Practice Essentials
Acute obstructive uropathy is a commonly encountered condition occurring in inpatient and outpatient settings. Unilateral obstruction to urinary outflow typically occurs, with little if any change in measured renal function in a healthy individual. However, the less common bilateral form results in measurable changes in kidney function. [1, 2, 3, 4, 5, 6, 7]
The backup of urine into the unilateral or bilateral kidneys causes hydronephrosis. Symptoms include difficulty initiating micturition, acute urinary retention, and lower abdominal discomfort and distention. The most common cause is benign prostatic hypertrophy (BPH) or hyperplasia. Other causes include constipation, urethral strictures, phimosis or paraphimosis, prostatic adenocarcinoma, retroperitoneal adenopathy, colonic endometriosis, ureterocele, urolithiasis, neuropathic bladder dysfunction, and urate nephrolithiasis. Urinary retention occurs in up to 1-2% of men with BPH each year. [1]
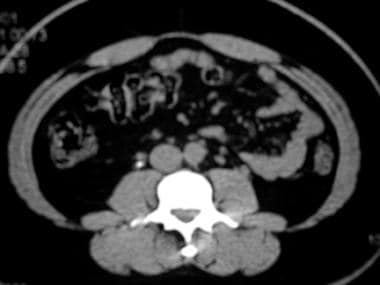
(Acute obstructive uropathy is depicted in the scans below.)
 Right-sided hydronephrosis secondary to mid ureteral calculus in young female presenting with acute flank pain
Right-sided hydronephrosis secondary to mid ureteral calculus in young female presenting with acute flank pain
Preferred examination
The advent of helical computed tomography (CT) scanning has dramatically altered the diagnostic imaging approach to patients presenting with acute flank pain. Unenhanced helical CT has both a high sensitivity of 95-98% and a high specificity of 96-100% in detecting ureteral calculi in the acute setting. [4, 8, 9, 10] Calcified and noncalcified calculi may be identified, along with the location and size of the stone. Secondary signs of obstructive uropathy, including hydronephrosis, perinephric and periureteral stranding, and ureterectasis, are well demonstrated on CT. [10, 11]
Several reports compared unenhanced helical CT with intravenous urography (IVU), the established criterion standard in evaluating the genitourinary system. [12, 13] CT has been shown to be more sensitive in detecting and characterizing ureteral calculi and at least as sensitive in demonstrating the presence of obstructive uropathy. [14]
Additionally, CT may be performed rapidly, in approximately one third the time of an IVU study, and does not require the use of IV contrast material. The ability to diagnose noncalculus etiologies, as well as evaluate other intra-abdominal pathologies that may mimic renal colic, affords CT an invaluable advantage.
Levine et al reported the sensitivity of plain radiography in detecting ureteral calculi to be approximately 45% and recommended that noncontrast helical CT replace the kidneys, ureters, bladder (KUB) film as the initial and possibly only imaging study. [15] While CT appears to have replaced plain radiography and IVU in the initial evaluation of acute flank pain, these modalities remain involved in the follow-up evaluation of stone disease, as well as surgical and interventional planning.
Initial ultrasonography is especially useful in determining the cause of the sudden onset of abdominal or flank pain, since patients with symptomatic abdominal aneurysms can be difficult to distinguish from those with renal colic. While US demonstrates renal calculi, it is poor at detecting ureteral stones. Doppler ultrasonography has been suggested as a method of indirectly determining obstruction by measuring the resistive index in renal arteries and evaluating the direction and magnitude of ureteral jets. [16, 17, 18] The American College of Radiology (ACR) noted that ultrasonography is generally not adequate for planning and intervention, as CT more accurately characterizes stone size and location. [19]
In nuclear medicine, the passage of radionuclide agents through the urinary tract is monitored with a gamma camera. Outlines of the kidney and ureter are generated, and a point of obstruction may be evident. More importantly, it provides physiologic information regarding the function and dynamics of the urinary system. The technique of choice in the evaluation of obstruction is diuresis renography, which is performed with technetium-99m-labeled mercaptoacetyltriglycine (99mTc-MAG3) in most centers. [20, 21, 22]
Diuresis renography is not performed routinely in acute ureteral colic, as CT usually provides the necessary information. However, it may be important in documenting return of renal function in patients for whom urologic intervention is required. Renography with Lasix is useful in determining whether pelvocalyceal system dilatation, often observed on a screening study such as US, is obstructive or nonobstructive in nature.
