Practice Essentials
Chemoembolization is the technique of delivering chemotherapeutic agents via a catheter into the feeding arteries of a tumor along with a blood vessel occluding agent to starve the blood supply to the tumor. Arterial chemoembolization is also termed transarterial chemoembolization (TACE). [1, 2, 3, 4, 5] Hepatocellular carcinoma (HCC) is the most common primary liver tumor worldwide, and its incidence is rising, with most HCCs being associated with cirrhosis. The risk of developing HCC appears to be related to the degree of activity of cirrhosis. The risk is high in patients with macronodular cirrhosis secondary to hemochromatosis and lower in those with alcoholic micronodular cirrhosis. International guidelines suggest the use of regular ultrasound examination for early diagnosis of HCC in patients with liver cirrhosis, but 40% of nodules greater than 2 cm may escape detection. Cross-sectional imaging with contrast-enhanced CT or MRI should be done for diagnostic and treatment planning purposes. Such imaging can determine whether there is anatomy or pathology that may prevent TACE from being safe or effective, such as whether the main portal vein is thrombosed. [2, 3, 6, 7, 8, 9]
Hepatocellular carcinoma accounts for 70–90% of primary liver cancers, and the incidence of HCC in the United States has tripled over the past 4 decades, which has been attributed to a number of factors, such as undiagnosed chronic hepatitis C virus, alcohol consumption, and increased levels of obesity and metabolic syndrome. HCC remains very difficult to manage, with average 5-year survival less than 15%. [2, 10]
Surgery offers the best prospect of cure, but the resectability of HCC is low. Key predictors of tumor response after chemoembolization on unresectable HCC include tumor size, vascularity, and number, as well as portal vein invasion. Factors associated with poor prognosis for overall patient survival include Child-Pugh class B or C, tumor size 4 cm or larger, 5 or more tumors, portal vein invasion, and an alpha-fetoprotein (AFP) level greater than 83 ng/mL. [11] Conventional and drug-eluting bead chemoembolization have been found to have a limited impact on liver function, and tumor response is not dependent on type of embolization used. [2, 3, 4, 5, 12, 13, 14]
Diagnostic imaging depicts not only the primary hepatic disease but also ascites, lymph node metastases, and thrombosis of portal or hepatic veins. Confirming portal vein patency is important because portal vein thrombosis is a relative contraindication to chemoembolization. [15, 16] If portal flow via collateral vessels remains hepatopetal, embolization may be better tolerated. Imaging also plays an important role in evaluating the effectiveness of interventional therapy.
Preferred examination
The imaging strategy in HCC depends on the clinical question to be answered and the treatment options available. Angiography is an essential part of the workup performed before embolization or chemoembolization, although most centers proceed to the embolization procedure if no contraindications are present. In patients with a known primary malignancy, such as colorectal cancer or islet cell tumors, an initial investigation includes an ultrasonographic examination followed by spiral or multisection, 3-phase, contrast-enhanced CT scanning. [6, 7, 8, 10, 17, 18, 19]
Contrast-enhanced ultrasound is useful in determining the differences between the grades of HCCs. In studies using auto-tracking contrast quantification software, the time to peak, the contrast-enhanced time, and the wash-out time were longer for well-differentiated hepatocellular lesions, and the enhancement slope and clearance slope were lower than that of moderately to poorly differentiated carcinomas. [3, 17, 20, 21, 22]
Magnetic resonance imaging (MRI) and radionuclide scanning are useful in confirming the diagnosis, particularly the diagnosis of benign lesions, such as hemangiomas and focal nodular hyperplasia. These lesions are increasingly encountered in the setting of malignant disease. The multiplanar capability of MRI is particularly helpful in determining the exact anatomic location of the lesions. In the setting of HCC, a protocol similar to that used for liver metastasis is performed. [3, 6, 7, 23, 24, 25]
Posttreatment surveillance by MRI or CT is frequently delayed by at least 4-6 weeks after each treatment cycle to allow for maturation of granulation tissue, to limit lipiodol-associated artifacts, and to help separate viable tumor from postembolization inflammation. [18, 19, 26]
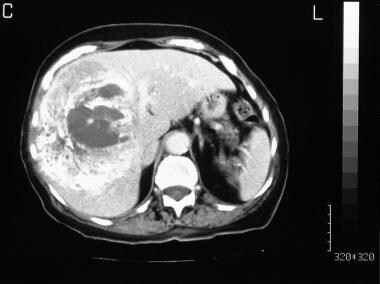
(An axial computed tomography (CT) scan of an HCC is shown below.)
