Practice Essentials
In small-bowel obstruction imaging, certain radiologic investigations can be used to confirm the diagnosis and severity of the obstruction, but not its etiology. Other imaging modalities are aimed at determining the cause of obstruction. [1] Conventional plain radiography (see the images below) is the investigation of choice for patients with suspected small-bowel obstruction. This study should always be performed first. [1]
 Plain abdominal radiograph in a 6-year-old boy who presented with vomiting and acute pain in the right iliac fossa. The loops of the small bowel are dilated, and small calcific nodules are seen in the right iliac fossa. These findings are suggestive of appendicoliths. At laparotomy, an appendiceal mass was found; this had caused the small-bowel obstruction.
Plain abdominal radiograph in a 6-year-old boy who presented with vomiting and acute pain in the right iliac fossa. The loops of the small bowel are dilated, and small calcific nodules are seen in the right iliac fossa. These findings are suggestive of appendicoliths. At laparotomy, an appendiceal mass was found; this had caused the small-bowel obstruction.
 Plain abdominal radiograph in a 9-year-old patient with a past history of appendicitis complicated by peritonitis who presented with abdominal pain and vomiting. The clinical diagnosis was small-bowel obstruction resulting from adhesions. This radiograph shows markedly distended loops of small bowel, with effacement of the valvulae in the mid abdomen. The child recovered with conservative treatment.
Plain abdominal radiograph in a 9-year-old patient with a past history of appendicitis complicated by peritonitis who presented with abdominal pain and vomiting. The clinical diagnosis was small-bowel obstruction resulting from adhesions. This radiograph shows markedly distended loops of small bowel, with effacement of the valvulae in the mid abdomen. The child recovered with conservative treatment.
 This plain abdominal radiograph of a 55-year-old woman presenting with features of intestinal obstruction shows dilated loops of the small bowel associated with thickened edematous valvulae conniventes and a strangulated left inguinal hernia (arrow).
This plain abdominal radiograph of a 55-year-old woman presenting with features of intestinal obstruction shows dilated loops of the small bowel associated with thickened edematous valvulae conniventes and a strangulated left inguinal hernia (arrow).
 Plain abdominal radiograph of the abdomen in a 72-year-old man with a history of intermittent abdominal pain over several years that settled spontaneously. On this occasion, his pain was severe. The abdominal radiograph shows dilated loops of small bowel, but the concentration of several loops of small bowel in the right hypochondrium should be noted as this finding is suggestive of malrotation. At surgery, a midgut volvulus caused by malrotation was found. The patient's age is unusual for those presenting with a midgut volvulus.
Plain abdominal radiograph of the abdomen in a 72-year-old man with a history of intermittent abdominal pain over several years that settled spontaneously. On this occasion, his pain was severe. The abdominal radiograph shows dilated loops of small bowel, but the concentration of several loops of small bowel in the right hypochondrium should be noted as this finding is suggestive of malrotation. At surgery, a midgut volvulus caused by malrotation was found. The patient's age is unusual for those presenting with a midgut volvulus.
