Practice Essentials
The term "stress fracture" refers to the failure of the skeleton to withstand submaximal forces over time. Two forms of stress fracture have been defined: fatigue fracture and insufficiency fracture. [1] A stress fracture is a partial or complete fracture caused by repeated stress lower than that required to cause a fracture in a single event. These injuries account for 0.7-20% of all sports medicine clinic injuries, with the highest incidence being in track-and-field athletes. [2, 3] Fatigue fracture is classically described in military recruits and runners in whom normal bone is exposed to repeated abnormal stresses. [4] The injury is usually seen in the lower extremities, but it has also been reported in the upper extremities and the ribs. [5, 6] The most common locations for stress fractures include the tibia, metatarsals, fibula, and navicular bones. [6, 7] Insufficiency fracture results when normal stress is applied to abnormal bone (such as bone with osteoporosis or Paget disease).
(See the images below.)
 A cortical disruption (arrow), along with a fine line of increased density, is noted. This is consistent with the appearance of sclerotic bone following a stress fracture.
A cortical disruption (arrow), along with a fine line of increased density, is noted. This is consistent with the appearance of sclerotic bone following a stress fracture.
 T1-weighted sagittal magnetic resonance image from the ankle. A stress fracture is noted as a linear area of low signal intensity in the calcaneus. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
T1-weighted sagittal magnetic resonance image from the ankle. A stress fracture is noted as a linear area of low signal intensity in the calcaneus. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
Imaging modalities
The first examination in evaluating a possible stress fracture is the plain film. If the plain film turns out to be negative, which is quite frequently the case, magnetic resonance imaging (MRI) or bone scintigraphy should be considered to further evaluate the clinical finding. The advantage of MRI is better spatial resolution and specificity. MRI can easily detect minor stress reactions, such as bone contusions on a short T1 inversion recovery (STIR) sequence or a fat-suppressed T2-weighted fast spin echo (FSE) sequence. If, in addition, the typical linear low signal component is identified, the classic criteria for a stress fracture are present. [1, 8, 9, 10]
Plain radiographs often are negative in the early stages of the evolution of stress fractures. MRI is very sensitive in the immediate documentation of the bony structures' stress reactions. It is well documented that MRI is able to show even minor stress changes (for example, after a marathon) at a much earlier stage than that of the actual stress fracture. Indeed, it seems sometimes to be an arbitrary cutoff between a severe bone contusion, which will contain multiple microfractures, and the actual stress fracture, which requires a linear component.
In a sacral fracture (see the images below), MRI can obtain a screening of the pelvis with different sequences (coronal and axial STIR and T1 SE).
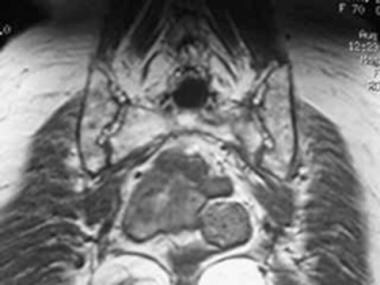 An area of hyposignal is noted in the T1 sequence at the left sacrum, at the site of an acute stress fracture.
An area of hyposignal is noted in the T1 sequence at the left sacrum, at the site of an acute stress fracture.
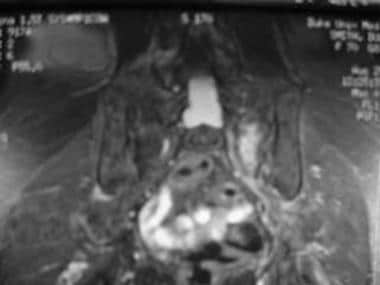 The acute stress fracture in the left sacrum appears as a linear area of hypersignal with adjacent edema.
The acute stress fracture in the left sacrum appears as a linear area of hypersignal with adjacent edema.
In addition, MRI is sensitive enough to detect further malignant entities causing a marrow replacement, which would make the bone prone to insufficiency fracture.
Another approach can be 3-phase skeletal scintigraphy with technetium-99m (99mTc) methylene diphosphonate (MDP). In an adult, typically about 25 mCi of 99mTc MDP is injected intravenously, with the patient positioned under the gamma camera. The dose for pediatric patients is adjusted accordingly. It is important to image the contralateral normal side as well. The first phase of the study is the dynamic phase, and rapid-sequence dynamic images are obtained for approximately 1 minute. The second phase is the blood pool phase. Static planar images are obtained immediately after the dynamic images. The third-phase images consist of static planar images obtained 2-3 hours later. Compared with MRI, the advantage of scintigraphy is that the entire skeleton can be screened.