Ultrafast T1- and T2-weighted techniques such as spoiled gradient echo (T1) and single-shot fast spin echo (T2) have been reported to be highly sensitive and specific for determining the presence of both ureteral calculi and acute obstructive uropathy. However, as with US, in magnetic resonance urography (MRU), the degree of dilatation must be sufficient to use the native urine as a contrast agent. [23, 24]
Limitations of techniques
An inherent limitation of unenhanced helical CT is in providing functional information. The severity of obstruction may be inferred by the presence of perinephric stranding, which is believed to result from forniceal rupture or inflammation in the perirenal fat from high calyceal pressures. The absence of this finding, as well as the other signs of obstruction, does not exclude a significant obstruction.
Performing a contrast-enhanced CT may provide greater physiologic information by demonstrating an obstructive nephrogram and pyelosinus extravasation of contrast material. An important consideration in choosing this modality is the significant radiation dose to the patient, compared to an intravenous pyelogram (IVP). This disadvantage restricts its use, especially in pregnant and pediatric patients.
It has been reported that in patients with ureteral calculi, stone size alone determines initial treatment of patients, with no correlation found between severity of obstruction as suggested by CT and the decision to treat conservatively or perform an intervention. The authors therefore suggest that nonenhanced helical CT is adequate for the initial diagnosis and treatment of patients with stone disease.
Plain radiography and IVU have similar drawbacks, including lower sensitivity because of superimposition of bone and other calcified structures and obscuring bowel pattern. They are limited by stone size (< 4 mm) and patient habitus. IVU, although providing both anatomic and physiologic information, has the added disadvantage of being time consuming and dependent on administration of contrast material, with its potential complications. It is also dependent on renal function, as the use of the test is greatly diminished when the serum creatinine concentration is elevated when the patient has both intrinsic renal disease and an acute obstruction.
US evaluates the ureters and detects calculi poorly. The accuracy of US in diagnosing obstruction in the setting of acute flank pain was found to be approximately 66%. This is directly related to the anatomic nature of the examination, which relies mainly on the presence of hydronephrosis to make the diagnosis. In early obstruction, up to 36 hours after onset, no dilatation of the collecting system may be present, and a false-negative study may result.
Doppler sonography is operator dependent and time consuming. Determination of ureteral jets and the resistive index has not been adopted into widespread clinical use for acute obstruction because of technical limitations and questionable accuracy. Most pathologic processes decrease renal perfusion and thus increase the resistive index (RI).
Diuresis renography, a physiologically driven study, depends on renal function. If marked impairment of bilateral renal function is present, an indeterminate study results. In patients who are dehydrated, the expected response to the diuretic may not be evident, leading to an inconclusive study.
The use of MRU in the acute setting of flank pain also is limited. Studies comparing MRU to CT and IVU have revealed that MRU misses small calculi and mild dilatation. In addition, it is time consuming and expensive and is limited to special situations, such as pregnant patients.
Imaging guidelines
The American College of Emergency Physicians (ACEP), European Association of Urology (EAU) and the American College of Radiology (ACR) recommend ultrasound as the initial imaging modality for emergent presentations of acute flank pain where stone disease is suspected. [7, 19, 25, 26]
The EAU published the following recommendations [7] :
-
Immediate imaging is indicated with fever or solitary kidney and when diagnosis is doubtful.
-
Use non-contrast-enhanced computed tomography to confirm stone diagnosis in patients with acute flank pain following initial ultrasound assessment.
-
Perform a contrast study if stone removal is planned and the anatomy of the renal collecting system needs to be assessed.
-
Non-contrast-enhanced CT is used to confirm stone diagnosis in patients with acute flank pain, as it is superior to IVU.
-
Enhanced CT enables 3D reconstruction of the collecting system, as well as measurement of stone density and skin-to-stone distance.
