Practice Essentials
Fractures of the thoracic spine may be seen in patients of any age, but in elderly patients, the frequency and severity of thoracic spinal fractures is increased. Fractures of the thoracic spine can occur whenever the spinal column is subjected to forces that exceed its strength and stability. Common causes of thoracic spinal fractures include falling from a height, motor vehicle accidents, violent weather, military and civilian blast injury, and penetrating trauma. Less common injury patterns may be related to sports injuries. The older patient presents an increased challenge because thoracic spinal fractures may occur following relatively minor falls. After aortic rupture, severe thoracic spinal cord injuries represent the most serious long-term morbidities resulting from thoracic trauma. [1, 2, 3, 4, 5, 6] Delayed diagnoses of unstable thoracolumbar spinal fractures can result in neurologic deficits and avoidable pain. [7, 8, 9, 10]
(See the images below.)
 Thoracic spine trauma. Anterior view of multiple spinal cord contusions caused by burst compression fractures of the middle and lower thoracic spine.
Thoracic spine trauma. Anterior view of multiple spinal cord contusions caused by burst compression fractures of the middle and lower thoracic spine.
The goals of diagnostic imaging in patients who have sustained thoracic spinal trauma are to correctly identify spinal fractures, to identify associated injuries to structures that are related to the thoracic spine, to identify injuries to the spinal cord and nerve roots, to aid in surgical planning, and to judge the stability of postoperative fixation.
In cases of multiple system trauma, thoracic spinal fractures may be first discovered during the performance of CT of the chest and abdomen. Some authors have advocated a careful review of the axial CT images obtained in the typical CT trauma series without the additional use of thin-section reformatted images. [11] Computed tomography has been found to be superior to plain films in the detection of thoracolumbar spinal fractures. [7, 8, 9, 10]
In a study by Gross, the reformatting of chest CT scans and abdominopelvic CT scans were shown to provide improved sensitivity in detecting thoracic and lumbar spine fractures. There were 176 abdominopelvic CT scans with reformatting and 175 chest CT scans with reformatting. In the study, there were 9 of 176 false-negative abdominopelvic CT scans, versus 3 of 176 false-negative lumbar spine CT scans, and there were 14 of 175 false-negative chest CT scans, versus 2 of 175 false-negative thoracic spine CT scans. According to the authors, the differences in sensitivity were significant for both comparisons. [12]
In general, anteroposterior (AP) and lateral radiographs should be obtained in the emergency department while other measures of resuscitation are performed. Multidetector CT scans with intravenous contrast enhancement are indicated in most patients to exclude intrathoracic vascular injury. In patients who have sustained blunt trauma, multidetector CT has been proposed as a screening study for thoracolumbar fracture. [13, 14, 15]
MRI of the thoracic spine should be reserved for patients with neurologic deficits or patients with spinal canal compromise who are unable to provide a full neurologic history. MRI of the thoracic region provides important information concerning the spinal cord and the dural structures. [16, 7] Because MRI is useful in evaluating soft-tissue injury to the ligaments, disks, and epidural space, it is helpful in cases where traumatic disk herniation, epidural hematoma, or spinal cord injury (SCI) is suspected. [17]
(Note the images below.)
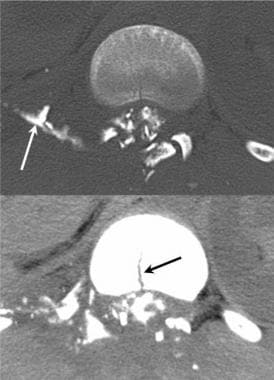 Thoracic spine trauma. Axial CT myelogram in a patient with a gunshot wound to the thoracic spine. While a fracture is obvious, the injury also resulted in a dural tear with a freely leaking cerebrospinal fluid space (white arrow). The midline fracture of the vertebral body is noted in the lower image (black arrow).
Thoracic spine trauma. Axial CT myelogram in a patient with a gunshot wound to the thoracic spine. While a fracture is obvious, the injury also resulted in a dural tear with a freely leaking cerebrospinal fluid space (white arrow). The midline fracture of the vertebral body is noted in the lower image (black arrow).
 Thoracic spine trauma. Axial CT image demonstrates a complex fracture of the T12 with rotation subluxation. Air was introduced into the epidural space during the injury.
Thoracic spine trauma. Axial CT image demonstrates a complex fracture of the T12 with rotation subluxation. Air was introduced into the epidural space during the injury.
Patients with osteoporotic vertebral fractures may require a comprehensive approach to spinal imaging. [18]
Many patients who present with thoracic injury have a pulmonary, rib, or vascular injury. Most patients who have sustained multiple system trauma will have had a CT of the chest and abdomen as part of their evaluation. Pregnant women should be imaged carefully while limiting radiation exposure if possible. [19] The expense and delay of obtaining routine CT scans of the thoracic spine are not justified in all cases. Focused CT scans should be performed if patients have unexplained thoracic back pain or neurologic symptoms.
A review of the bone windows of thoracic CT scans indicates most major deformities associated with Chance fracture, distraction injury, and burst vertebral fractures. The more complex injuries can be studied later if necessary. Multisectional axial CT of the thoracic region should be reformatted to examine the thoracic spine in a lateral (sagittal) view.
The application of MRI in spinal trauma should be linked to an abnormality of the neurologic examination or to an evaluation of unexplained severe spinal pain.
Pathophysiology
Compression fractures of the thoracic spine occur when a vertical force with or without a flexion or rotational sheer force exceeds the weight-bearing strength of the vertebral body. Various diseases, advanced age, and other comorbidities may make compression fractures more likely.
Fractures associated with subluxation or dislocation are more commonly the result of high-velocity blunt trauma with an element of flexion or rotational stress. In cases associated with unusual causes of spinal injury, such as child abuse, the mechanism of injury may be a complex combination of traumas to the thoracic spine. A high index of suspicion of abuse can help identify occult spinal fractures in younger patients. [20]
In patients with ankylosing spondylitis, the incidence of thoracic spinal fractures is increased but the patterns of spinal fracture are unusual. Fractures in patients with ankylosing spondylitis are most commonly linear and horizontal in orientation. [21]
Multiple myeloma commonly involves the thoracic spine, and fractures are more common. The surgical repair of fractures of the thoracic spine in patients with multiple myeloma is complicated by the multicentric nature of the disease. [22]
Epidemiology
Thoracic spinal fractures remain a common component of trauma in the United States and in other developed nations with high rates of motor vehicle accidents. [23, 24] Mortality due to motor vehicle traffic accidents have declined, [25] primarily because of better traffic conditions and improved emergency trauma services. During that same period, the number of deaths due to falls from a height increased.
In a study of thoracolumbar spinal injuries in pediatric patients, by Habermehl et al, thoracolumbar spinal injuries occurred more commonly in 16- to 17-year-olds (45.7%), and the injuries were often sustained from a motor vehicle accident (55.2%) and resulted in an injury to bone (82.3%). [9]
Mechanical CPR devices have been identified as an unusual cause of thoracic spinal fractures. [26]
The incidence of pathologic fractures due to osteoporosis is somewhat lower in black women than in persons of other races and greater in elderly women
Mortality/morbidity
Mortality associated with thoracic spinal fractures is most commonly related to injuries associated with aortic tear or rupture and cardiac trauma. Short-term morbidity is complicated by pulmonary disease and shock. Long-term morbidity among spinal fracture patients includes paralysis, sepsis, and the need for spinal stabilization. The means of aortic repair may include endovascular repair versus open surgical graft placement. The timing and nature of spinal fracture fixation is subject to regional and individual opinion. [27, 28, 29, 30]
The timing of surgical repair of a thoracic spinal fracture may make a difference in clinical outcome. [31]
In a study of 198 patients with thoracic spinal fractures, by Bizimungu et al, 62% had associated injuries and an 88.5% admission rate. Less than half of the fractures were considered clinically significant, and 40.8% of patients received thoracolumbosacral orthosis bracing, 10.9% underwent surgery, and 3.8% had an associated neurologic deficit. [32]
Anatomy
There are 12 thoracic vertebral bodies in the majority of people. The typical thoracic vertebral segment consists of a thoracic vertebral body, right and left transverse processes, a single posterior spinous process, and a right and left superior and inferior facet surface linked to the vertebral body by a pedicle. Each of the thoracic vertebral bodies is linked by the anterior longitudinal ligament, the posterior longitudinal ligament, the ligament flava, and the interspinal ligaments. The typical thoracic vertebral body has facet surfaces for the articulation of a right and left rib. The intervertebral distances between the thoracic vertebral bodies are less than the lumbar segments.