Scintigraphic changes can precede plain film changes by up to a few weeks because the increased osteoblastic activity associated with a stress fracture is more easily detected by scintigraphy. Bone scintigraphy and MRI have been found, in some studies, to be comparable in the evaluation of stress fractures, although MRI has been shown to provide a better evaluation of soft tissues around fractures. Bone scintigraphy can show increased bone remodeling in the early stages, as well as allow early assessment of changes in bone metabolism. [11, 12, 13, 14, 15, 16, 15]
Single-photon emission computerized tomography (SPECT) can help detect early changes, showing stress reactions before they are seen on plain films. If results are negative, a fracture is unlikely. [17, 18, 19, 20]
Imaging Guidelines
The American College of Radiology (ACR) Appropriateness Criteria for imaging stress fractures includes the following recommendations [21] :
-
Radiographs are the preferred initial imaging for suspected fatigue fractures and suspected insufficiency fractures in the pelvis, hip, or lower extremities.
-
Follow-up MRI without contrast should be performed if the initial radiograph is negative for hip fatigue fractures or insufficiency fractures of the pelvis or hip. CT without contrast is less sensitive but may be considered an alternative for follow-up imaging of insufficiency fractures.
-
If initial radiographs for suspected fatigue fractures are negative in any site other than the hip, radiographs may be repeated after 10-14 days, or MRI without contrast may be performed based on the location and risk of complications.
-
If initial radiographs for suspected insufficiency fracture are negative in any site other than the hip and pelvis, MRI without contrast is preferred. Radiographs repeated after 10-14 days is less sensitive but may be considered an alternative for follow-up imaging.
-
MRI without contrast is appropriate for initial return-to-play evaluations.
-
In pregnant women with suspected stress fracture, MRI without contrast is the initial imaging test of choice for the pelvis. Radiographs are the initial imaging test for the long bones, with follow-up MRI if the radiographic findings are negative or equivocal.
Radiography
On plain film radiography, stress fractures usually appear as sclerosed areas and often are oriented linearly. A focal periosteal reaction or a cortical break also may be present. [22] A history of repetitive stress may not always be obtained. Occasionally, a stress fracture may have the appearance of aggressive periostitis without a linear sclerosis. A biopsy of these lesions may at times result in unwarranted therapy if the histopathology is confused with malignancy.
This approach is still appropriate, considering the fact of a potential differential diagnosis, which could include any of a variety of other underlying bone diseases that could result in stress fracture. These include a bone cyst, osteoid osteoma, or malignant entities, such as osteosarcoma.
Plain film radiography can also help to determine the chronicity of the stress fracture, based on the fact that an acute stress fracture will present with a fine line of lucency, whereas a subacute or old stress fracture will demonstrate a fine line of increased density consistent with sclerotic dead bone.
(See the image below.)
 A cortical disruption (arrow), along with a fine line of increased density, is noted. This is consistent with the appearance of sclerotic bone following a stress fracture.
A cortical disruption (arrow), along with a fine line of increased density, is noted. This is consistent with the appearance of sclerotic bone following a stress fracture.
The degree of confidence is low; plain film findings often are normal, especially in the early stages of injury, and they may therefore delay appropriate therapy. Initial radiographs usually are negative. Even follow-up studies are positive in only 50% of patients. [23]
The delay in the appearance of findings can result in false negatives and can hold up therapy until the diagnosis is made by scintigraphy. False-positive results are less common, but as previously mentioned, the findings may at times mimic malignancy. Plain films still can be used, as an unexpected finding can be discovered to explain the patient's problems.
In a study of 62,371 soldiers in the Israeli Defense Forces over 4 years, 3672 (5.9%) were diagnosed with clinical stress fractures. Radiographs were positive for stress fractures in only 11.1% of tests, whereas bone scans showed evidence of stress fractures in 49.7%. [24]
Computed Tomography
Computed tomography (CT) scanning occasionally may be performed to diagnose stress fractures. Disruption of the bony cortex usually can be demonstrated through CT scanning, and evidence of periostitis also can be detected in this way. The sensitivity of CT scans is higher than that of plain films. However, compared with MRI or bone scanning, the sensitivity of CT scanning with regard to stress reactions and fractures is rather low, resulting in a high rate of false negatives. [25]
Thus, in the appropriate clinical setting, CT scanning can be skipped, and either MRI or a bone scan can be performed. Repeat CT scanning is not an attractive alternative, although it can result in the correct diagnosis because of the interval development of osteonecrosis.
