along the radial articular surface.
The volar tilt, or palmar/volar inclination, is an angle between a line drawn perpendicular to the long axis of the radius and a tangential line drawn along the radial articular surface.
Ulnar variance is measured on PA radiographs. In adults, the following 3 methods are used [18] :
-
Project-a-line technique
-
Method of perpendiculars
-
Concentric-circle technique
Ulnar variance is described as being zero, minus, or plus. Positive (plus) or negative (minus) ulnar variance should be compared with the variance on the contralateral normal forearm. [19] Normal ulnar variance is 9 to 12 mm. Note that ulnar variance does not depend on the length of the ulnar styloid but on the positioning of the forearm, as well as on the radiographic technique.
Because fractures of the distal radius can be radiographically occult, an evaluation of the soft tissues of the distal forearm is important. For this assessment, 2 fat planes on the lateral view and 5 fat planes on the PA view are useful.
On the lateral view, the deep fat pad of the pronator quadratus and the dorsal skin subcutaneous fat line can be seen anterior to the distal radius. The deep fat pad of the pronator quadratus forms a slight, ventral concave line. This is convexly bowed in a ventral direction, disrupted, or completely obliterated in pathologic conditions. [22] The dorsal skin subcutaneous fat line is flat or is a dorsal concave line. It is abnormal when it is convex in the dorsal direction.
The PA view shows the thenar, hypothenar, pararadial, and paraulnar skin subcutaneous fat lines and the deep, navicular fat pad.
Swelling that is not associated with an observed fracture should initiate a search for an alternative abnormality or raise suspicion for a radiographically occult fracture.
DRFs that are not appropriately diagnosed with radiographic methods may result in increased morbidity when diagnosis is delayed. CT and MRI can be used to assess suspected occult fractures. Additionally, in instances of suspected clinically relevant soft-tissue injury, CT or MRI may be of benefit. Beware of the often-overlooked distal radioulnar subluxation/dislocation. [23, 24, 25, 26]
Goldwyn et al studied the use of traction radiography in the evaluation of distal radial fractures. They concluded that traction radiography may provide some of the same information as CT, but at a lower cost. They suggested further comparison between CT and traction radiography of the distal part of the radius as a result. [27]
Radiographic findings that are equivocal or potentially the result of normal anatomic variation require comparison with the contralateral wrist and/or additional imaging before intervention is recommended. [9]
Angiography is indicated in cases involving a compromise of vascular structures, as reflected in the clinical presentation.
Radiography
Colles fracture
In 1814, Abraham Colles described the Colles fracture, which is reported to be the most common distal radius fracture. The injury is usually produced by a fall onto an outstretched hand (FOOSH). The impact produces a transverse fracture in the distal 2-3 cm of the radius. The fracture is dorsally displaced and may be comminuted. The fracture pattern is often described as a silver or dinner-fork deformity. The fracture fragments are usually impacted and comminuted along the dorsal aspect. The fracture can extend into the epiphysis to involve the distal radiocarpal joint or the distal radioulnar joint (see image below). [17, 26]
Resnick noted that 50-60% of Colles fractures are associated with an ulnar styloid fracture. [28] An associated ulnar styloid fracture should prompt an investigation for tears of the triangular fibrocartilage (TFC). The TFC extends from the rim of the sigmoid notch of the distal radius to the ulnar styloid and assists with stabilizing the distal radioulnar joint.
 Lateral view of the wrist demonstrates a Colles fracture. There is dorsal displacement and angulation of the principal distal fracture fragment.
Lateral view of the wrist demonstrates a Colles fracture. There is dorsal displacement and angulation of the principal distal fracture fragment.
PA and lateral radiographs constitute the minimal examination. The examiner should note the direction and severity of displacement and angulation, extent of comminution, intra-articular involvement (radiocarpal and/or distal radioulnar joint), and radial length or variance in comparison to the normal side.