A thoracic nerve named for the vertebral segment exits laterally at the same numbered level. Each thoracic nerve root is formed from a ventral and a dorsal nerve root. A dorsal root ganglion is located inferior to the vertebral pedicle of the same number.
While most people have 12 ribs, the 12th rib may be rudimentary. Each rib is attached to the vertebral body by 2 joint cavities. The lateral costotransverse ligament, the articular capsule, the superior costotransverse ligament, and the intra-articular ligament provide flexible stability between the transverse process and the rib facets.
(Depictions of the anatomy of the thoracic spine and vertebra are provided in the images below.)
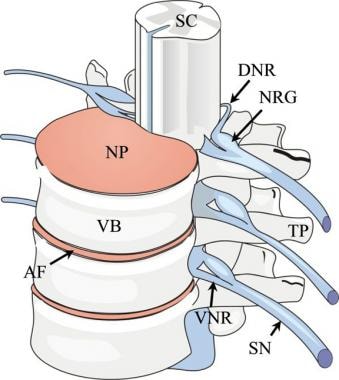 Thoracic spine trauma. Drawing of the thoracolumbar spine viewed from an oblique frontal projection. SC indicates the spinal cord; NP, nucleus pulposus; VB, vertebral body; AF, annulus fibrosis; VNR, ventral nerve root; SN, spinal nerve; TP, transverse process; DNR, dorsal nerve root; and NRG, nerve root ganglion.
Thoracic spine trauma. Drawing of the thoracolumbar spine viewed from an oblique frontal projection. SC indicates the spinal cord; NP, nucleus pulposus; VB, vertebral body; AF, annulus fibrosis; VNR, ventral nerve root; SN, spinal nerve; TP, transverse process; DNR, dorsal nerve root; and NRG, nerve root ganglion.
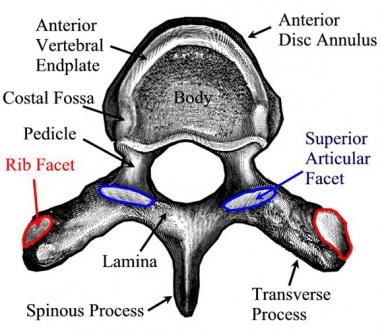 Thoracic spine trauma. Axial drawing of a typical thoracic vertebral body viewed from above. The thoracic vertebral bodies are unique in that ribs articulate by rib facets (red outline and red arrow) with the correspondingly numbered vertebrae. The superior articular facet (outlined in blue, blue arrow) is oriented along a lateral plane.
Thoracic spine trauma. Axial drawing of a typical thoracic vertebral body viewed from above. The thoracic vertebral bodies are unique in that ribs articulate by rib facets (red outline and red arrow) with the correspondingly numbered vertebrae. The superior articular facet (outlined in blue, blue arrow) is oriented along a lateral plane.
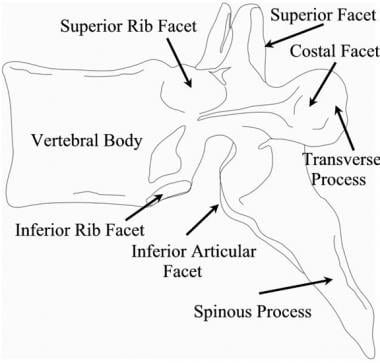 Thoracic spine trauma. Drawing of a typical thoracic vertebral body viewed in a lateral projection. The superior rib facet, semilunar inferior rib facet and the costal facet provide articulation for the ribs. The articular facet surfaces are oriented laterally. The spinous processes of the upper and mid thoracic vertebrae are angulated caudally.
Thoracic spine trauma. Drawing of a typical thoracic vertebral body viewed in a lateral projection. The superior rib facet, semilunar inferior rib facet and the costal facet provide articulation for the ribs. The articular facet surfaces are oriented laterally. The spinous processes of the upper and mid thoracic vertebrae are angulated caudally.
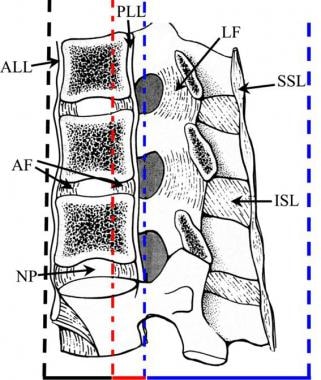 Thoracic spine trauma. Sagittal drawing of the thoracic spine demonstrating the structures that comprise the anterior, middle, and posterior columns. ALL indicates the anterior longitudinal ligament; AF, annulus fibrosus; NP, nucleus pulposus; PLL, posterior longitudinal ligament; SSL, supraspinous ligament; LF, ligamentum flavum; and ISL, interspinous ligament. Lateral drawing of the 3 spinal columns of the thoracolumbar junction. The anterior column is indicated by the black dotted line and includes the anterior spinal ligament, the anterior annulus fibrosis and the intervertebral disk, and the anterior two thirds of the vertebral bodies. The middle column (red dotted line) includes the posterior aspect of the vertebral bodies, the posterior annulus fibrosis, and the posterior longitudinal ligament. The posterior column (blue dotted line) includes all of the spine posterior to the longitudinal ligament (thick blue dotted line).
Thoracic spine trauma. Sagittal drawing of the thoracic spine demonstrating the structures that comprise the anterior, middle, and posterior columns. ALL indicates the anterior longitudinal ligament; AF, annulus fibrosus; NP, nucleus pulposus; PLL, posterior longitudinal ligament; SSL, supraspinous ligament; LF, ligamentum flavum; and ISL, interspinous ligament. Lateral drawing of the 3 spinal columns of the thoracolumbar junction. The anterior column is indicated by the black dotted line and includes the anterior spinal ligament, the anterior annulus fibrosis and the intervertebral disk, and the anterior two thirds of the vertebral bodies. The middle column (red dotted line) includes the posterior aspect of the vertebral bodies, the posterior annulus fibrosis, and the posterior longitudinal ligament. The posterior column (blue dotted line) includes all of the spine posterior to the longitudinal ligament (thick blue dotted line).
 Thoracic spine trauma. Twelve similar thoracic vertebral bodies form the thoracic spine. A rib is attached to each of the vertebral bodies of the same number. The mild kyphosis of the thoracic spine occurs due to the slightly wedged shape of the anterior thoracic vertebral bodies.
Thoracic spine trauma. Twelve similar thoracic vertebral bodies form the thoracic spine. A rib is attached to each of the vertebral bodies of the same number. The mild kyphosis of the thoracic spine occurs due to the slightly wedged shape of the anterior thoracic vertebral bodies.
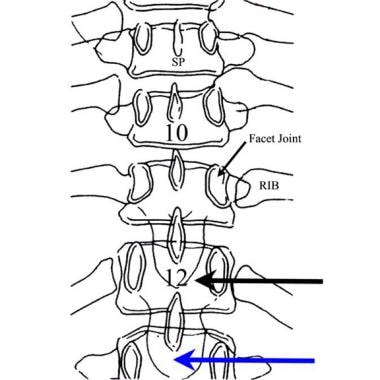 Thoracic spine trauma. Posterior drawing of the lower thoracic spine. The last rib usually is attached to the 12th thoracic vertebral body. Each thoracic vertebral body articulates with a rib. The facet joints of the thoracic region are oriented in an anterior to posterior direction. The first lumbar vertebral body (blue arrow) is similar to the last thoracic vertebral body (black arrow) except for the absence of a rib at T12.
Thoracic spine trauma. Posterior drawing of the lower thoracic spine. The last rib usually is attached to the 12th thoracic vertebral body. Each thoracic vertebral body articulates with a rib. The facet joints of the thoracic region are oriented in an anterior to posterior direction. The first lumbar vertebral body (blue arrow) is similar to the last thoracic vertebral body (black arrow) except for the absence of a rib at T12.
 Thoracic spine trauma. Lateral drawing the spine with the natural spinal curves shown by a curved line. A normal lordotic curve of the cervical spine, a mild kyphosis of the thoracic spine, and lordosis of the lumbar region are noted. These curves act to distribute the vertical weight-bearing load most efficiently.
Thoracic spine trauma. Lateral drawing the spine with the natural spinal curves shown by a curved line. A normal lordotic curve of the cervical spine, a mild kyphosis of the thoracic spine, and lordosis of the lumbar region are noted. These curves act to distribute the vertical weight-bearing load most efficiently.