Magnetic Resonance Imaging
Low signal on T1- and T2-weighted images is the classic appearance of a stress fracture on magnetic resonance images. [26, 27, 28, 8]
MRI is often useful in patients with severe osteoporosis, in whom skeletal scintigraphy may produce false negatives because of generalized poor uptake of the tracer. MRI is highly sensitive for the detection of bone marrow changes. Better anatomic resolution also is an advantage. [29]
This is particularly helpful in the case of small joints of the hands and feet, in which the relatively poor spatial resolution of the radionuclide bone scan can be a disadvantage.
MRI also has the advantage of distinguishing between arthritis, osteomyelitis, and osteonecrosis, all of which potentially can have the same appearance on a bone scan.
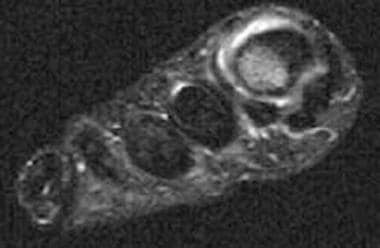
Typically, the stress fracture appears as a low signal band that arises from the cortex of the bone and extends perpendicular to the surface of the bone.
(See the images below.)
 T1-weighted sagittal magnetic resonance image from the ankle. A stress fracture is noted as a linear area of low signal intensity in the calcaneus. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
T1-weighted sagittal magnetic resonance image from the ankle. A stress fracture is noted as a linear area of low signal intensity in the calcaneus. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
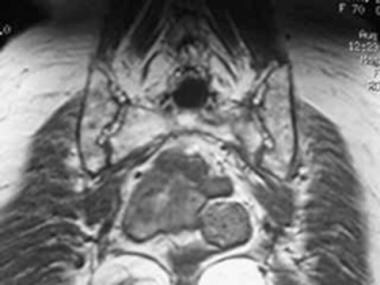 An area of hyposignal is noted in the T1 sequence at the left sacrum, at the site of an acute stress fracture.
An area of hyposignal is noted in the T1 sequence at the left sacrum, at the site of an acute stress fracture.
If imaging is performed soon after the onset of symptoms (typically within 4 weeks), a high signal area often can be observed in the T2-weighted images and represents associated edema or hemorrhage. (See the image below.)
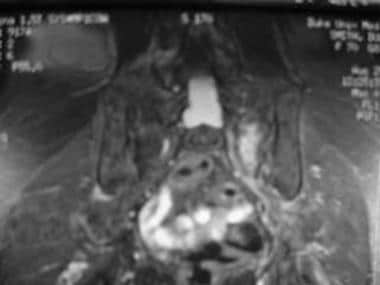 The acute stress fracture in the left sacrum appears as a linear area of hypersignal with adjacent edema.
The acute stress fracture in the left sacrum appears as a linear area of hypersignal with adjacent edema.
Fat suppression sequences are very sensitive for edema and can help to confirm subtle findings on T1 and T2 images. An image from a STIR is demonstrated in the image below, in which a bone bruise and surrounding soft-tissue edema show high signal areas.
 Short T1 inversion recovery sequence coronal images reveal a well-circumscribed area of increased signal intensity in the lateral aspect of the first metatarsal. This is consistent with a bone bruise. Also seen is a small amount of surrounding high signal intensity, which is consistent with soft-tissue edema. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
Short T1 inversion recovery sequence coronal images reveal a well-circumscribed area of increased signal intensity in the lateral aspect of the first metatarsal. This is consistent with a bone bruise. Also seen is a small amount of surrounding high signal intensity, which is consistent with soft-tissue edema. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
Shin splints
Shin splints are a condition commonly associated with stress fractures. They are believed to result from periosteal reaction caused by microperiosteal tears from abnormal stress mediated by Sharpey fibers, which connect the tendons to the bones. Shin splints usually do not progress to further trauma to the bone. Repeated microperiosteal tears with the associated periosteal reaction and healing response can cause increased tracer uptake in a technetium-99m (99mTc) methylene diphosphonate (MDP) bone scan.
On T2-weighted magnetic resonance images, any form of microtrauma would result in a signal increase. Fat suppression is helpful in distinguishing the signal abnormalities from the surrounding fat marrow. In a T1-weighted series, a low signal area is demonstrated corresponding to the finding in the T2-weighted images.
Degree of confidence
Confidence in the imaging findings is usually high in a patient who is clinically believed to have a stress fracture. MRI findings can be positive within 24 hours of the onset of symptoms. Radionuclide bone scans can take longer to become positive, particularly in patients with osteoporosis.