Two popular distal radial fracture classification systems are described below: the Association for Osteosynthesis (AO) system and the Frykman system (see Tables 2 and 3).
Table 2. AO Classification of Distal Radius Fractures (Open Table in a new window)
Type |
Description |
A |
Extra-articular |
B |
Partial articular |
C 1 2 3 |
Complete articular Simple articular and metaphyseal fracture Simple articular with complex metaphyseal fracture Complex articular and metaphyseal fracture |
Table 3. Frykman Classification of Distal Radius Fractures (Open Table in a new window)
Type |
Radius |
Ulna |
Radiocarpal |
Radioulnar |
I |
Extra-articular |
Absent |
Absent |
Absent |
II |
Extra-articular |
Present |
Absent |
Absent |
III |
Intra-articular |
Absent |
Present |
Absent |
IV |
Intra-articular |
Present |
Present |
Absent |
V |
Intra-articular |
Absent |
Absent |
Present |
VI |
Intra-articular |
Present |
Absent |
Present |
VII |
Intra-articular |
Absent |
Present |
Present |
VIII |
Intra-articular |
Present |
Present |
Present |
The AO and Frykman classifications are useful in discussing prognosis.
Complications of the Colles fracture include compressive neuropathy, posttraumatic arthrosis, Volkmann ischemic contracture, acute carpal tunnel syndrome, and shoulder-hand syndrome. [20]
Colles fractures occur more frequently in elderly persons, as a result of osteoporosis. [21, 29]
Smith fracture
Robert Smith described the Smith fracture in 1847. An impact to the dorsum of the hand or a hyperflexion or hypersupination injury is thought to be the cause. A Smith fracture is usually called a reverse Colles fracture because the distal fragment is displaced volarly. It is often described as a garden-spade deformity. The ulnar head can be displaced dorsally (see images below).
 Lateral radiograph demonstrates volar displacement of the principal distal fracture fragment, described by Smith.
Lateral radiograph demonstrates volar displacement of the principal distal fracture fragment, described by Smith.
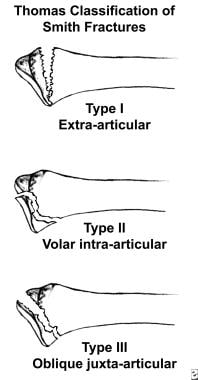
The criteria used to evaluate and describe Colles fractures also apply to Smith fractures. In 1957, F. Brian Thomas created the Thomas Classification of Smith fractures (see Table 4 and image below). [30]
Table 4. Thomas Classification of Smith Fractures (Open Table in a new window)
Type |
Description |
I |
Most stable, extra-articular, transverse distal radial fracture with volar and proximal displacement |
II |
Barton type, volar-lip fracture of the distal radius with volar and proximal dislocation of the carpus |
III |
Unstable, oblique, juxta-articular fracture of the distal radius with volar displacement and volar tilt of the distal radius |
The complications of Smith fractures are similar to those of Colles fractures.
Barton fracture
John Rhea Barton characterized the Barton fracture in 1838. [20] This fracture involves a dorsal rim injury of the distal portion of the radius. The volar Barton fracture is thought to occur with the same mechanism as the Smith fracture, with more force and loading on the wrist. The dorsal Barton fracture is caused by a fall onto an extended and pronated wrist, increasing carpal compression force on the dorsal rim. The salient feature is a subluxation of the wrist in this die-punch injury.
The Barton fracture involves either the volar or dorsal radial rim, and the mechanism is intra-articular. By definition, this fracture has some degree of carpal displacement. The volar variety is more common than the dorsal type. [20]
PA and lateral views of the wrist constitute the minimal examination. A true lateral projection is needed to evaluate the degree of carpal subluxation.
Wood and Berquist suggested that trispiral tomograms or coronal and/or sagittal CT could be used to evaluate articular congruity of the distal radius. [20]
Barton fractures are classified as dorsal or volar (always intra-articular), and they always involve carpal subluxation.