The unique capabilities of CT scanning (see the images below) make it an important diagnostic tool when a specific clinical answer is sought. Studies have shown the superiority of CT scanning in revealing not only the site of the obstruction but also its cause. CT scans may demonstrate signs of ischemia as well. [2, 3, 4, 5]
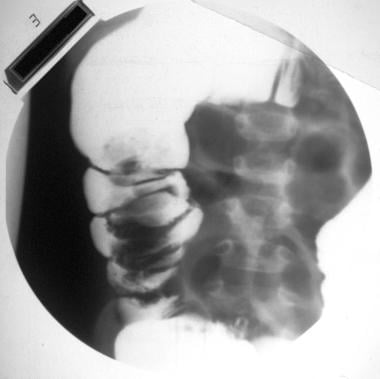
 A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
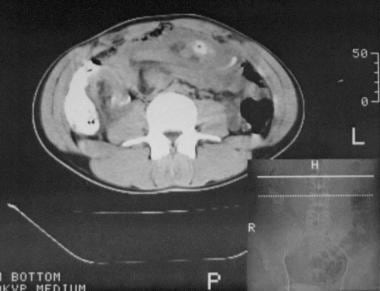
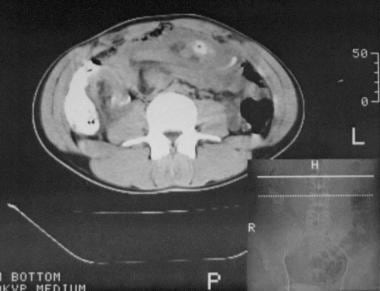
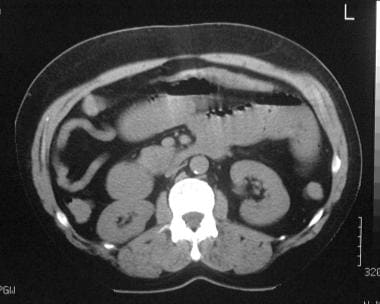
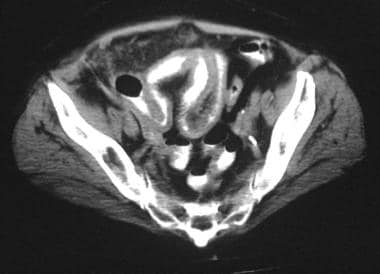
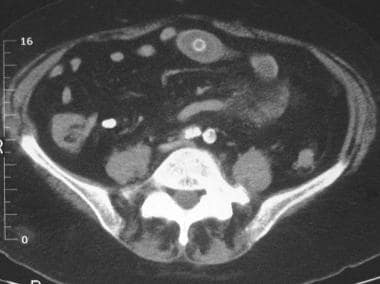
 A CT scan of a 36-year-old woman with Gardner syndrome presented with features of small-bowel obstruction. The axial contrast-enhanced CT scan through the midabdomen shows an extrinsic mass compressing a loop of small bowel. At laparotomy, a desmoid tumor of the mesentery was found; this caused the small-bowel obstruction.
A CT scan of a 36-year-old woman with Gardner syndrome presented with features of small-bowel obstruction. The axial contrast-enhanced CT scan through the midabdomen shows an extrinsic mass compressing a loop of small bowel. At laparotomy, a desmoid tumor of the mesentery was found; this caused the small-bowel obstruction.
Vercruysse et al outlined the following approach to evaluation of small-bowel obstruction in adults [3] :
-
First-line imaging in patients with abdominal pain is an acute abdominal x-ray series. Signs of bowel ischemia such as pneumatosis, portal venous gas, or pneumoperitoneum should prompt urgent surgical evaluation.
-
Stable patients should also undergo CT of the abdomen and pelvis with IV contrast. Consider the risk of contrast-induced nephropathy in patients with chronic kidney disease. Do not use oral contrast in patients with suspected small-bowel obstruction.
-
A transition zone is required for the diagnosis of small-bowel obstruction.
The American College of Radiology has published the following CT guidelines for imaging small-bowel obstruction [4] :
-
CT of the abdomen and pelvis with IV contrast is usually appropriate for the initial imaging of a suspected small-bowel obstruction with an acute presentation.
-
CT of the abdomen and pelvis with IV contrast or CT enterography is usually appropriate for the imaging of a suspected intermittent or low-grade small-bowel obstruction with an indolent presentation. These 2 procedures are equivalent alternatives (ie, only one will be ordered to provide the clinical information to effectively manage the patient’s care). However, CT enterography could be performed as a complementary examination if small-bowel distention aids in accentuating small-bowel pathology that is not initially evident on a CT without oral contrast.