Other entities, such as osteomyelitis or a neoplasm, can cause extensive bone marrow edema. In addition, the detection of stress responses in hematopoietic marrow can be more challenging.
The linear low signal finding usually is helpful in identifying stress fractures.
Nuclear Imaging
Typically, stress fractures are associated with hyperemia in the first 2 phases of the 3-phase bone scan. This is manifested by increased tracer activity at the affected site.
If an image of the contralateral side is available, the hyperemia is easier to detect. While detection of hyperemia is not difficult in adults, increased tracer activity around the epiphyses of pediatric patients may be difficult to detect in the absence of contralateral images.
The first phase demonstrates increased blood flow in the arterial phase, and the second phase demonstrates the presence of tissue hyperemia. The third phase demonstrates increased osteoblastic activity in response to the stress fracture. [9, 10]
(See the images below.)
 This patient had severe pain of the left heel. Radiographs were normal. Three-phase bone scintigraphy reveals increased perfusion to the left heel (top row), increased blood pool activity in the second phase (middle row), and increased tracer uptake in the left calcaneum in the third phase (bottom row). The findings are consistent with stress fracture of the left calcaneum. The marker is on the right side. A smaller focus of tracer uptake also is seen in the left heel. This is probably because of degenerative change. The patient was asymptomatic at this site.
This patient had severe pain of the left heel. Radiographs were normal. Three-phase bone scintigraphy reveals increased perfusion to the left heel (top row), increased blood pool activity in the second phase (middle row), and increased tracer uptake in the left calcaneum in the third phase (bottom row). The findings are consistent with stress fracture of the left calcaneum. The marker is on the right side. A smaller focus of tracer uptake also is seen in the left heel. This is probably because of degenerative change. The patient was asymptomatic at this site.
 This patient had increased her hours of running to prepare for a marathon. Her left foot was hurting. Radiographs were normal. The perfusion images are not available, but the blood pool images (top row) clearly reveal hyperemia of the left foot. The delayed static images demonstrate intense uptake of tracer in the third metatarsal. The scan findings are consistent with stress fracture of the third metatarsal on the left side. The marker is on the right side.
This patient had increased her hours of running to prepare for a marathon. Her left foot was hurting. Radiographs were normal. The perfusion images are not available, but the blood pool images (top row) clearly reveal hyperemia of the left foot. The delayed static images demonstrate intense uptake of tracer in the third metatarsal. The scan findings are consistent with stress fracture of the third metatarsal on the left side. The marker is on the right side.
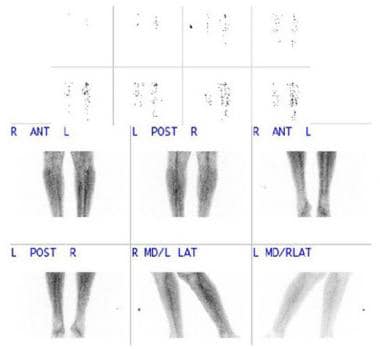 This patient was a marathon runner who complained of pain in his left leg. Radiographs were normal. The top 2 rows are perfusion images; there is increased perfusion to the left leg. The bottom 2 rows are blood pool images, demonstrating increased blood pool activity in the left leg.
This patient was a marathon runner who complained of pain in his left leg. Radiographs were normal. The top 2 rows are perfusion images; there is increased perfusion to the left leg. The bottom 2 rows are blood pool images, demonstrating increased blood pool activity in the left leg.
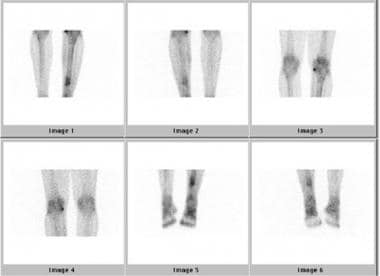 Delayed images of the same patient as in the previous image. Increased tracer uptake is noted just below the midpoint of the shaft of the left tibia. The findings are consistent with a stress fracture of the left tibia. Note increased tracer activity from degenerative changes at the medial portion of the right knee. The patient was asymptomatic at this site.
Delayed images of the same patient as in the previous image. Increased tracer uptake is noted just below the midpoint of the shaft of the left tibia. The findings are consistent with a stress fracture of the left tibia. Note increased tracer activity from degenerative changes at the medial portion of the right knee. The patient was asymptomatic at this site.
Bilateral fractures of the sacral ala can produce a pattern of tracer uptake that is often termed the Honda sign. The hyperemia observed in the first 2 phases is most intense during the first 2-3 weeks and then gradually diminishes. The increased tracer uptake observed in the third phase remains positive much longer. While some lesions resolve in approximately 6 months, it is not uncommon for lesions to be scintigraphically detectable even after 1 year, although the intensity and size of the lesion gradually diminish.