The ACR has noted the following [26] :
-
In patients with urinary diversion after a remote history of cystectomy for cancer and no fever, normal WBC count, and urine output, CT scan shows new moderate bilateral hydronephrosis.
-
In patients with a 7-day history of right flank pain, fever, and leukocytosis, CT scan shows a 10-mm calculus in the mid right ureter without hydronephrosis.
-
In pregnant patients (20+ weeks) with a 3-day history of left flank pain, fever, and leukocytosis, ultrasound shows new moderate left hydronephrosis.
-
In patients with advanced cervical carcinoma and decreased estimated glomerular filtration rate < 15, CT scan reveals new bilateral hydronephrosis and hydroureter due to local invasion by a pelvic mass.
-
In patients with a prolonged history of right flank pain, fever, and leukocytosis, CT scan shows dilated right ureter and renal pelvis with perinephric stranding.
-
In patients with urinary ascites after recent abdominal surgery, CT urogram reveals contrast leak from left pelvic ureteral injury.
The American Urological Association recommends the following [6, 27] :
-
In the presentation of acute flank pain, noncontrast computed tomography (NCCT) is the most sensitive and specific mode of imaging to confirm the diagnosis of upper urinary tract stones. However, ultrasonography is recommended to be used initially, if available, because it is inexpensive and free of radiation. If the urinary tract anatomy needs assessment before stone removal, contrast imaging should be performed.
-
NCCT is recommended before performing percutaneous nephrolithotripsy (PCNL), and it could identify the candidate’s suitability for shockwave lithotripsy (SWL) versus ureteroscopy. If significant renal function impairment is suspected, functional imaging (eg, diethylenetriamine-pentaacetate or mercaptoacetyltriglycine) could be used to assess the renal function.
-
In pregnancy, ultrasonography is the recommended first-line imaging modality, with MRI being second line and low-dose NCCT being the last resort.
-
Ultrasonography is the preferred choice of imaging in children to limit exposure to ionizing radiation. However, because of low sensitivity, a kidney-ureter-bladder (KUB) radiograph or low-dose NCCT may be necessary. NCCT imaging is recommended in children before PCNL.
Special concerns
Calculi may be missed and signs of obstruction may not be evident. Clinical and imaging follow-up care is warranted to prevent the loss of kidney function. The interpreting radiologist is responsible for all pathologic entities present on the imaging study, whether or not they may be the source of the present symptoms.
The diagnostic imaging approach to these patients begins with an abdominal US to demonstrate the presence of hydronephrosis. Remember that mild hydroureteronephrosis is observed in normal pregnant patients. Transvaginal and transrectal US may be used to detect distal ureteral calculi. Doppler sonography plays an important role, using the RI and ureteral jets to diagnose obstruction.
Where US does not provide a diagnosis, MRU or IVU may be the next step in imaging. MRU, if available, is preferred, as there is no ionizing radiation exposure. One can make the diagnosis of an obstructing calculus by the presence of a filling defect with associated perinephric or periureteral edema.
Alternatively, an extremely limited IVU may provide the necessary information. The limited IVU consists of a preliminary film followed by a single postcontrast exposure to demonstrate the point and cause of obstruction. However, the gravid uterus with the fetus can obscure a nonpregnancy cause of hydronephrosis.
ICD-10
The ICD-10 code for uropathy is N39.9, for obstructive uropathy N13.9, and for reflux uropathy N13.9. The ICD-10 code for renal colic is N23. [28]
Radiography
The plain abdominal radiograph or KUB film has long been the initial imaging study of choice in patients presenting with symptoms of acute flank pain. [4] Calculi may have a variable appearance on radiographs depending on their chemical composition, especially the percentage and distribution of calcium within them. They may appear homogeneously dense and smooth to laminated and jagged.
(The radiographic characteristics of acute obstructive uropathy are demonstrated in the images below.)