Complications of Barton fractures are similar to those of Colles fractures.
Hutchinson, chauffeur's, or radial styloid fracture
The chauffeur's fracture derives its name from injuries that were acquired in the days when motor vehicles were cranked, when a vehicle backfired. The force is described as a direct axial compression of the scaphoid into the radial facet. The radial styloid is fractured, with associated avulsion of the radial collateral ligament (see image below). [20, 28] A chauffeur's fracture represents an avulsion related to the attachment sites of the radiocarpal ligaments or of the radial collateral ligament. Scapholunate dissociation and lesser arc injuries of the wrist may be indicated by a fracture line on the radial articular surface between the scaphoid and lunate fossae.
 Oblique radiograph of a chauffeaur fracture. Note the fracture extending through the radial styloid.
Oblique radiograph of a chauffeaur fracture. Note the fracture extending through the radial styloid.
The PA view usually demonstrates the lesion. Wood and Berquist report that little or no abnormality is seen on lateral views. [20]
Chauffeur's fractures are classified as simple or comminuted radial styloid fractures and as displaced or nondisplaced fractures. These injuries show no evidence of carpal subluxation.
Complications include scapholunate dislocation, osteoarthritis, and ligamentous damage.
Galeazzi, or Piedmont, fracture
A Galeazzi fracture results from a FOOSH mechanism with the forearm hyperpronated, or from a direct impact to the dorsal radial wrist. The radial diaphysis at the distal and middle third junction is fractured, with associated subluxation/dislocation of the distal radioulnar joint. There may be resultant shortening of the radius.
PA views demonstrate the radial fracture and potentially subluxation/dislocation of the distal radioulnar joint. Distal radioulnar distances greater than 2 mm are suggestive of a ligamentous injury and/or a tear of the TFC.
The lateral view may be necessary to identify the distal radioulnar subluxation/dislocation. On the lateral view, the distal radius may be angulated volarly as a result of the pull of the brachioradialis muscle. [20]
An associated ulnar styloid fracture may be present.
Classification is based on the direction of displacement of the distal fracture fragment.
Complications include radial malunion, nonunion, and persistent subluxation of the radioulnar joint. [20]
Pediatric distal radial fracture
The distal one third of the forearm is the most common fracture site in children. Dicke notes that these represent 35.8-45% of all pediatric fractures. The primary mechanism of injury is a FOOSH. Unlike such falls in adults, these falls rarely lead to intra-articular fractures in children, but fractures can occur at the diaphyseal-metaphyseal junction or at the physis. Boys have a higher frequency of distal radial fractures than do girls.
Five classifications of pediatric fractures are used, as follows [31] :
-
Plastic deformation - This occurs most commonly in the ulna and fibula.
-
Buckle (torus) fracture - The diaphysis (cortical bone) causes the metaphysis to buckle under compressive forces.
-
Greenstick fracture - This fracture occurs when the tension side of the bone fails as it is bent.
-
Complete fracture - A complete fracture propagates through the entire bone and can occur as a spiral fracture, an oblique fracture, or a transverse fracture.
-
Physeal fracture - This fracture involves the growth plate. The distal radial physis is the most frequently injured physis.
Fractures involving the physis are categorized as follows, using the Salter-Harris (SH) classification:
-
Type I - A fracture through the physis.
-
Type II - A fracture through the physis and obliquely through the metaphysis.
-
Type III - A fracture through a portion of the physis and longitudinally through the epiphysis.
-
Type IV - An oblique fracture extending through the metaphysis, physis, and epiphysis.
A displaced pronator fat sign may be the only indication of a nondisplaced Salter-Harris type I fracture. Salter-Harris type II fractures are the most common, according to Waters, [32] reflecting 58% of the fractures considered in a study by Dicke.