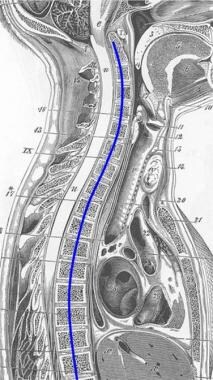 Thoracic spine trauma. The natural lordotic curvature of the cervical spine is reversed in the upper thoracic spine to form a kyphosis in the T1-T2-T3 segments in most adults.
Thoracic spine trauma. The natural lordotic curvature of the cervical spine is reversed in the upper thoracic spine to form a kyphosis in the T1-T2-T3 segments in most adults.
Clinical details
The Denis classification is considered clinically useful in the description of spinal fractures. Although the Denis classification provides a useful framework for describing the initial bony injury and the neurologic deficits, neurologic recovery has been reported to have a poor correlation. [33]
The differential diagnosis includes aortic dissection, blunt chest trauma, thoracic aortic aneurysm, thoracic disc injuries, and thoracic discogenic pain syndrome.
The initial evaluation of a patient with a thoracic spinal fracture should account for a possible multisystem trauma pattern (polytrauma). In such cases, possible cranial, abdominal, pelvic, and extremity injuries must be managed. The challenge for the radiologist in polytrauma is to effectively manage the large amount of information obtained by multiple radiographs, CT studies, and MRI scans.
Guidelines
Guidelines for the evaluation and treatment of thoracic and lumbar spinal fractures have been published by the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Section on Dis. These guidelines support the use of MRI in clinical decision-making but found insufficient evidence to recommend radiographic studies for predication of clinical outcomes. [34]
AOSpine (a part of AO [Arbeitsgemeinschaft für Osteosynthesefragen]) published a series of systematic review articles in the Global Spine Journal aimed at providing evidence-based guidelines for the management of spinal cord injuries (SCIs). The guidelines recommended performing MRI in adult patients with acute SCIs before surgical intervention when possible to aid in clinical decision-making. They also recommended that MRI be performed before or after surgery to improve prediction of the neurologic prognosis. However, the level of evidence for both of these recommendations was low. [35]
Radiography
Radiographic features of an anterior compression (wedge) fracture include soft tissue swelling, anterior superior cortical impaction, loss of vertical height of the anterior vertebral body, buckling of the anterior cortex of the vertebral body, trabecular compaction, endplate fractures, and disk-space narrowing.
(The radiographic images below display various thoracic spinal traumatic injuries.)
 Thoracic spine trauma. Lateral radiograph of the thoracic spine of a 74-year-old woman. The kyphosis of the thoracic spine is related to osteoporotic failure of the T8 vertebral body. Note the 30-40% wedge-shaped deformity of the T8 vertebra.
Thoracic spine trauma. Lateral radiograph of the thoracic spine of a 74-year-old woman. The kyphosis of the thoracic spine is related to osteoporotic failure of the T8 vertebral body. Note the 30-40% wedge-shaped deformity of the T8 vertebra.
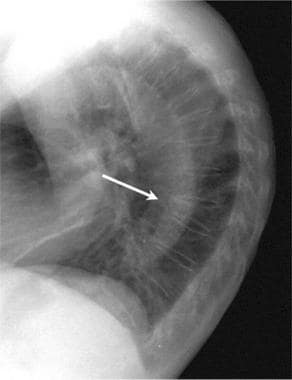
 Thoracic spine trauma. Anteroposterior view radiograph of the lumbar spine demonstrates a narrowed T12 vertebral body height (arrow) consistent with a compression fracture.
Thoracic spine trauma. Anteroposterior view radiograph of the lumbar spine demonstrates a narrowed T12 vertebral body height (arrow) consistent with a compression fracture.
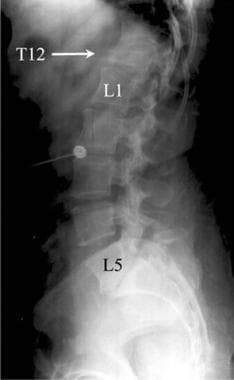 Thoracic spine trauma. Lateral radiograph of the lumbar spine. In the upper portion of the lumbar radiograph, a T12 compression fracture (arrow) is demonstrated. Superimposed lung and rib shadows make full depiction of the fracture difficult.
Thoracic spine trauma. Lateral radiograph of the lumbar spine. In the upper portion of the lumbar radiograph, a T12 compression fracture (arrow) is demonstrated. Superimposed lung and rib shadows make full depiction of the fracture difficult.
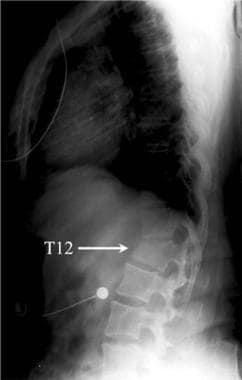 Thoracic spine trauma. Lateral radiograph of the thoracic spine with compression fracture (arrow) centered in the image. The radiograph demonstrates a 40% anterior compression of the vertebral body.
Thoracic spine trauma. Lateral radiograph of the thoracic spine with compression fracture (arrow) centered in the image. The radiograph demonstrates a 40% anterior compression of the vertebral body.
 Thoracic spine trauma. Lateral radiograph of the lumbar spine in a patient with chronic renal disease. Metabolic bone disease, such as renal osteodystrophy (arrow), results in more frequent and more severe compression fractures.
Thoracic spine trauma. Lateral radiograph of the lumbar spine in a patient with chronic renal disease. Metabolic bone disease, such as renal osteodystrophy (arrow), results in more frequent and more severe compression fractures.
Among the more serious injuries of the thoracic spine, the burst fracture usually is detected easily by using standard radiographs of the thoracic spine. In the lateral view, the criteria for instability include a greater than 50% loss of vertebral body height, a greater than 20° angulation of the thoracolumbar junction (normal is 0°), neurologic injury, and a canal narrowing of greater than 30%. Early surgical repair is indicated for such an injury because additional compression of the fracture and more severe neurologic injury can be expected if weight bearing is attempted without surgical fixation.
Degree of confidence
The degree of confidence in the initial identification of thoracic spine fractures is related directly to the severity of the spinal deformity and inversely related to technical factors such as the size of the patient, patient movement, and the type of radiologic equipment available.
The degree of compression and changes in the disk interspaces are important factors that help in determining if a compression fracture is clinically significant. A compression with intervertebral disk narrowing of more than 50% has a less favorable prognosis for successful treatment. Beyond acute trauma, anterior wedge fractures are subject to differential diagnostic considerations that include congenital hemivertebra, infections, primary tumors, metastatic tumors, metabolic bone disease, Scheuermann disease, Kummell disease, and Schmorl nodes.
False positives/negatives
Many spinal anomalies may be mistaken for a fracture. Horizontal residual venous sinus grooves may appear as suspected fractures. In young children, the anterior corners of the vertebral body may have a small depression, which represents the epiphyseal margin. The ossification centers at the ends of transverse processes may appear as fractures. Ossification centers may be irregular in appearance without pathologic fractures. Spina bifida occulta may occur in the posterior spine at any level. The body of T12 is often slightly wedged anteriorly, described as physiologic wedging.
Asymmetry of the pedicles of the lower thoracic spine has been reported in 7% of persons without spinal fracture. The best interobserver agreement can be obtained by measuring from the superior endplate of the vertebral body one level above the injured vertebral body to the inferior endplate of the vertebral body one level below.
A congenital butterfly vertebral body appears as a compression fracture viewed in the lateral projection. Superimposed shadows of the glenoid process of the scapula may give a false impression of a compression fracture when viewed in the lateral projection, whereas the outline of the mandible may suggest a fracture in an anterior view. False-positive findings can result from previous (chronic) kyphosis due to osteoporosis or prior injury. Kyphosis after trauma is best compared by using prior lateral radiographs if such images are available.
Computed Tomography
Thin-section axial CT performed by using a bone algorithm is the single most sensitive means by which to diagnose fractures of the thoracic spine. Routine helical CT scans of the thoracic spine are valuable because multisection CT scanners can generate high-resolution spinal images, even during a primary multisystemic trauma evaluation. [13, 14, 36, 37]
(The CT images below display various thoracic spinal traumatic injuries.)
 Thoracic spine trauma. Lateral 3-dimensional maximum intensity projection CT scan of multiple upper thoracic and lower cervical spinous process fractures. The force necessary to fracture the spinous processes of the upper thoracic spine may also involve the lower cervical spine.
Thoracic spine trauma. Lateral 3-dimensional maximum intensity projection CT scan of multiple upper thoracic and lower cervical spinous process fractures. The force necessary to fracture the spinous processes of the upper thoracic spine may also involve the lower cervical spine.