 Kidneys, ureters, bladder (KUB) film showing right staghorn calculus and small left proximal ureteral calculus
Kidneys, ureters, bladder (KUB) film showing right staghorn calculus and small left proximal ureteral calculus
 Delayed intravenous pyelogram (IVP) film with right staghorn calculus and obstructive nephrogram on the left, from a stone lodged in the proximal ureter
Delayed intravenous pyelogram (IVP) film with right staghorn calculus and obstructive nephrogram on the left, from a stone lodged in the proximal ureter
While 90% of stones contain calcium, the sensitivity of plain films has been reported at only 50-60%, with a specificity of 70%. Therefore, in many centers, plain radiographs are deferred in favor of CT in the acute setting. In some instances, renal and ureteral calculi are detected on plain abdominal radiographs obtained for another reason.
Most noncalcified stones, blood clots, and most other intraluminal obstructive causes are radiolucent; therefore, they are not seen on abdominal radiographs. In trauma, the presence of pelvic fractures and soft-tissue mass in the abdomen or pelvis may alert the radiologist to the possibility of ureteral injury, a rare complication, or obstruction from a large hematoma.
IVU, also termed excretory urography, came into clinical existence in the 1920s as a method of evaluating the structure and function of the kidney and urinary tract. It served as a screening study and a diagnostic imaging study in patients with acute renal colic or ureteral colic, demonstrating calculi and the presence of obstruction fairly accurately.
Since 1995, noncontrast helical CT has superseded IVU in this setting, at least as a screening study. Obstructive uropathy demonstrated on unenhanced helical CT often requires no further imaging studies. An estimated 15% of helical CT studies require radiopaque contrast media to confirm or exclude pelvic calcifications as stones or phleboliths. [29] However, IVU may be performed if findings are equivocal or a noncalculus etiology is suggested.
IVU begins with a scout or preliminary radiograph. Additionally, oblique scout radiographs may be obtained. Preinjection linear tomograms are helpful when the bowel pattern obscures the areas of interest. Following the administration of the contrast agent, coned films and tomograms are then obtained, with the intervals and total number of films being quite variable. In a normal kidney, opacification of the renal parenchyma is observed within 1 minute. Within the next 2 minutes, the pelvocalyceal system may be seen, followed by the ureters approximately 5-10 minutes post injection.
In an obstructed kidney, delayed accumulation of contrast is seen, resulting in a nephrogram that is initially of lower density. Progressive concentration of contrast within the renal cortex and medulla occurs, producing the classically described "obstructive nephrogram" that may persist for some duration. Striations may occasionally be seen in the parenchyma, representing contrast material within dilated tubules.
The pelvocalyceal system may not opacify for hours or at all, depending on the severity of obstruction. Dilatation proximal to the obstructing process may be seen as hydronephrosis and hydroureter, which may be minimal in the acute situation. A standing column of contrast may be observed proximal to the obstruction. Pyelosinus extravasation of contrast and mild clubbing of the calyces also may be seen.
Degree of confidence
Degree of confidence in interpreting plain film in acute obstructive uropathy depends on the etiology. Determining the presence of calculi depends on multiple factors, including the size of the stone, chemical composition, location, and multiplicity. Equally important are the technical factors involved in obtaining an optimal radiograph. Further imaging is required when calculi are observed, to confirm their presence and determine if signs of obstruction exist.
On an IVU, the findings of a persistent nephrogram and delayed passage of contrast through the urinary system indicate with a high degree of confidence that an obstruction is present. IVU is best performed following a screening study that produces either negative or equivocal results.
False positives/negatives
Both false positives and false negatives are quite common, as the sensitivity and specificity of plain radiographs are poor. Small calcified stones, radiolucent stones, clots, and mucosal edema are not visualized. In addition, a large patient body habitus and overlying bowel may obscure even densely calcified stones, resulting in a false-negative interpretation.
Most false positives occur because of the presence of other calcific densities within the perceived or expected areas of the kidney and ureter. While gallstones usually are multiple and have a faceted appearance, they may be seen overlying the right kidney and, even on oblique films, may be indistinguishable from renal calculi. In the pelvis, phleboliths often are misinterpreted as ureteral calculi. The radiolucent center of a phlebolith may not always be present to help differentiate the two.