Complications of pediatric distal radius fractures include nonunion or malunion, growth-plate arrest that leads to deformity, nerve and vessel damage, sympathetic dystrophy, overgrowth of the healing bone, and compartment syndrome.
Computed Tomography
Computed tomography (CT) is used to plan operative repair, providing improved accuracy for evaluation of fracture alignment and articular involvement. [17, 26] CT is also a useful modality for resolving uncertain findings on conventional radiographs, such as the presence of a potential radiographically occult fracture. In the postoperative setting, fracture healing can be assessed. Optimal results are obtained when sagittal and coronal reformatted images are used in conjunction with imaging in the axial plane (see images below).
 Coronal computed tomography (CT) scan demonstrates intra-articular radiocarpal joint involvement in a distal radial fracture.
Coronal computed tomography (CT) scan demonstrates intra-articular radiocarpal joint involvement in a distal radial fracture.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is not routinely used in the initial evaluation of acute distal radial fractures. However, the modality is useful in the assessment of additional bony, ligamentous, and soft-tissue abnormalities associated with distal radial fractures and may be helpful in detecting the radiographically occult distal radius fracture (see images below). [25]
 Posteroanterior radiograph of the wrist demonstrates a barely perceptible sclerotic fracture of the distal radial metaphysis.
Posteroanterior radiograph of the wrist demonstrates a barely perceptible sclerotic fracture of the distal radial metaphysis.
 T1-weighted MRI in the same patient exhibits the hypointense, nondisplaced fracture of the distal radial metaphysis.
T1-weighted MRI in the same patient exhibits the hypointense, nondisplaced fracture of the distal radial metaphysis.
 T2-weighted MRI of the wrist in the same patient exhibits linear bone marrow edema within the distal radial metaphysis corresponding to a sublte, and near radiographically occult, fracture.
T2-weighted MRI of the wrist in the same patient exhibits linear bone marrow edema within the distal radial metaphysis corresponding to a sublte, and near radiographically occult, fracture.
MRI is routinely used to evaluate the integrity of the intercarpal ligaments, the TFC, and the median nerve within the carpal tunnel when injury to these structures is suspected in conjunction with fracture of the distal radius.
Compared with radiographs and scintigrams, MRI may be more sensitive in detecting early posttraumatic osteonecrosis of the carpus that may occur with distal radius fractures.
The improved contrast resolution afforded by MRI improves the detection of marrow edema at the site of fracture, which is not detectable on CT scans.
Wood and Berquist quote a sensitivity of 100% and a specificity of 92% for MRI in the detection of TFC tears, compared to a sensitivity and specificity of 89% and 90%, respectively, for arthrography. [20]
Ultrasonography
Ultrasonography may be used in pediatric patients to visualize the physes of children in whom mineralization of secondary growth plates has yet to occur. Ultrasonography may also be used in patients who lack bony landmarks. On ultrasonograms, cortical surfaces are echogenic or echoreflective, whereas cartilage or unossified physes are sonolucent or hypoechoic. [33]
Ultrasound waves are almost completely reflected by cortical bone, and fractures easily appear on an ultrasound screen. The cartilaginous nature of pediatric bones makes some fractures difficult to identify on x-ray. The nature of ultrasound waves, however, allows the cartilaginous areas of pediatric bones to be identified. The ability of ultrasound to identify subperiosteal hematoma makes this procedure particularly valuable in the early recognition of possible abusive skeletal injury in children. [34]
Bianchi et al found that ultrasonography is an effective, dynamic, and noninvasive technique with which to diagnose and evaluate damage to the extensor tendons and their synovial sheaths. The authors analyzed ultrasound examinations of 9 consecutive patients with a history of distal radial fractures treated by open reduction and internal fixation of the volar plate. [35]
Poonai, et al reported that the sensitivity of point-of-care-ultrasound was 94.7% (95% confidence interval [CI] = 89.7-99.8) and specificity was 93.5% (95% CI = 88.6-98.5). In additiion, ultrasound was associated with low levels of pain and high caregiver satisfaction. [36]
Nuclear Imaging
Nuclear scintigraphy can be used to detect fractures because the early osteoblastic reaction at fracture margins results in a focal linear accumulation of technetium-99m (99mTc) methylene diphosphonate (MDP) at the site. However, reports describe poor accumulation of the radiotracer in patients with congestive heart failure or chronic renal failure and in the elderly. [33]
If bony, cartilaginous, or ligamentous abnormalities are suspected despite normal radiographs, radionuclide bone imaging may be helpful. An occult fracture or other osteochondral pathology must be excluded when an area of intense focal tracer accumulation is noted. Mildly increased focal tracer uptake suggests ligamentous or cartilaginous pathology. Lack of focal tracer accumulation on delayed images excludes osteochondral involvement.