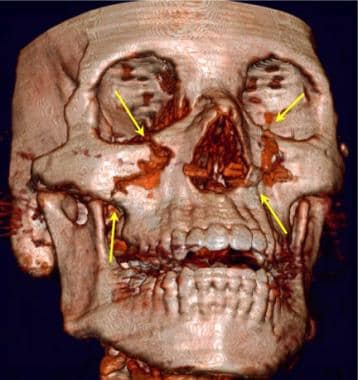 Thoracic spine trauma. Three-dimensional CT scan of complex midface fractures including a Le Fort I injury in a patient who had fractures of the upper thoracic and lower cervical spinous processes. Sudden deceleration of the face and skull resulted in severe stress forces on the spinous processes.
Thoracic spine trauma. Three-dimensional CT scan of complex midface fractures including a Le Fort I injury in a patient who had fractures of the upper thoracic and lower cervical spinous processes. Sudden deceleration of the face and skull resulted in severe stress forces on the spinous processes.
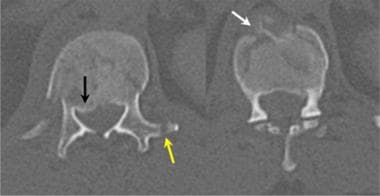 Thoracic spine trauma. Axial CT scan of a T12 compression fracture demonstrates a fracture line through the anterior body of the T12 (white arrow), posterior displacement of the T12 vertebral endplate (black arrow) into the spinal canal, and a fracture of the left transverse spinous process.
Thoracic spine trauma. Axial CT scan of a T12 compression fracture demonstrates a fracture line through the anterior body of the T12 (white arrow), posterior displacement of the T12 vertebral endplate (black arrow) into the spinal canal, and a fracture of the left transverse spinous process.
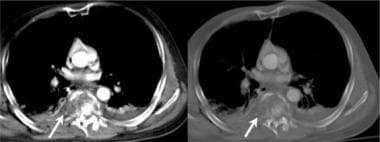
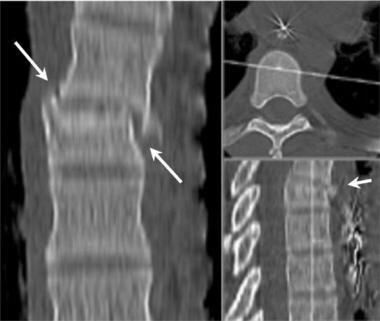
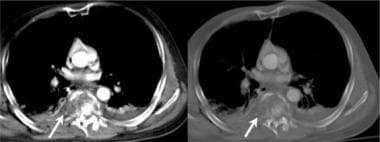
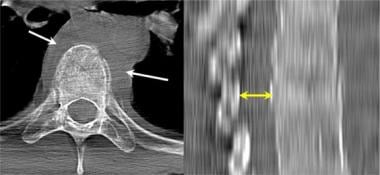 Thoracic spine trauma. Axial and sagittal CT images of an acute lower thoracic spine compression fracture. Note the paraspinal hematoma (white arrows) and the slight narrowing of the spinal canal at the level of the compression fracture (double yellow arrows).
Thoracic spine trauma. Axial and sagittal CT images of an acute lower thoracic spine compression fracture. Note the paraspinal hematoma (white arrows) and the slight narrowing of the spinal canal at the level of the compression fracture (double yellow arrows).
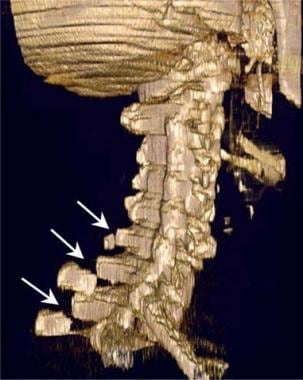
 Thoracic spine trauma. Three-dimensional CT scan of the thoracic spine demonstrates a compression fracture.
Thoracic spine trauma. Three-dimensional CT scan of the thoracic spine demonstrates a compression fracture.
 Thoracic spine trauma. Sagittal CT scan of the thoracic and lumbar spine demonstrates a complete distraction fracture at the L1-2 interspace (arrow).
Thoracic spine trauma. Sagittal CT scan of the thoracic and lumbar spine demonstrates a complete distraction fracture at the L1-2 interspace (arrow).
 Thoracic spine trauma. Axial CT image of an unstable fracture of the thoracic spine. Note the association of compression of the vertebral body with laminar and pedicle fractures. Injury to the anterior, middle, and posterior columns results in an unstable fracture.
Thoracic spine trauma. Axial CT image of an unstable fracture of the thoracic spine. Note the association of compression of the vertebral body with laminar and pedicle fractures. Injury to the anterior, middle, and posterior columns results in an unstable fracture.
 Thoracic spine trauma. Coronal multiplanar reformatted CT images of an unstable thoracic spinal fracture. The association of both anterior compression and lateral subluxation (arrows) indicates instability.
Thoracic spine trauma. Coronal multiplanar reformatted CT images of an unstable thoracic spinal fracture. The association of both anterior compression and lateral subluxation (arrows) indicates instability.
 Thoracic spine trauma. Volume maximum intensity projection CT image of the entire thoracic spine demonstrates spinous process fractures of the C7 through T7 vertebra. Although spinous process fractures of the T1 may occur in a manner similar to a clay shoveler's fracture of the C6 or C7, middle and lower thoracic spinous process fractures most likely occur due to a combination of forward flexion and axial rotation. Note the lack of findings of compression vertebral body fractures.
Thoracic spine trauma. Volume maximum intensity projection CT image of the entire thoracic spine demonstrates spinous process fractures of the C7 through T7 vertebra. Although spinous process fractures of the T1 may occur in a manner similar to a clay shoveler's fracture of the C6 or C7, middle and lower thoracic spinous process fractures most likely occur due to a combination of forward flexion and axial rotation. Note the lack of findings of compression vertebral body fractures.
 Thoracic spine trauma. Three-dimensional surface CT image of the cervical spine. Note the spinous process fractures of the C6, C7, and T1. CT examination of both the cervical and the thoracic spine was obtained as a single study using a multisection CT scanner. All images were obtained by using a 3-mm reconstruction with 1.5-mm collimation. Scanning times were 0.5 seconds per rotation. These 3-dimensional images were reconstructed by using an independent imaging workstation. In complex cases, reconstructed images are very useful in consultation with treating physicians.
Thoracic spine trauma. Three-dimensional surface CT image of the cervical spine. Note the spinous process fractures of the C6, C7, and T1. CT examination of both the cervical and the thoracic spine was obtained as a single study using a multisection CT scanner. All images were obtained by using a 3-mm reconstruction with 1.5-mm collimation. Scanning times were 0.5 seconds per rotation. These 3-dimensional images were reconstructed by using an independent imaging workstation. In complex cases, reconstructed images are very useful in consultation with treating physicians.
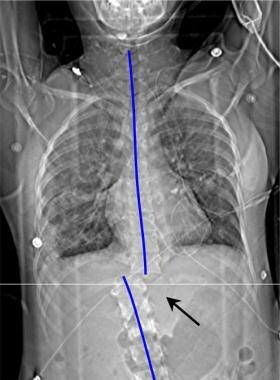 Thoracic spine trauma. Scout view image from a spiral CT scan shows a complete subluxation fracture (curved blue lines) of the lower thoracic spine. Such an injury combines lateral displacement with rotational injury (arrow).
Thoracic spine trauma. Scout view image from a spiral CT scan shows a complete subluxation fracture (curved blue lines) of the lower thoracic spine. Such an injury combines lateral displacement with rotational injury (arrow).
 Thoracic spine trauma. Fracture dislocation of the lower thoracic spine. Axial CT image demonstrates the large distance that the lower thoracic spine has been displaced.
Thoracic spine trauma. Fracture dislocation of the lower thoracic spine. Axial CT image demonstrates the large distance that the lower thoracic spine has been displaced.
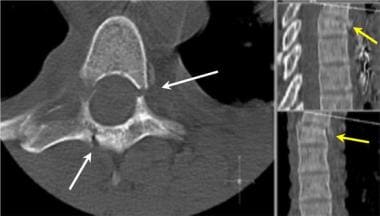
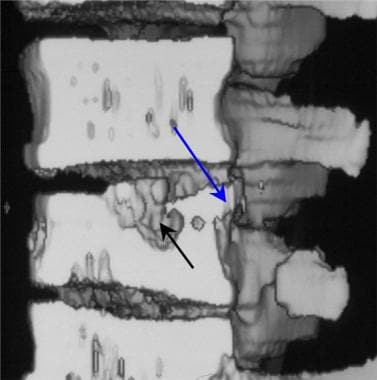
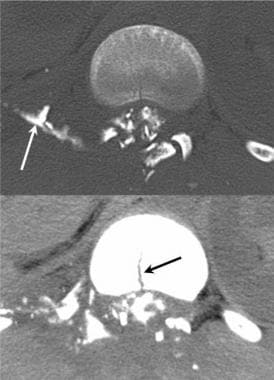 Thoracic spine trauma. Axial CT myelogram in a patient with a gunshot wound to the thoracic spine. While a fracture is obvious, the injury also resulted in a dural tear with a freely leaking cerebrospinal fluid space (white arrow). The midline fracture of the vertebral body is noted in the lower image (black arrow).