As reported in the literature, IVU sensitivity in the evaluation of acute flank pain varies from 52 to 87%. The detection of calculi as a cause of obstructive uropathy depends on multiple factors, including stone size and location, as well as the degree of obstruction. As a result, false-negative studies are not uncommon in the urographic evaluation of calculi.
The presence of a standing column of contrast does not always indicate the site of obstruction, as it may be seen in normal individuals.
Computed Tomography
On unenhanced helical CT, calcified calculi appear as opaque densities within the genitourinary tract, as in radiographs. Interestingly, calculi that are radiolucent on plain film also are of high attenuation on CT. Researchers have reported that Hounsfield values may be used to differentiate the types of calculi, as this can provide the clinician information concerning an underlying metabolic disorder, as well as influence treatment decisions. However, the overlap in Hounsfield values among the different stones makes this of limited use. [30, 31, 32, 2, 10]
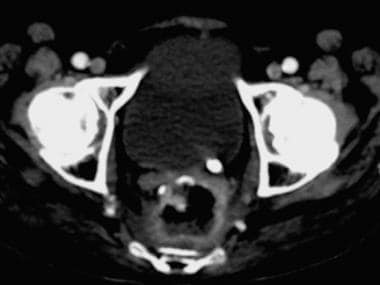
(Enhanced CT scans of acute obstructive uropathy are demonstrated below.)
These values become important in determining the presence of an intraluminal blood clot, which appears dense on CT but has a lower attenuation value than calculi. An exception to the normal high attenuation of calculi has been described in a small percentage of HIV-positive patients being treated with indinavir, a protease inhibitor. [33] As the stones are of soft-tissue attenuation, they are not detected on non–contrast-enhanced CT.
As mentioned previously, unenhanced helical CT is not a physiologic imaging study, and the sole finding of a stone is inadequate to make the diagnosis of obstruction. Therefore, secondary signs of obstruction, as detected on CT, are necessary to confirm the diagnosis and obtain an idea concerning the severity of obstruction. In the presence of ureteral calculi, proximal ureterectasis is the most commonly seen indirect sign. This also may be observed with other causes of intraluminal obstruction.
Dilatation of the pelvocalyceal system is seen on CT as anterior and medial bulging of the renal pelvis, which is of low attenuation compared to the surrounding renal parenchyma. Renal enlargement also may be observed in some patients. Perinephric fat stranding, representing engorged lymphatics and/or edema, is seen as linear wispy densities in the normally low-attenuation fat. Moderate-to-severe perinephric stranding generally corresponds to the degree of obstruction present.
Periureteral stranding densities often are seen, again representing edema in the surrounding fat. Other signs of obstruction include the rim sign, which refers to the soft-tissue attenuation halo around an intraureteral calculus, ureteral wall edema, and blurring of the renal sinus fat. One or more of these secondary signs usually is present, and the predictive values of the individual signs have been reported in the literature. Ureterectasis, hydronephrosis, and periureteral and perinephric stranding each have a positive predictive value of approximately 90%.
Hydronephrosis and perinephric stranding may be the only signs of obstruction in patients with inadvertent ligation of the ureters, while the presence of an intra-abdominal hematoma in a posttraumatic setting or an inflammatory mass in a patient with abdominal pain indicates a possible etiology.
The administration of IV contrast material in the above situations may help to delineate the ureter and determine whether the obstruction is indeed secondary to extrinsic compression. In many patients, IVU or direct visualization of the urinary tract is needed to establish the diagnosis.
Contrast-enhanced CT in obstruction produces findings similar to that first described with IVU, revealing a prolonged parenchymal phase. The persistent nephrogram, in which the kidney appears with either a homogeneous or mottled density, results from delayed passage of contrast into the collecting system. Pyelosinus extravasation is well demonstrated on CT as areas of contrast material within the renal sinus fat.
Dual-energy CT (DECT) can provide information on stone composition. Two data sets are obtained with different peak kilovoltages from the same region, and material decomposition is determined by attenuation differences at different energy levels. Calculi are detectable using iodine subtraction techniques. [34, 35]
Degree of confidence
Degree of confidence in interpreting an unenhanced helical CT in a patient with a ureteral stone depends on the presence of secondary signs of obstruction. Ureterectasis and perinephric stranding, when present together, have a positive predictive value of 99%. With other causes, secondary signs of obstruction increase the confidence in making the diagnosis, although a clear-cut cause may not be evident.