Radionuclide bone imaging may be helpful in determining the age of a fracture and for documenting fracture healing when radiographic results are inconclusive. It is also important in the diagnosis of reflex sympathetic dystrophy (RSD).
Bone scintiscan findings may remain positive for as long as 2 years as a result of vascular recruitment from trauma. [33]
Metz and Gilula quote a sensitivity and specificity of 96% and 97%, respectively, in the diagnosis of RSD by using radionuclide bone imaging. [37]
-
Radial height (RH) is measured by drawing 2 parallel lines perpendicular to the long axis of the radius. Shortening of RH may indicate impaction of the distal radius when compared with a normal contralateral wrist. Ulnar variance (UV) is measured here by using the method of perpendiculars, in which 2 lines are drawn perpendicular to the long axis of the radius. One line is drawn on the ulnar-side articular surface of the radius, and the other is drawn on the ulnar carpal surface. This image demonstrates ulnar plus variance.
-
Posteroanterior view of an adult left wrist demonstrates an impacted distal radial fracture. Measurement of radial shortening and comparison with the contralateral normal wrist aids in the diagnosis.
-
The radial inclination is measured by drawing a line perpendicular to the long axis of the radius and a tangential line from the radial styloid to the ulnar corner of the lunate fossa.
-
The volar tilt, or palmar/volar inclination, is an angle between a line drawn perpendicular to the long axis of the radius and a tangential line drawn along the radial articular surface.
-
Lateral view of the wrist demonstrates a Colles fracture. There is dorsal displacement and angulation of the principal distal fracture fragment.
-
Illustration of the Thomas classification of Smith fractures.
-
Oblique radiograph of a chauffeaur fracture. Note the fracture extending through the radial styloid.
-
Posteroanterior view of the left wrist demonstrates buckle fractures of the distal radius and ulna.
-
Axial computed tomography (CT) scan demonstrates a comminuted distal radial fracture.
-
Coronal computed tomography (CT) scan demonstrates intra-articular radiocarpal joint involvement in a distal radial fracture.
-
Sagittal computed tomography (CT) scan demonstrates a comminuted distal radial fracture with intra-articular radiocarpal joint involvement.
-
Posteroanterior radiograph of the wrist demonstrates a barely perceptible sclerotic fracture of the distal radial metaphysis.
-
T1-weighted MRI in the same patient exhibits the hypointense, nondisplaced fracture of the distal radial metaphysis.
-
T2-weighted MRI of the wrist in the same patient exhibits linear bone marrow edema within the distal radial metaphysis corresponding to a sublte, and near radiographically occult, fracture.
-
Posteroanterior radiograph exhibiting a fracture of the distal radius.
-
Lateral radiograph demonstrates volar displacement of the principal distal fracture fragment, described by Smith.
-
Posteroanterior radiograph demonstrates a comminuted fracture of the distal radius. Note should be made of angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones.
-
Lateral radiograph demonstrates a comminuted fracture of the distal radius. Note should be made of angulation and displacement, intra-articular or extra-articular involvement, and associated anomalies of the ulnar or carpal bones.