Practice Essentials
Primary bone lymphoma (PBL) is a rare, malignant, neoplastic disorder of the skeleton. In 1939, it was described as a distinct clinical condition by Parker and Jackson. [1] Later that year, Ewing included it among the bone tumors listed in the Bone Sarcoma Registry, under the heading of reticulum cell lymphosarcoma. [2] In 1963, the term was introduced by Ivins and Dahlin. [3]
PBL accounts for only 1-5% of malignant lymphomas. [4, 5, 6] The majority of PBLs are diffuse large B-cell lymphomas (DLBCLs) and can occur in any bone, with the femur and the pelvis being the most common locations. [7, 5] The most common presentation of primary bone lymphoma consists of several months of bone pain and the appearance of a soft-tissue mass. Neurologic symptoms and fracture may also be present. [8] Treatment usually consists of a combination of chemotherapy and radiotherapy, with 5-year survival being 80-90%. [6]
A classic finding on imaging is a bone lesion with a soft-tissue component in which the cortical layer is preserved more than would be expected for an invasive lesion. MRI is the best imaging modality to identify the extent of involvement of adjacent compartments, and CT displays the cortical layer in greater detail. [9] On CT, the diagnosis of primary bone lymphoma should be considered whenever a large soft-tissue mass and abnormal bone marrow attenuation are seen without extensive cortical destruction that is proportional to the volume of the extraosseous lesion. [9]
According to the American College of Radiology (ACR), radiography is usually appropriate as the initial modality for evaluating suspected primary bone tumors. In cases where radiographs are negative or do not explain the symptoms, MRI with and without contrast is usually appropriate. Listed below are some of the ACRs most recent recommendations [10] :
-
Radiographs are usually appropriate for initial imaging of suspected primary bone tumors.
-
MRI without and with IV contrast, or MRI without IV contrast, is usually appropriate in patients who have positive symptoms for a suspected primary bone tumor but have negative radiographs. These procedures are equivalent alternatives; that is, only one procedure will be ordered to provide the clinical information to manage the patient’s care.
-
MRI without and with IV contrast, MRI without IV contrast, or CT without IV contrast may be appropriate for evaluating suspected primary bone tumor with benign lesions on radiographs, which is not osteoid osteoma. These procedures are equivalent alternatives; that is, only one procedure will be ordered to provide the clinical information to effectively manage the patient’s care.
-
CT without IV contrast is usually appropriate for a suspected primary bone tumor in patients who have radiographic findings or clinical presentations that suggest osteoid osteoma.
-
MRI without and with IV contrast is usually appropriate for a suspected primary bone tumor in patients who have indeterminate or aggressive-appearing lesions on radiographs that suggest malignancy.
-
Radiographs are usually appropriate to evaluate bone lesions that are incidentally found, and are not clearly benign, on MRI and CT.
After biopsy of the bone lesion confirms the diagnosis of lymphoma, CT scanning of the chest, abdomen, and pelvis is needed to exclude a primary, soft-tissue origin or distant disease. The CT scan may be combined with fluorodeoxyglucose (FDG) positron emission tomography (PET). Technetium-99m (99mTc) bone scintigraphy can also be used to look for additional sites of involvement that may be clinically silent. [11, 12, 13, 14] Once soft-tissue origin and distant disease are excluded, magnetic resonance imaging (MRI) is the preferred examination to stage the extent of disease within the affected bone. [15, 16]
Currently, few conventional angiograms are performed in the diagnostic imaging workup of primary bone tumors. Large feeding arteries or draining veins can be depicted with dynamic, contrast-enhanced CT scanning or MRI. Conventional angiographic findings are nonspecific. Lesions typically demonstrate hypervascular flow with tumor neovascularity, but they may be hypovascular or avascular. [17]
(See the images of bone lymphoma below.)
 A 57-year-old woman with knee pain. Lateral radiograph of the right lower leg reveals a large, permeative, lytic lesion with a moth-eaten appearance in the metadiaphysis of the tibia. Note the cortical destruction, aggressive periosteal reaction, and soft-tissue mass.