 Contrast-enhanced axial CT scan through the liver in the portal venous phase in an 88-year-old woman who presented with right upper quadrant discomfort. Scan shows a 13-cm mass occupying the right lobe of the liver; it displaces the portal vein medially. Results of laparoscopic biopsy confirmed the mass to be a well-differentiated hepatocellular carcinoma in a noncirrhotic liver.
Contrast-enhanced axial CT scan through the liver in the portal venous phase in an 88-year-old woman who presented with right upper quadrant discomfort. Scan shows a 13-cm mass occupying the right lobe of the liver; it displaces the portal vein medially. Results of laparoscopic biopsy confirmed the mass to be a well-differentiated hepatocellular carcinoma in a noncirrhotic liver.
Peptide-receptor radionuclide therapy (PRRT) is reserved for treatment of unresectable or metastatic gastroenteropancreatic neuroendocrine tumors (GEP NETs). Campana et al conducted a study to determine the time to progression of patients treated with PRRT and to identify the prognostic factors related to treatment response. The study concluded that low tumor burden and a low proliferation index represent independent prognostic factors for long progression-free survival, while previous transcatheter arterial chemoembolization (TACE) techniques represent independent prognostic factors for early tumor progression and shorter progression-free survival. The data derived from the study suggest that TACE techniques to reduce the hepatic tumor burden should be avoided. [27]
Liu et al retrospectively studied 246 consecutive patients with primary Budd-Chiari syndrome (BCS) with the view to analyze the imaging features of BCS-associated HCC and the results of angioplasty/stenting of hepatic veins/inferior vena cava and TACE. The study concluded that BCS patients with inferior vena cava block and stricture of hepatic venous outflow tract seem to be associated with HCC. A single, large, irregular nodule with a peripheral location appears to be HCC. [28]
Bile duct strictures are a known complication of TACE. Anastomosis between A1 or A4 and other branches has been shown to be frequently associated with bile duct strictures 2-8 months after TACE of the bile duct branch. [29]
A review by Rempp and associates suggested that radiofrequency ablation should be used in patients with early-stage HCC with up to 3 lesions with a tumor diameter of 3 cm or less and for patients with nonresectable liver metastasis. [30]
CT SCAN
Postprocedural imaging
Follow-up CT scans are obtained approximately 10-14 days after chemoembolization. An early scan may be acquired if complications, such as nontarget embolization, are suspected. Because the chemotherapeutic agent is mixed with lipiodol, CT scans of a tumor reveal dense opacification associated with necrosis (see the image below). Along with nontarget embolization, CT scans also demonstrate such complications as the development of ascites and pleural effusions. When only polyvinyl alcohol embolization is performed, as in cases of hepatic carcinoid, postembolization CT scans demonstrate only tumor necrosis. [31] In patients with hepatocellular carcinoma (HCC), if the embolization procedure is successful, the postprocedural CT scan will show a lipiodol uptake greater than 50% in necrotic tumor. In these cases, the embolization is repeated in 6-8 weeks. If the lipiodol uptake is less than 50%, the authors repeat the CT scan in 6-8 weeks. [8, 32, 33, 34]
 Contrast-enhanced, axial CT scan through the liver, obtained 10 days after chemoembolization, shows intensely concentrated lipiodol within the hepatocellular carcinoma. Note the considerable central tumor necrosis.
Contrast-enhanced, axial CT scan through the liver, obtained 10 days after chemoembolization, shows intensely concentrated lipiodol within the hepatocellular carcinoma. Note the considerable central tumor necrosis.