Thoracic spine trauma. Axial CT myelogram in a patient with a gunshot wound to the thoracic spine. While a fracture is obvious, the injury also resulted in a dural tear with a freely leaking cerebrospinal fluid space (white arrow). The midline fracture of the vertebral body is noted in the lower image (black arrow).
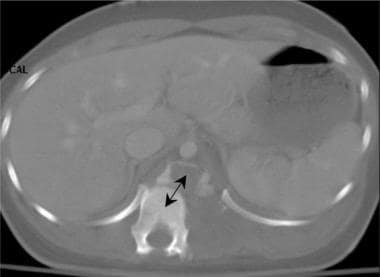
 Thoracic spine trauma. Axial CT image demonstrates a complex fracture of the T12 with rotation subluxation. Air was introduced into the epidural space during the injury.
Thoracic spine trauma. Axial CT image demonstrates a complex fracture of the T12 with rotation subluxation. Air was introduced into the epidural space during the injury.
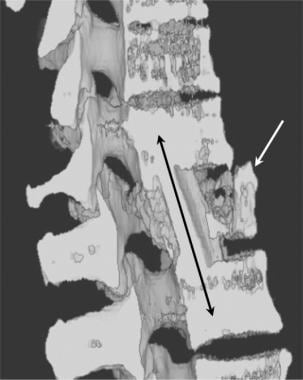
 Thoracic spine trauma. Sagittal multiplanar CT image of a burst fracture following fixation. The image has been cut in the sagittal plane. Surgical repair of unstable thoracic spine fractures, such as this burst fracture, usually involves placement of an interposition graft (double black arrow) together with a lateral plate held in position by screws placed into the vertebral body above and below the injury. A residual fragment of the burst fracture is seen anteriorly (white arrow). The double white arrow illustrates the restored spinal canal.
Thoracic spine trauma. Sagittal multiplanar CT image of a burst fracture following fixation. The image has been cut in the sagittal plane. Surgical repair of unstable thoracic spine fractures, such as this burst fracture, usually involves placement of an interposition graft (double black arrow) together with a lateral plate held in position by screws placed into the vertebral body above and below the injury. A residual fragment of the burst fracture is seen anteriorly (white arrow). The double white arrow illustrates the restored spinal canal.
 Thoracic spine trauma. Shaded-surface 3-dimensional CT image of a burst fracture following fixation. The image has been cut in the sagittal plane. Surgical repair of unstable thoracic spine fractures, such as this burst fracture, usually involves placement of an interposition graft (double black arrow) together with a lateral plate held in position by screws placed into the vertebral body above and below the injury. A residual fragment of the burst fracture is seen anteriorly (white arrow).
Thoracic spine trauma. Shaded-surface 3-dimensional CT image of a burst fracture following fixation. The image has been cut in the sagittal plane. Surgical repair of unstable thoracic spine fractures, such as this burst fracture, usually involves placement of an interposition graft (double black arrow) together with a lateral plate held in position by screws placed into the vertebral body above and below the injury. A residual fragment of the burst fracture is seen anteriorly (white arrow).
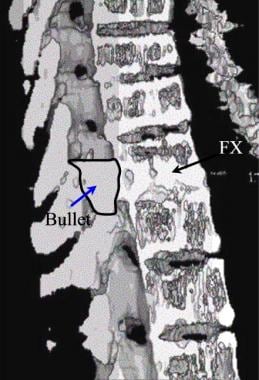 Thoracic spine trauma. Shaded-surface 3-dimensional CT image of a gunshot wound to the thoracic spine. Although the bullet passed into the interspace, causing a fracture of the vertebral body, the bullet stopped within the spinal canal. Note the outline drawn around the bullet (arrow).
Thoracic spine trauma. Shaded-surface 3-dimensional CT image of a gunshot wound to the thoracic spine. Although the bullet passed into the interspace, causing a fracture of the vertebral body, the bullet stopped within the spinal canal. Note the outline drawn around the bullet (arrow).
 Thoracic spine trauma. Shaded-surface 3-dimensional CT scan of a gunshot wound to the thoracic spine. In other cases, the bullet may enter the spinal canal superior to the final position in the canal. The passage of the bullet within the spinal canal (yellow arrow) destroys the spinal cord and also may result in a fracture of the vertebral body. Note that the bullet has been darkened (blue arrow).
Thoracic spine trauma. Shaded-surface 3-dimensional CT scan of a gunshot wound to the thoracic spine. In other cases, the bullet may enter the spinal canal superior to the final position in the canal. The passage of the bullet within the spinal canal (yellow arrow) destroys the spinal cord and also may result in a fracture of the vertebral body. Note that the bullet has been darkened (blue arrow).
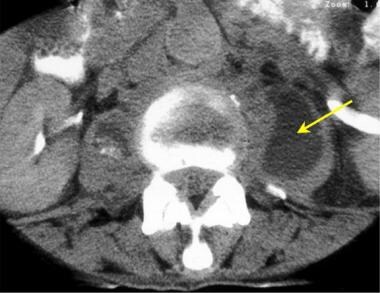 Thoracic spine trauma. Axial CT image in a man with known pulmonary tuberculosis and back pain. Note the left-sided paraspinal abscess (arrow).
Thoracic spine trauma. Axial CT image in a man with known pulmonary tuberculosis and back pain. Note the left-sided paraspinal abscess (arrow).
 Thoracic spine trauma. Sagittal shaded-surface 3-dimensional reconstruction CT scan of the lower thoracic spine. The spinal image has been cut in the midsagittal plane to demonstrate posterior displacement of the thoracic spinal vertebral body (arrow) and downward displacement of the superior endplate. Note the general wedge shape of the vertebral body.
Thoracic spine trauma. Sagittal shaded-surface 3-dimensional reconstruction CT scan of the lower thoracic spine. The spinal image has been cut in the midsagittal plane to demonstrate posterior displacement of the thoracic spinal vertebral body (arrow) and downward displacement of the superior endplate. Note the general wedge shape of the vertebral body.
Because of its superior contrast definition and the absence of superimposed structures, good-quality CT imaging depicts more thoracic spinal injuries than do conventional radiographic studies. However, the percentage of clinically important fractures that are seen on CT scans but not on radiographs is lower with thoracic spinal fractures than with cervical spinal fractures. Most of the fractures missed on radiographs were spinous process fractures, transverse process fractures, and fractures in large patients. Because axial CT is performed with patients in a neutral position, bony distraction of the fracture fragments and subluxations of the spinal articulations may not be as significant on CT images as on they are on acute trauma-series radiographs. [14, 18, 36, 37, 38, 39, 40]
The level of a burst fracture and the percentage of spinal canal stenosis have been correlated with associated neurologic deficits. A significant correlation exists between neurologic deficit and the percentage of spinal canal stenosis. The higher the level of injury, the greater the probability of neurologic deficit. This association may be related to the smaller canal diameter in the upper thoracic spine. The severity of neurologic deficit cannot be predicted.
In patients with Chance-type fractures, CT scans often show a burst-type fracture with posterior cortex buckling or retropulsion, and serial transaxial CT images often show a gradual loss of definition of the pedicles. [15]
Thoracic spine CTs are usually performed during free breathing and with a narrow field of view, but Manca et al suggest that thoracic spine CTs be done during breath hold with additional full field of view (FOV) reconstructions, which can allow evaluation of lungs and identification of extraspinal pathologies during the same examination. [41]
Degree of confidence
The confidence level for the diagnosis of a thoracic spinal fracture with 2-mm axial sections (possible with a multisection CT unit) is reportedly 99%.
Because axial CT is performed with the patient in a neutral position, bony distraction of the fracture fragments and subluxations of the spinal articulations may not be as significant on CT images as on acute trauma-series radiographs.
False-positive results may occur in patients with a Schmorl node, which is a chronic internal herniation of the vertebral disk into the thoracic vertebral body endplate and failure of the fusion of the anterior vertebral endplate epiphysis, resulting in a limbus vertebra. False-negative CT studies may occur in chronic stress injuries and in severe generalized osteoporotic endplate fractures.