The largest source of false-positive errors in unenhanced helical CT results from phleboliths in the pelvis. On CT, the radiolucent center is not present to help differentiate them from stones, and some stones have a lucent center. The false-positive rate in most studies is approximately 4%. Administration of IV contrast may help by outlining the ureter and separating it from extraluminal densities.
The absence of secondary signs of obstruction, as may occur in early obstruction, can result in a false-negative study, especially when no intraluminal or extraluminal cause may be seen. The incidence of false negatives is reported to be 0-6%.
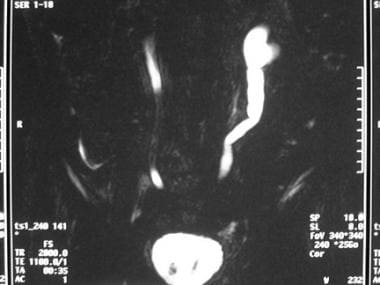
Magnetic Resonance Imaging
As previous mentioned, ultrafast T1- and T2-weighted techniques such as spoiled gradient echo (T1) and single-shot fast spin echo (T2) have been reported to be highly sensitive and specific for determining the presence of ureteral calculi and acute obstructive uropathy. However, as with US, in magnetic resonance urography (MRU), the degree of dilatation must be sufficient to use the native urine as a contrast agent [23, 24, 36, 2, 37]
(See the images below.)
Distinguishing between pain in pregnancy caused by urolithiasis and physiologic dilation of the renal tract can be challenging. Although ultrasound may be the first-line imaging test in the pregnant patient, MRI is better able to distinguish the cause of renal dilation. In cases of physiologic dilation, smooth tapering of the ureter in the middle third will be seen because it is compressed between the gravid uterus and the retroperitoneum. In cases of obstruction caused by calculi, renal enlargement and perinephric edema will be visualized. If there is a calculus in the lower ureter, a standing column of dilated ureter will be seen below the physiologic constriction, and the stone may be seen. [38]
The use of MRU in the acute setting of flank also is limited. Studies comparing MRU to CT and IVU reveal that MRU misses small calculi and mild dilatation. In addition, it is time consuming and expensive and is limited to special situations, such as pregnant patients.
For nephrourographic techniques and applications, see Kalb et al [39] and Akgun et al. [40]
Ultrasonography
The hallmark of obstruction on US is the presence of hydronephrosis. Prominent anechoic structures within the renal sinus represent a dilated pelvocalyceal system. Renal calculi also may be demonstrated as echogenic foci with or without shadowing. This finding depends on the size of the calculi, with smaller stones blending into the echogenic renal sinus. Ureteral calculi and ureterectasis are detected less often. While UPJ and UVJ stones may be observed, mid ureteral stones are extremely difficult to detect. [41]
(The ultrasonographic characteristics of acute obstructive uropathy are demonstrated below.)
 Ureterovesical junction calculus seen on abdominal ultrasound using the bladder as an acoustic window
Ureterovesical junction calculus seen on abdominal ultrasound using the bladder as an acoustic window
The reported sensitivity of US in the detection of a ureteral stone and associated obstruction is 60-70%. As a result, US is not routinely used in the evaluation of acute renal or ureteral colic. However, it is an important screening examination in pregnant patients with acute flank pain and in acute renal failure. [42, 3, 38] The gravid uterus causes ureteric obstruction, and a ureteric stone may be missed
Doppler sonography is an additional tool that may be employed when radiation exposure is undesirable, such as in pregnant patients. The RI, which is a measure of impedance to renal blood flow, may be raised when obstruction to urine outflow exists. In most centers, obstruction is indicated by an RI greater than 0.70 or a difference of greater than 0.10 between the kidneys. However, any process causing decreased perfusion will result in an elevated RI. Ureteral jets also may be evaluated; these may be absent or decreased in frequency in acute obstruction.