A 57-year-old woman with knee pain. Lateral radiograph of the right lower leg reveals a large, permeative, lytic lesion with a moth-eaten appearance in the metadiaphysis of the tibia. Note the cortical destruction, aggressive periosteal reaction, and soft-tissue mass.
 A 65-year-old man with right hip pain. Axial computed tomography (CT) scan demonstrates a destructive lesion of the right acetabular roof with multiple small sequestra and soft-tissue extension.
A 65-year-old man with right hip pain. Axial computed tomography (CT) scan demonstrates a destructive lesion of the right acetabular roof with multiple small sequestra and soft-tissue extension.
The 2020 World Health Organization classification of soft tissue and bone tumors officially refers to it as "primary non-Hodgkin lymphoma of bone" or "primary bone lymphoma" and recognizes the following 4 groups of lymphoma involving bone [18] :
-
A single primary bone site with or without regional nodes
-
Multiple bone sites but no visceral involvement
-
A bone lesion and involvement of multiple visceral or lymph node sites
-
Soft-tissue lymphoma, with bone involvement detected by bone biopsy or marrow aspirate
This author would consider only groups 1 and 2 to represent primary bone lymphoma. Groups 3 and 4 would most likely represent metastatic involvement of bone.
Kim et al have noted the following as criteria for primary bone marrow lymphoma [19] :
-
Pathological evidence of isolated bone marrow infiltration regardless of peripheral blood involvement.
-
Absence of nodal or extranodal involvement.
-
No evidence of tumor formation.
-
No evidence of bony trabecular destruction on bone marrow biopsy.
-
Exclusion of leukemia/lymphoma that involves the bone marrow, such as chronic lymphocytic leukemia/small lymphocytic leukemia.
Radiography
Because primary bone lymphoma (PBL) is one of the least common primary skeletal malignancies and varies widely in appearance on conventional radiographs, a confident diagnosis based on initial radiographs usually is not possible.
In a review of 237 cases, Mulligan and colleagues listed the most common radiographic features, which included those listed below [20] :
-
Permeative, lytic pattern of bone destruction (74%)
-
Metadiaphyseal location (69%)
-
Periosteal reaction (58%)
-
Soft-tissue mass (80-100%)
(See the images below.)
 A 57-year-old woman with knee pain. Lateral radiograph of the right lower leg reveals a large, permeative, lytic lesion with a moth-eaten appearance in the metadiaphysis of the tibia. Note the cortical destruction, aggressive periosteal reaction, and soft-tissue mass.
A 57-year-old woman with knee pain. Lateral radiograph of the right lower leg reveals a large, permeative, lytic lesion with a moth-eaten appearance in the metadiaphysis of the tibia. Note the cortical destruction, aggressive periosteal reaction, and soft-tissue mass.
 A 5-year-old girl with left leg pain. Anteroposterior radiograph of the lower legs demonstrates a permeative, lytic lesion in the metadiaphysis of the left tibia. Note the aggressive periosteal reaction with Codman triangles and soft-tissue extension/swelling. Soft-tissue involvement is easy to appreciate when the left leg is compared with the normal right leg.
A 5-year-old girl with left leg pain. Anteroposterior radiograph of the lower legs demonstrates a permeative, lytic lesion in the metadiaphysis of the left tibia. Note the aggressive periosteal reaction with Codman triangles and soft-tissue extension/swelling. Soft-tissue involvement is easy to appreciate when the left leg is compared with the normal right leg.
 Variant appearance. A 20-year-old man with left leg pain. Lateral radiograph of the left lower leg reveals a well-circumscribed, geographic, lytic lesion in the tibial metadiaphysis. Note the absence of cortical destruction, lack of periosteal reaction, and lack of soft-tissue extension.
Variant appearance. A 20-year-old man with left leg pain. Lateral radiograph of the left lower leg reveals a well-circumscribed, geographic, lytic lesion in the tibial metadiaphysis. Note the absence of cortical destruction, lack of periosteal reaction, and lack of soft-tissue extension.
 Variant appearance. A 45-year-old man with right hip pain. Anteroposterior radiograph of the right hip demonstrates a large, expansile, aneurysmal, lytic lesion in the iliac wing.