Stress fractures are relatively easy to diagnose by skeletal scintigraphy. Confidence is high. A normal bone scan reliably excludes the diagnosis of stress fracture. [30, 31]
Acute traumatic fractures can reveal somewhat similar findings on skeletal scintigraphy, but the uptake pattern in stress fractures usually demonstrates a smaller area of increased tracer activity than does the uptake pattern of fractures resulting from acute trauma. In patients with multiple stress fractures, an accurate determination of the age of the fracture may not always be possible.
Particular attention must be given to epiphyses in children, as the physiologic increased uptake of tracer in the epiphyseal region can easily mask increased tracer activity caused by osteoblastic activity.
In patients with severe osteoporosis, tracer uptake by the bone may be too low, and false-negative results may be produced.
Bone neoplasms can have a tracer uptake pattern similar to that of stress fractures. It is important not to confuse the 2 of these. While the history alone is sufficient in most cases to resolve the issue, correlation of the findings with that of plain film radiography should be adequate in almost all situations.
Scintigraphic changes can precede plain film changes by up to a few weeks because the increased osteoblastic activity associated with a stress fracture is more easily detected by scintigraphy. Bone scintigraphy and MRI have been found, in some studies, to be comparable in the evaluation of stress fractures, although MRI has been shown to provide a better evaluation of soft tissues around fractures. Bone scintigraphy can show increased bone remodeling in the early stages, as well as allow early assessment of changes in bone metabolism. [11, 12, 16, 15]
In nuclear bone scans, symmetrical positioning of the limbs is crucial. A limb that is nearer to the gamma camera head as compared with the contralateral side will show an apparent increase of tracer uptake, and this can cause diagnostic confusion.
Single-photon emission computerized tomography (SPECT) can help detect early changes, showing stress reactions before they are seen on plain films. If results are negative, a fracture is unlikely. [17, 18, 19, 20]
In a study of 62,371 soldiers in the Israeli Defense Forces over 4 years, 3672 (5.9%) were diagnosed with clinical stress fractures. Radiographs were positive for stress fractures in only 11.1% of tests, whereas bone scans showed evidence of stress fractures in 49.7%. [24]
-
A cortical disruption (arrow), along with a fine line of increased density, is noted. This is consistent with the appearance of sclerotic bone following a stress fracture.
-
T1-weighted sagittal magnetic resonance image from the ankle. A stress fracture is noted as a linear area of low signal intensity in the calcaneus. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
-
An area of hyposignal is noted in the T1 sequence at the left sacrum, at the site of an acute stress fracture.
-
The acute stress fracture in the left sacrum appears as a linear area of hypersignal with adjacent edema.
-
Short T1 inversion recovery sequence coronal images reveal a well-circumscribed area of increased signal intensity in the lateral aspect of the first metatarsal. This is consistent with a bone bruise. Also seen is a small amount of surrounding high signal intensity, which is consistent with soft-tissue edema. Courtesy of Drs. Mike Handlon, Jennifer Keilp, and Molly Hester.
-
This patient had severe pain of the left heel. Radiographs were normal. Three-phase bone scintigraphy reveals increased perfusion to the left heel (top row), increased blood pool activity in the second phase (middle row), and increased tracer uptake in the left calcaneum in the third phase (bottom row). The findings are consistent with stress fracture of the left calcaneum. The marker is on the right side. A smaller focus of tracer uptake also is seen in the left heel. This is probably because of degenerative change. The patient was asymptomatic at this site.
-
This patient had increased her hours of running to prepare for a marathon. Her left foot was hurting. Radiographs were normal. The perfusion images are not available, but the blood pool images (top row) clearly reveal hyperemia of the left foot. The delayed static images demonstrate intense uptake of tracer in the third metatarsal. The scan findings are consistent with stress fracture of the third metatarsal on the left side. The marker is on the right side.
-
This patient was a marathon runner who complained of pain in his left leg. Radiographs were normal. The top 2 rows are perfusion images; there is increased perfusion to the left leg. The bottom 2 rows are blood pool images, demonstrating increased blood pool activity in the left leg.
-
Delayed images of the same patient as in the previous image. Increased tracer uptake is noted just below the midpoint of the shaft of the left tibia. The findings are consistent with a stress fracture of the left tibia. Note increased tracer activity from degenerative changes at the medial portion of the right knee. The patient was asymptomatic at this site.