In a study by Tamandl et al, CT perfusion was found to detect lesions with complete response one day after TACE for HCC and to be a feasible tool for early response assessment. Blood flow, blood volume, time to start, arterial liver perfusion, portal liver perfusion, and hepatic perfusion index were measured, and it was determined that out of 41 lesions, 21 (51%) had a complete remission and 5 (12%) had a partial response. [35]
MRI
MRI and radionuclide scanning are useful in confirming a diagnosis, particularly the diagnosis of benign lesions, such as hemangiomas and focal nodular hyperplasia. These lesions are increasingly encountered in the setting of malignant disease. The multiplanar capability of MRI is particularly helpful in determining the exact anatomic location of the lesions. In the setting of hepatocellular carcinoma, a protocol similar to that used for liver metastasis is performed. [6, 7, 23, 24]
Preoperative tumor features on MRI have also been used to predict the response of HCC after transcatheter arterial chemoembolization (TACE) combined with high-intensity focused ultrasound (HIFU) treatment. A study of 188 patients who underwent TACE/HIFU treatment reported that a finding of irregular margins in tumors 2-5 cm were closely related to early noncomplete response (NCR). Irregular margins, arterial peritumoral enhancement, and abnormal alpha-fetoprotein (AFP) were independent predictors of early NCR in tumors greater than 5 cm. [25]
Angiography
Angiography is an essential part of the workup performed before embolization or chemoembolization, although most centers proceed to the embolization procedure if no contraindications are present. Angiography is usually performed by placing a 5F to 6F catheter through a sheath via the right or left femoral artery. The catheter should be able to accept the insertion of a 3F coaxial microcatheter. A celiac-axis and superior mesenteric angiogram is first obtained to identify common variations in the blood supply to the liver and to check for patency of the portal vein.
(Angiograms obtained before and after chemoembolization are seen below.)
 Arterial/early capillary phase of a celiac-axis angiogram shows extensive neovascularity in the mass, with stretching of the vessels around the mass.
Arterial/early capillary phase of a celiac-axis angiogram shows extensive neovascularity in the mass, with stretching of the vessels around the mass.
 Portal venous phase of a celiac-axis angiogram (same patient as in the previous image) shows patent splenic and portal veins; therefore, the patient is a suitable candidate for chemoembolization.
Portal venous phase of a celiac-axis angiogram (same patient as in the previous image) shows patent splenic and portal veins; therefore, the patient is a suitable candidate for chemoembolization.
 Selective hepatic angiogram obtained after chemoembolization shows a complete shutdown of the neovascularity and pruning of the stretched peripheral vessels.
Selective hepatic angiogram obtained after chemoembolization shows a complete shutdown of the neovascularity and pruning of the stretched peripheral vessels.
Embolization of parasitized extrahepatic arteries (EHAs) to reestablish intrahepatic arterial inflow to hepatic tumors was found to be safe and effective in a retrospective analysis of 201 patients. [36] The procedure successfully delivered yttrium-90 microspheres to tumors previously perfused by parasitized EHAs.
-
Contrast-enhanced axial CT scan through the liver in the portal venous phase in an 88-year-old woman who presented with right upper quadrant discomfort. Scan shows a 13-cm mass occupying the right lobe of the liver; it displaces the portal vein medially. Results of laparoscopic biopsy confirmed the mass to be a well-differentiated hepatocellular carcinoma in a noncirrhotic liver.
-
Arterial/early capillary phase of a celiac-axis angiogram shows extensive neovascularity in the mass, with stretching of the vessels around the mass.
-
Portal venous phase of a celiac-axis angiogram (same patient as in the previous image) shows patent splenic and portal veins; therefore, the patient is a suitable candidate for chemoembolization.
-
Selective hepatic angiogram obtained after chemoembolization shows a complete shutdown of the neovascularity and pruning of the stretched peripheral vessels.
-
Contrast-enhanced, axial CT scan through the liver, obtained 10 days after chemoembolization, shows intensely concentrated lipiodol within the hepatocellular carcinoma. Note the considerable central tumor necrosis.