Degree of confidence
US has inherent limitations that restrict its use in patients with symptoms of acute renal or ureteral colic. Even in those patients in whom it is used, further imaging often is required for confirmation and characterization of the obstruction.
The presence of obstruction is inferred by visualizing a dilated collecting system. This may be minimal or even absent in acute obstruction. In addition, ureteral calculi are not well demonstrated. The false-negative rate is as high as 35% in patients with uropathy secondary to a calculus lodged in the ureter. Technical limitations to the study, such as patient obesity, bowel gas, and operator skill, also may result in a false-negative study.
The false-positive rate is approximately 10% in patients with urolithiasis. The source of such errors includes vascular calcifications that may simulate a calculus. Peripelvic cysts, an extrarenal pelvis, or even a normal collecting system may be misinterpreted as representing hydronephrosis. Doppler sonography can help by readily distinguishing renal hilar vessels from a slightly dilated collecting system.
Nuclear Imaging
Scintiscans and time-activity curves before and after administration of a diuretic (furosemide) are obtained over a period of approximately 35 minutes. In a normal renogram, initial increased activity is seen as tracer accumulates within the kidney. As tracer moves into the collecting system and ureter, the activity in the kidney starts to drop. In kidneys with dilated collecting systems, an up-slope in the time-activity curve occurs as tracer is retained within the kidney. [22]
Administration of furosemide in a nondilated kidney results in a washout of tracer activity from the collecting system, reflected as a down-slope on the time-activity curve. T½ is defined as the time taken for reduction of activity by 50%; a normal T½ is less than 10 minutes with 99mTc-MAG3.
In a kidney with collecting system dilatation, a decrease in activity with furosemide indicates a nonobstructive cause of dilatation. In an obstructed kidney, no response is observed following the injection of furosemide. A prolonged T½ greater than 20 minutes is highly indicative of obstruction. In addition, the scintiscans, while providing the data for the time-activity curve, also may indicate the site of obstruction, past which little or no activity is seen.
Degree of confidence
Diuresis renography is accepted as a useful examination in distinguishing obstructive from nonobstructive urinary tract dilatation, especially when collecting system dilatation has been detected on another imaging study. In general, it correlates with findings at surgery and ureteral perfusion studies.
To make this study definitive, renal function must be at least partially preserved. The glomerular filtration rate (GFR) must be greater than 15 mL/min for an obstructive time-activity curve to be judged accurate. In patients where the GFR is less than 15 mL/min, no response to the administration of furosemide is observed. No washout of activity occurs regardless of the presence or absence of obstruction. Thus, the study is deemed indeterminate, and further workup or intervention is required to make the diagnosis.
False positives/negatives
False-positive results are encountered predominantly as a result of impaired renal function and overly compliant collecting systems. Both result in a delayed washout phase, leading to the erroneous diagnosis of obstruction. In addition, use of an inadequate dose of diuretic may lead to a similar conclusion.
The incidence of false-negative findings is lower and may result from a noncompliant collecting system. In a partially obstructed urinary tract, the high-flow state following diuretic administration may overcome the obstruction, resulting in a normal-appearing time-activity curve.
-
Right ureteral calculus with periureteral stranding
-
Right-sided hydronephrosis secondary to mid ureteral calculus in young female presenting with acute flank pain
-
Contrast-enhanced CT showing calculus at left ureterovesical junction
-
Left ureterectasis secondary to a distal ureteral stone
-
Moderate left-sided and mild right-sided hydronephrosis
-
Kidneys, ureters, bladder (KUB) film showing right staghorn calculus and small left proximal ureteral calculus
-
Delayed intravenous pyelogram (IVP) film with right staghorn calculus and obstructive nephrogram on the left, from a stone lodged in the proximal ureter
-
Pelvocalyceal system dilation from ureteropelvic obstruction
-
Ureterovesical junction calculus seen on abdominal ultrasound using the bladder as an acoustic window
-
Dilated collecting system on left seen on MRI
-
Left-sided hydroureter and hydronephrosis secondary to distal ureteral obstruction
-
Filling defects within the collecting system due to calculi visualized during percutaneous nephrostomy. Dilatation of the upper pole and mid renal calyces are observed.