Variant appearance. A 45-year-old man with right hip pain. Anteroposterior radiograph of the right hip demonstrates a large, expansile, aneurysmal, lytic lesion in the iliac wing.
Detection of a soft-tissue mass depends on the type of imaging modality used. CT scanning and MRI are more sensitive than are conventional radiographs (see the images below).
 A 65-year-old man with right hip pain. Axial computed tomography (CT) scan demonstrates a destructive lesion of the right acetabular roof with multiple small sequestra and soft-tissue extension.
A 65-year-old man with right hip pain. Axial computed tomography (CT) scan demonstrates a destructive lesion of the right acetabular roof with multiple small sequestra and soft-tissue extension.
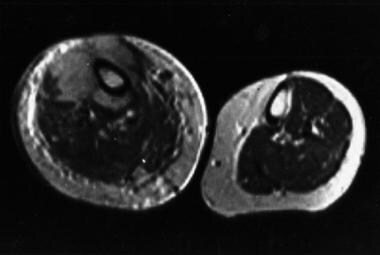 A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
The range of appearances is broad, including the following:
-
Some patients (< 5%) present with no detectable abnormal findings on initial conventional radiographs.
-
Some patients (11%) demonstrate focal geographic lesions that may have a mixed or blastic appearance.
-
The location can be epiphyseal, metaphyseal, or diaphyseal.
-
Primary intracortical and periosteal lesions have been reported.
-
Typical lesions occasionally are large enough for patients to present with pathologic fracture (22%).
-
Periosteal reaction varies, ranging from a single, continuous layer to interrupted multiple layers. Interrupted single or multiple layers were the most common type of periosteal reaction (52%) found in the study referenced above.
Sequestrum formation is a feature of PBL that can help differentiate it from most other diagnostic possibilities, because sequestra typically are not observed in conditions such as metastatic disease and myeloma. Sequestra have been reported in 11-16% of patients with PBL. [21]
Another uncommon feature of PBL is involvement of adjacent bones (4%) by extension across the joint space.
Computed Tomography
Cross-sectional imaging studies are useful adjuncts to conventional radiographs in PBL. One pattern of involvement observed with either CT scanning or MRI is specific for round cell tumors, such as PBL.
The pattern appears as extensive evidence of disease within the marrow cavity associated with a surrounding soft-tissue mass but without extensive cortical destruction (see the image below). This pattern has been reported only in PBL, Ewing sarcoma, and myeloma. However, in one report, 31% of cases had a nonaggressive appearance by MRI.15 When the pattern of involvement described is demonstrated on CT or MRI scans, the degree of confidence is high that the process is one of the round cell tumors. The pattern is not specific for individual entities.
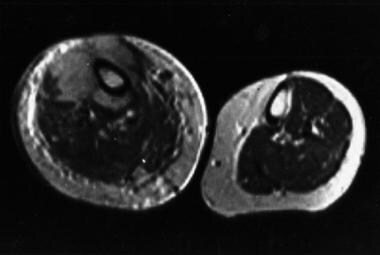 A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
Magnetic Resonance Imaging
MRI signal intensities are nonspecific, with the signal typically lower than muscle on T1-weighted sequences and higher or brighter than muscle on T2-weighted sequences. These tumors are usually treated with radiation therapy, and in that setting, it is not necessary to define a precise surgical margin; thus, intravenous (IV) contrast (ie, gadolinium) usually is not administered. These tumors typically demonstrate diffuse heterogeneous to homogeneous enhancement when IV contrast is used, and it may be needed when surgery is to be employed for local control. (See the image below.)
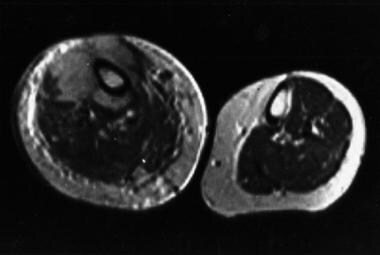 A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). NSF has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Nuclear Imaging
Bone scintigraphy with technetium-99m (99mTc) may be performed as part of the initial workup when considering other diagnoses, especially metastatic disease. In one study of PBL, 64% of patients had a marked increase in uptake of 99mTc in the solitary lesion.