It has been reported that among trauma patients who had a chest and/or abdominal CT, fractures of the thoracic spine are frequently underreported. Sagittal reformats of the spine obtained from thin sections and morphometric analysis using electronic calipers help to identify fractures that might otherwise not be identified. [18]
Magnetic Resonance Imaging
Thoracic spinal MRI can demonstrate many vertebral fractures and most abnormalities of alignment. [19] The patterns of injury are similar to those demonstrated on radiographs. MRI is superior to both radiography and CT in the detection of soft tissue injury to the ligaments, facet capsules, and prevertebral spaces. Integrity of the posterior ligamentous complex is one of the 3 aspects of thoracolumbar injury, along with injury morphology and the neurologic status of the patient, that make up the Thoracolumbar Injury Classification and Severity Score (TLICS). [42, 43] TLICS scores have been proposed as a guideline for management of thoracolumbar injuries.
MRI is unique in the ability to depict epidural bleeding and spinal cord injury. Injury to the thoracic cord is particularly critical because such injury may result in paralysis. However, MRI has fewer line pairs of resolution than does CT, which makes MRI a secondary method for fracture evaluation.
(The images below display thoracic spinal injuries on MRI.)
 Thoracic spine trauma. Sagittal MRIs in a patient with acute spinal injury resulting from a motor vehicle accident. A, Fast spin-echo MRI demonstrates a combined fracture compression of vertebral bodies of T8 and T9. A small fragment of bone compromises the spinal canal and is in contact with the spinal cord. B, Gradient-echo T2-weighted image better defines the bone fragment within the canal (arrow). This fracture was associated with a partial spinal cord injury in which loss of motor function occurred with preservation of distal sensory function.
Thoracic spine trauma. Sagittal MRIs in a patient with acute spinal injury resulting from a motor vehicle accident. A, Fast spin-echo MRI demonstrates a combined fracture compression of vertebral bodies of T8 and T9. A small fragment of bone compromises the spinal canal and is in contact with the spinal cord. B, Gradient-echo T2-weighted image better defines the bone fragment within the canal (arrow). This fracture was associated with a partial spinal cord injury in which loss of motor function occurred with preservation of distal sensory function.
 Thoracic spine trauma. Sagittal MRIs of the thoracic spine in a patient who had a complete spinal cord injury. A, Sagittal fast spin-echo T2-weighted MRI demonstrates disruption of the anterior longitudinal ligament (white arrow) and a wide distraction of the T9-T10 facets joints (yellow arrow). The spinal cord between T8-T9 and T9-T10 is disrupted with poorly defined margins. B, Sagittal gradient-echo T2-weighted MRI demonstrates the ligamentous injuries anteriorly (white arrow) and posteriorly (black arrow).
Thoracic spine trauma. Sagittal MRIs of the thoracic spine in a patient who had a complete spinal cord injury. A, Sagittal fast spin-echo T2-weighted MRI demonstrates disruption of the anterior longitudinal ligament (white arrow) and a wide distraction of the T9-T10 facets joints (yellow arrow). The spinal cord between T8-T9 and T9-T10 is disrupted with poorly defined margins. B, Sagittal gradient-echo T2-weighted MRI demonstrates the ligamentous injuries anteriorly (white arrow) and posteriorly (black arrow).
 Thoracic spine trauma. Sagittal T1-weighted MRI image of a compression fracture of the lower thoracic spine. The forces causing a Chance fracture include vertical loading and forward rotation around a fixation point, which often is a seatbelt.
Thoracic spine trauma. Sagittal T1-weighted MRI image of a compression fracture of the lower thoracic spine. The forces causing a Chance fracture include vertical loading and forward rotation around a fixation point, which often is a seatbelt.
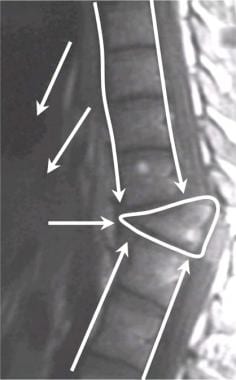
 Thoracic spine trauma. Gradient-echo T2-weighted sagittal MRI image of a compression fracture. The T12 vertebral body has lost vertical height (white arrow). The spinal canal has been narrowed. Note the disruption of the posterior spinal ligaments (black arrow).
Thoracic spine trauma. Gradient-echo T2-weighted sagittal MRI image of a compression fracture. The T12 vertebral body has lost vertical height (white arrow). The spinal canal has been narrowed. Note the disruption of the posterior spinal ligaments (black arrow).
 Thoracic spine trauma. Chance fracture of the T12 resulting in lower thoracic cord injury. Note the edema of the lower thoracic spinal cord (arrow) resulting from the T12 fracture and the associated hyperflexion injury.
Thoracic spine trauma. Chance fracture of the T12 resulting in lower thoracic cord injury. Note the edema of the lower thoracic spinal cord (arrow) resulting from the T12 fracture and the associated hyperflexion injury.
 Thoracic spine trauma. Axial T1-weighted MRI image of the thoracic spine in a patient with a burst injury of the T12 vertebral body. A large bone fragment has entered the spinal canal resulting in posterior displacement of the conus (arrow).
Thoracic spine trauma. Axial T1-weighted MRI image of the thoracic spine in a patient with a burst injury of the T12 vertebral body. A large bone fragment has entered the spinal canal resulting in posterior displacement of the conus (arrow).
 Thoracic spine trauma. Volume maximum intensity projection CT image of the entire thoracic spine demonstrates spinous process fractures of the C7 through T7 vertebra. Although spinous process fractures of the T1 may occur in a manner similar to a clay shoveler's fracture of the C6 or C7, middle and lower thoracic spinous process fractures most likely occur due to a combination of forward flexion and axial rotation. Note the lack of findings of compression vertebral body fractures.
Thoracic spine trauma. Volume maximum intensity projection CT image of the entire thoracic spine demonstrates spinous process fractures of the C7 through T7 vertebra. Although spinous process fractures of the T1 may occur in a manner similar to a clay shoveler's fracture of the C6 or C7, middle and lower thoracic spinous process fractures most likely occur due to a combination of forward flexion and axial rotation. Note the lack of findings of compression vertebral body fractures.
 Thoracic spine trauma. Sagittal T2-weighted MRI of the thoracolumbar junction demonstrates a complete dislocation at the T12-L1 interspace (arrow).
Thoracic spine trauma. Sagittal T2-weighted MRI of the thoracolumbar junction demonstrates a complete dislocation at the T12-L1 interspace (arrow).
With a T2-weighted gradient-echo technique, the cortical break can be demonstrated in some fractures. MRI is superior to CT in the identification of the indirect signs of a fracture, such as paraspinal edema or hemorrhage, epidural bleeding, and sprains of the paraspinal and intraspinal ligaments.
A gradient-echo sagittal T2-weighted MRI of the spine demonstrates compression fractures by showing the cortical bone as dark (black), while the T2-weighted quality shows cerebrospinal fluid and spinal cord edema as bright (white). Subacute hemorrhage within the spinal cord or in the epidural space may be seen as a susceptibility area of lost signal brightness.
Degree of confidence
Thoracic spine MRIs demonstrate many vertebral fractures and most abnormalities of alignment. MRI is superior to CT in the identification of indirect signs of a fracture, such as perivertebral edema or hemorrhage, epidural bleeding, and sprains of the paraspinal and intraspinal ligaments. Associated injuries to intracranial structures are evaluated better by using MRI than CT imaging.
False-positive MRI results are often associated with movement artifacts of metal near the site of injury. Blood-vessel canals may mimic bone injury. The use of upper cervical and intracranial magnetic resonance angiography may help in differentiating certain vascular variations.
False-negative findings may result from motion on the part of the patient. Artifacts related to implanted metal may mask spinal fractures. In older patients or in patients with known neoplastic disease, a pathologic fracture should be considered. In these patients, MRI with Gd-DTPA enhancement will demonstrate a spinal mass or osteomyelitis. MRI has less line-pair resolution than does CT scanning. With T2-weighted gradient-echo sequences, the cortical break can be demonstrated in some fractures; however, even with adequate MRI technique, minimally displaced fracture lines may not be seen by using MRI.
Ultrasonography
The use of thoracic ultrasonography is usually limited to the localization of pleural effusions, which may occur after significant thoracic spinal and chest wall injury. Diagnostic thoracentesis is more easily performed by using sonographic guidance. Paraspinal abscess may be localized prior to aspiration in select patients.