Bone scintigraphy is more sensitive than conventional radiography. The pattern of extensive abnormality within a bone on a bone scan, accompanied by normal findings on conventional radiographs, suggests a round cell tumor, such as primary bone lymphoma (PBL) (see the image below). A scintigraphic pattern that is suggestive of multifocal PBL is reported to be a combination of lesions in the skull, distal femur, and proximal tibia. Of the patients described in a report by Melamed and colleagues, 5 out of 8 demonstrated this pattern of involvement. [22] Patients with multifocal disease often also have spinal column involvement.
 Typical scintigraphic appearance. A 65-year-old woman with right leg pain. Whole-body image from technetium-99m (99mTc) bone scan reveals a solitary area of intensely increased tracer uptake suggestive of Paget disease. An old left rib fracture and degenerative changes in both hands are evident.
Typical scintigraphic appearance. A 65-year-old woman with right leg pain. Whole-body image from technetium-99m (99mTc) bone scan reveals a solitary area of intensely increased tracer uptake suggestive of Paget disease. An old left rib fracture and degenerative changes in both hands are evident.
Gallium-67 (67Ga) citrate and thallium-201 (201Tl) are also positive in patients with PBL. Whole-body 67Ga scanning can help with initial staging by identifying or excluding soft-tissue foci of disease. Ga-67 scanning also may be more helpful than other imaging modalities when determining the response of the tumor to the clinical treatment. Fluorodeoxyglucose positron emission tomography (FDG-PET) is also useful for initial staging and follow-up.
Findings are not specific, but the pattern of uptake helps limit the differential diagnosis. Only a few conditions reveal a marked uptake increase with bone scintigraphy, including Paget disease, fibrous dysplasia, and osteosarcoma. Because most cases of PBL demonstrate increased uptake with bone scanning, one may be able to exclude plasmacytoma or multiple myeloma from consideration, because the latter conditions usually do not show significant increased uptake with 99mTc.
-
A 57-year-old woman with knee pain. Lateral radiograph of the right lower leg reveals a large, permeative, lytic lesion with a moth-eaten appearance in the metadiaphysis of the tibia. Note the cortical destruction, aggressive periosteal reaction, and soft-tissue mass.
-
A 65-year-old man with right hip pain. Axial computed tomography (CT) scan demonstrates a destructive lesion of the right acetabular roof with multiple small sequestra and soft-tissue extension.
-
A 70-year-old woman with right leg pain. Conventional radiographic findings were normal. Axial, T2-weighted magnetic resonance imaging (MRI) through the lower legs at the level of the tibial tubercle reveals an abnormal low signal within the medullary canal and a large soft-tissue mass surrounding the right tibia. Note the intact cortex on the right and the normal medullary signal and soft tissues on the left.
-
A 5-year-old girl with left leg pain. Anteroposterior radiograph of the lower legs demonstrates a permeative, lytic lesion in the metadiaphysis of the left tibia. Note the aggressive periosteal reaction with Codman triangles and soft-tissue extension/swelling. Soft-tissue involvement is easy to appreciate when the left leg is compared with the normal right leg.
-
Variant appearance. A 20-year-old man with left leg pain. Lateral radiograph of the left lower leg reveals a well-circumscribed, geographic, lytic lesion in the tibial metadiaphysis. Note the absence of cortical destruction, lack of periosteal reaction, and lack of soft-tissue extension.
-
Variant appearance. A 45-year-old man with right hip pain. Anteroposterior radiograph of the right hip demonstrates a large, expansile, aneurysmal, lytic lesion in the iliac wing.
-
Variant location. A 51-year-old man with left leg pain. Lateral radiograph demonstrates a lytic lesion with a moth-eaten appearance centered in the middiaphysis of the tibia.
-
Typical scintigraphic appearance. A 65-year-old woman with right leg pain. Whole-body image from technetium-99m (99mTc) bone scan reveals a solitary area of intensely increased tracer uptake suggestive of Paget disease. An old left rib fracture and degenerative changes in both hands are evident.