As a result of the limitations of sonographic studies of bone and the lungs, sonography should be used only in specific patients.
Ultrasound does not penetrate the air in the lungs or the bones of the spine and ribs. Ultrasonography may be applied in select patients for localization studies.
Nuclear Imaging
Nuclear medicine studies have a limited role in the acute phase of thoracic spine injury; however, in a possible congenital anomaly, an acute fracture can be differentiated from a limbus vertebra.
After 12-24 hours, a bone scan with technetium-99m hydroxydimethylpyrimidine demonstrates increased uptake in the area of a fracture. Later in the clinical course, persistent back pain may be explained by a nondisplaced facet injury or pedicle fracture, which is also associated with an area of increased uptake. After surgery or in open spinal fractures, diskitis and osteomyelitis can be identified by focal areas of increased activity; however, indium 111–tagged white blood cells (WBCs) act as a more specific agent in the detection of abscess and osteomyelitis. Unfortunately, 111In-tagged WBC scans have a poor sensitivity for the detection of diskitis.
Fat-saturated T1-weighted MRI with intravenous gadolinium enhancement may demonstrate the enhancement of osteomyelitis or diskitis, even in cases in which the 111In WBC scan was negative. MRI is also superior in the detection of an associated epidural abscess.
In cases in which MRI is contraindicated (pacemaker, aneurysm clip, etc) or in the presence severe MRI artifacts resulting from fixation plates, wires, or screws, a combined 99mTc hydroxydimethylpyrimidine-gallium scan is recommended. In all patients, the tomographic qualities of single-photon emission computed tomography (SPECT) improve both accuracy and specificity.
Degree of confidence
In the absence of prior surgery, radionuclear bone imaging is fairly sensitive. If bone scans are needed, SPECT should be applied in all patients with suspected upper thoracic spine trauma.
Many false-positive findings can be expected in older adults. Osteomyelitis, diskitis, metastatic disease, degenerative spondylosis, rheumatoid arthritis, and ankylosing spondylitis [44] may result in abnormal spinal images that are not related directly to acute trauma. In the young child, variations of thoracic spine development may mimic acute injury. SPECT helps improve visualization of these conditions, reducing the occurrence of false-positive findings
False-negative results may occur in the first hours after an acute trauma. If possible, 24 hours should be allowed to pass before attempting nuclear bone scans of the thoracic spine.
Angiography
Angiography has a limited and indirect but critical role in the assessment of thoracic spinal injury. After a gunshot wound to the chest, injuries to the aorta and the proximal great vessels are best evaluated by using angiography. New higher-resolution CT angiography makes catheter angiography less essential. Evaluation of injury to the aorta, subclavian arteries, and innominate artery are routinely performed during the assessment of patients with multisystemic trauma. Trauma, including arterial laceration with hemorrhage, may be seen in association with displaced rib and transverse-process fractures.
The higher resolution of digital subtraction angiography results in excellent image quality. Rarely are other vascular images necessary. Use of angiography is typically reserved for possible interventional repair of arterial injuries and in patients in whom the diagnosis is confused.
Standing waves within the proximal carotid artery or innominate artery may mimic vascular injury with spasm. In the older adult, arteriosclerotic vascular disease may mimic spasm. Intercostal arteries may be in spasm at the time of an examination, preventing localization of a bleeding site.
-
Thoracic spine trauma. Drawing of the thoracolumbar spine viewed from an oblique frontal projection. SC indicates the spinal cord; NP, nucleus pulposus; VB, vertebral body; AF, annulus fibrosis; VNR, ventral nerve root; SN, spinal nerve; TP, transverse process; DNR, dorsal nerve root; and NRG, nerve root ganglion.
-
Thoracic spine trauma. Axial drawing of a typical thoracic vertebral body viewed from above. The thoracic vertebral bodies are unique in that ribs articulate by rib facets (red outline and red arrow) with the correspondingly numbered vertebrae. The superior articular facet (outlined in blue, blue arrow) is oriented along a lateral plane.
-
Thoracic spine trauma. Drawing of a typical thoracic vertebral body viewed in a lateral projection. The superior rib facet, semilunar inferior rib facet and the costal facet provide articulation for the ribs. The articular facet surfaces are oriented laterally. The spinous processes of the upper and mid thoracic vertebrae are angulated caudally.
-
Thoracic spine trauma. Sagittal drawing of the thoracic spine demonstrating the structures that comprise the anterior, middle, and posterior columns. ALL indicates the anterior longitudinal ligament; AF, annulus fibrosus; NP, nucleus pulposus; PLL, posterior longitudinal ligament; SSL, supraspinous ligament; LF, ligamentum flavum; and ISL, interspinous ligament. Lateral drawing of the 3 spinal columns of the thoracolumbar junction. The anterior column is indicated by the black dotted line and includes the anterior spinal ligament, the anterior annulus fibrosis and the intervertebral disk, and the anterior two thirds of the vertebral bodies. The middle column (red dotted line) includes the posterior aspect of the vertebral bodies, the posterior annulus fibrosis, and the posterior longitudinal ligament. The posterior column (blue dotted line) includes all of the spine posterior to the longitudinal ligament (thick blue dotted line).
-
Thoracic spine trauma. Twelve similar thoracic vertebral bodies form the thoracic spine. A rib is attached to each of the vertebral bodies of the same number. The mild kyphosis of the thoracic spine occurs due to the slightly wedged shape of the anterior thoracic vertebral bodies.
-
Thoracic spine trauma. Posterior drawing of the lower thoracic spine. The last rib usually is attached to the 12th thoracic vertebral body. Each thoracic vertebral body articulates with a rib. The facet joints of the thoracic region are oriented in an anterior to posterior direction. The first lumbar vertebral body (blue arrow) is similar to the last thoracic vertebral body (black arrow) except for the absence of a rib at T12.
-
Thoracic spine trauma. Lateral drawing the spine with the natural spinal curves shown by a curved line. A normal lordotic curve of the cervical spine, a mild kyphosis of the thoracic spine, and lordosis of the lumbar region are noted. These curves act to distribute the vertical weight-bearing load most efficiently.
-
Thoracic spine trauma. The natural lordotic curvature of the cervical spine is reversed in the upper thoracic spine to form a kyphosis in the T1-T2-T3 segments in most adults.
-
Thoracic spine trauma. Lateral radiograph of the thoracic spine of a 74-year-old woman. The kyphosis of the thoracic spine is related to osteoporotic failure of the T8 vertebral body. Note the 30-40% wedge-shaped deformity of the T8 vertebra.
-
Thoracic spine trauma. Lateral 3-dimensional maximum intensity projection CT scan of multiple upper thoracic and lower cervical spinous process fractures. The force necessary to fracture the spinous processes of the upper thoracic spine may also involve the lower cervical spine.
-
Thoracic spine trauma. Lower cervical spine facet fracture. Multiple spinal injuries may occur in a single patient due to the similarity of the mechanisms of injury that affect the lower cervical spine and the upper thoracic spine.
-
Thoracic spine trauma. Three-dimensional CT scan of complex midface fractures including a Le Fort I injury in a patient who had fractures of the upper thoracic and lower cervical spinous processes. Sudden deceleration of the face and skull resulted in severe stress forces on the spinous processes.
-
Thoracic spine trauma. Anteroposterior view radiograph of the lumbar spine demonstrates a narrowed T12 vertebral body height (arrow) consistent with a compression fracture.
-
Thoracic spine trauma. Lateral radiograph of the lumbar spine. In the upper portion of the lumbar radiograph, a T12 compression fracture (arrow) is demonstrated. Superimposed lung and rib shadows make full depiction of the fracture difficult.
-
Thoracic spine trauma. Lateral radiograph of the thoracic spine with compression fracture (arrow) centered in the image. The radiograph demonstrates a 40% anterior compression of the vertebral body.
-
Thoracic spine trauma. Lateral radiograph of the lumbar spine in a patient with chronic renal disease. Metabolic bone disease, such as renal osteodystrophy (arrow), results in more frequent and more severe compression fractures.
-
Thoracic spine trauma. Axial CT scan of a T12 compression fracture demonstrates a fracture line through the anterior body of the T12 (white arrow), posterior displacement of the T12 vertebral endplate (black arrow) into the spinal canal, and a fracture of the left transverse spinous process.
-
Thoracic spine trauma. Axial and sagittal CT images of an acute lower thoracic spine compression fracture. Note the paraspinal hematoma (white arrows) and the slight narrowing of the spinal canal at the level of the compression fracture (double yellow arrows).
-
Thoracic spine trauma. Three-dimensional CT scan of the thoracic spine demonstrates a compression fracture.
-
Thoracic spine trauma. Drawing of a Chance fracture of the thoracic lumbar junction. The defect follows an irregular horizontal plane (arrows), which results in disruption of the anterior (black dotted line), the middle column (red dotted line), and the posterior column (blue dotted line).
-
Thoracic spine trauma. Sagittal MRIs in a patient with acute spinal injury resulting from a motor vehicle accident. A, Fast spin-echo MRI demonstrates a combined fracture compression of vertebral bodies of T8 and T9. A small fragment of bone compromises the spinal canal and is in contact with the spinal cord. B, Gradient-echo T2-weighted image better defines the bone fragment within the canal (arrow). This fracture was associated with a partial spinal cord injury in which loss of motor function occurred with preservation of distal sensory function.
-
Thoracic spine trauma. Anterior view of multiple spinal cord contusions caused by burst compression fractures of the middle and lower thoracic spine.
-
Thoracic spine trauma. Sagittal CT scan of the thoracic and lumbar spine demonstrates a complete distraction fracture at the L1-2 interspace (arrow).
-
Thoracic spine trauma. Drawing illustrates the mechanism of injury causing a Chance fracture.
-
Thoracic spine trauma. Axial CT image of an unstable fracture of the thoracic spine. Note the association of compression of the vertebral body with laminar and pedicle fractures. Injury to the anterior, middle, and posterior columns results in an unstable fracture.
-
Thoracic spine trauma. Coronal multiplanar reformatted CT images of an unstable thoracic spinal fracture. The association of both anterior compression and lateral subluxation (arrows) indicates instability.
-
Thoracic spine trauma. Sagittal MRIs of the thoracic spine in a patient who had a complete spinal cord injury. A, Sagittal fast spin-echo T2-weighted MRI demonstrates disruption of the anterior longitudinal ligament (white arrow) and a wide distraction of the T9-T10 facets joints (yellow arrow). The spinal cord between T8-T9 and T9-T10 is disrupted with poorly defined margins. B, Sagittal gradient-echo T2-weighted MRI demonstrates the ligamentous injuries anteriorly (white arrow) and posteriorly (black arrow).
-
Thoracic spine trauma. Sagittal T1-weighted MRI image of a compression fracture of the lower thoracic spine. The forces causing a Chance fracture include vertical loading and forward rotation around a fixation point, which often is a seatbelt.
-
Thoracic spine trauma. Gradient-echo T2-weighted sagittal MRI image of a compression fracture. The T12 vertebral body has lost vertical height (white arrow). The spinal canal has been narrowed. Note the disruption of the posterior spinal ligaments (black arrow).
-
Thoracic spine trauma. Chance fracture of the T12 resulting in lower thoracic cord injury. Note the edema of the lower thoracic spinal cord (arrow) resulting from the T12 fracture and the associated hyperflexion injury.
-
Thoracic spine trauma. Axial T1-weighted MRI image of the thoracic spine in a patient with a burst injury of the T12 vertebral body. A large bone fragment has entered the spinal canal resulting in posterior displacement of the conus (arrow).
-
Thoracic spine trauma. Volume maximum intensity projection CT image of the entire thoracic spine demonstrates spinous process fractures of the C7 through T7 vertebra. Although spinous process fractures of the T1 may occur in a manner similar to a clay shoveler's fracture of the C6 or C7, middle and lower thoracic spinous process fractures most likely occur due to a combination of forward flexion and axial rotation. Note the lack of findings of compression vertebral body fractures.
-
Thoracic spine trauma. Three-dimensional surface CT image of the cervical spine. Note the spinous process fractures of the C6, C7, and T1. CT examination of both the cervical and the thoracic spine was obtained as a single study using a multisection CT scanner. All images were obtained by using a 3-mm reconstruction with 1.5-mm collimation. Scanning times were 0.5 seconds per rotation. These 3-dimensional images were reconstructed by using an independent imaging workstation. In complex cases, reconstructed images are very useful in consultation with treating physicians.
-
Thoracic spine trauma. Scout view image from a spiral CT scan shows a complete subluxation fracture (curved blue lines) of the lower thoracic spine. Such an injury combines lateral displacement with rotational injury (arrow).
-
Thoracic spine trauma. Fracture dislocation of the lower thoracic spine. Axial CT image demonstrates the large distance that the lower thoracic spine has been displaced.
-
Thoracic spine trauma. Sagittal T2-weighted MRI of the thoracolumbar junction demonstrates a complete dislocation at the T12-L1 interspace (arrow).
-
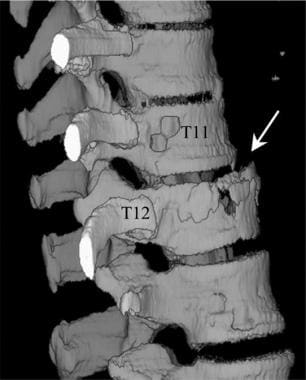
Thoracic spine trauma. Three-dimensional volume image of the thoracic and lumbar spine demonstrates a fracture dislocation of the T11-T12 vertebrae.
-
Thoracic spine trauma. Epidural air (black arrow) is noted, as is gas in the muscular layers of the neck (white arrows).
-
Thoracic spine trauma. Axial CT myelogram in a patient with a gunshot wound to the thoracic spine. While a fracture is obvious, the injury also resulted in a dural tear with a freely leaking cerebrospinal fluid space (white arrow). The midline fracture of the vertebral body is noted in the lower image (black arrow).
-
Thoracic spine trauma. Axial CT image demonstrates a complex fracture of the T12 with rotation subluxation. Air was introduced into the epidural space during the injury.
-
Thoracic spine trauma. Sagittal multiplanar CT image of a burst fracture following fixation. The image has been cut in the sagittal plane. Surgical repair of unstable thoracic spine fractures, such as this burst fracture, usually involves placement of an interposition graft (double black arrow) together with a lateral plate held in position by screws placed into the vertebral body above and below the injury. A residual fragment of the burst fracture is seen anteriorly (white arrow). The double white arrow illustrates the restored spinal canal.
-
Thoracic spine trauma. Shaded-surface 3-dimensional CT image of a burst fracture following fixation. The image has been cut in the sagittal plane. Surgical repair of unstable thoracic spine fractures, such as this burst fracture, usually involves placement of an interposition graft (double black arrow) together with a lateral plate held in position by screws placed into the vertebral body above and below the injury. A residual fragment of the burst fracture is seen anteriorly (white arrow).
-
Thoracic spine trauma. Shaded-surface 3-dimensional CT image of a gunshot wound to the thoracic spine. Although the bullet passed into the interspace, causing a fracture of the vertebral body, the bullet stopped within the spinal canal. Note the outline drawn around the bullet (arrow).
-
Thoracic spine trauma. Shaded-surface 3-dimensional CT scan of a gunshot wound to the thoracic spine. In other cases, the bullet may enter the spinal canal superior to the final position in the canal. The passage of the bullet within the spinal canal (yellow arrow) destroys the spinal cord and also may result in a fracture of the vertebral body. Note that the bullet has been darkened (blue arrow).
-
Thoracic spine trauma. Axial CT image in a man with known pulmonary tuberculosis and back pain. Note the left-sided paraspinal abscess (arrow).
-
Thoracic spine trauma. Sagittal shaded-surface 3-dimensional reconstruction CT scan of the lower thoracic spine. The spinal image has been cut in the midsagittal plane to demonstrate posterior displacement of the thoracic spinal vertebral body (arrow) and downward displacement of the superior endplate. Note the general wedge shape of the vertebral body.
-
Thoracic spine trauma. Coronal shaded-surface display of a compression fracture. Note the downward displacement of the vertebral body endplate (double blue arrow) and the small central cold abscess (black arrow).
-
Thoracic spine trauma. Microscopic image of a smear from a paravertebral abscess aspirate. Note the red stain associated with tuberculosis. Tuberculosis is one of the more common causes of spinal compression fracture in the underdeveloped nations of Asia and the Far East (acid-fast stain, magnification X100).
-
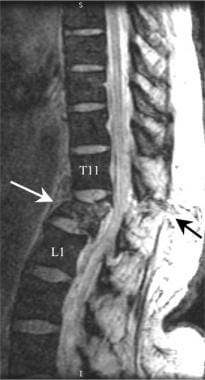
Sagittal MRP CT of the Thoracic Spine. This fracture dislocation of T11 on T12 demonstrates a jumped locked facet of T11 on T12.
-
Sagittal PD MRI of the lumbar spine. The examination demonstrates the subluxation of the T11 on T12. Note the compression of the lower thoracic spinal cord. (arrow)