Atri et al studied 99 adult patients who underwent 105 nonenhanced CTs and enhanced CTs and found that the 2 procedures had comparable accuracy in diagnosing mechanical small-bowel obstruction and that they can be interpreted by reviewers of varying expertise. Mechanical obstruction was present in 56% (59/105). The average sensitivity, specificity, negative predictive value, positive predictive value, and accuracy for nonenhanced CTs were 88.1%, 77%, 83.0%, 83%, and 83%, respectively, with no significant difference between 3 reviewers (abdominal radiologist, abdominal fellow, second-year radiology resident). The corresponding numbers for enhanced CT were 87.6%, 75%, 82.6%, 82.1%, and 82%, respectively. [6]
O'Daly et al conducted a retrospective review of 88 patients who had acute adhesional small-bowel obstruction and underwent CT, and 58 (66%) were managed conservatively and 30 (34%) underwent surgery. Peritoneal fluid detected on a CT scan (n = 37) was associated more frequently with surgery than conservative management (46% versus 29%). Peritoneal fluid detected on a CT scan was identified as an independent predictor of surgical intervention. According to study findings, such patients are 3 times more likely to require surgery. [7]
Delabrousse et al evaluated the CT findings of 67 patients with small-bowel obstruction to identify characteristics of small-bowel obstruction caused by adhesive bands and that caused by matted adhesions. Closed-loop patterns and a whirl sign were seen only in patients with adhesive bands, and the beak sign and fat notch sign were present more often in patients with adhesive bands. Bowel ischemia and bowel necrosis were also more frequent findings with adhesive bands than with matted adhesions. In patients with matted lesions, the small-bowel feces sign was more frequently seen, and there was a higher rate of accidental bowel perforation. [8]
The relative value of performing conventional small-bowel contrast enema studies versus CT scans in a known or suspected small-bowel obstruction remains underdetermined. Small-bowel enema is preferable to CT scanning when the obstruction is intermittent or incomplete, and it may be of particular value under these circumstances if the plain radiographic findings are normal.
Although ultrasonography (see the image below) has no specific role in the diagnosis of an acute small-bowel obstruction, the technique is widely used in the investigation of acute abdominal pain. The radiologist must be aware of the sonographic appearance of small-bowel obstructions. Sonograms help not only in the diagnosis of an obstruction but also in defining the cause. The sonographic findings differentiate an adynamic ileus from a mechanical obstruction by depicting peristalsis. Ultrasonography has particular advantages in the diagnosis of neonatal small-bowel obstructions. [9, 10]
 Abdominal sonogram in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The sonogram shows a complex mass of concentric rings of alternating hypoechoic and hyperechoic layers surrounding a highly reflective center. The mass was located in the epigastrium.
Abdominal sonogram in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The sonogram shows a complex mass of concentric rings of alternating hypoechoic and hyperechoic layers surrounding a highly reflective center. The mass was located in the epigastrium.
Radionuclide-labeled white blood cell scanning has no specific role in the diagnosis of acute small-bowel obstruction; however, the technique is sensitive and specific in the diagnosis of some of the causes of chronic and incomplete obstruction, such as Crohn disease. Similarly, a specific diagnosis of a carcinoid of the gastrointestinal tract associated with an incomplete obstruction may be achieved by performing imaging with a radionuclide-labeled somatostatin analogue. (See the image below.)
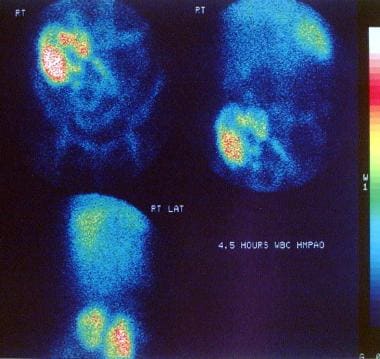 Technetium-99m hexamethylpropyleneamine oxime (99mTc HMPAO)–labeled white blood cell scan in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows active uptake of the radionuclide in the terminal ileum and the cecum/ascending colon indicative of an active inflammatory process. The patient was treated for active Crohn disease.
Technetium-99m hexamethylpropyleneamine oxime (99mTc HMPAO)–labeled white blood cell scan in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows active uptake of the radionuclide in the terminal ileum and the cecum/ascending colon indicative of an active inflammatory process. The patient was treated for active Crohn disease.
The diagnosis of small-bowel obstruction has been achieved by using magnetic resonance imaging (MRI) with T1-weighted sequences combined with antiperistaltic agents and retrograde insufflation. Similar results have been achieved by using subsecond rapid acquisition with relaxation enhancement (RARE) imaging for the delineation of bowel obstruction. Virtual small-bowel imaging is theoretically possible with a spiral CT scanner, but it should be noted that any digital imaging technique enables virtual-reality processing.
Description and classification
Small-bowel obstructions can result from a variety of causes. In parts of Europe, the term "ileus" is applied both to a mechanical small-bowel obstruction and to atony of the bowel related to abdominal surgery or peritonitis; however, in most English-speaking countries, the term "obstruction" is used for a mechanical bowel blockage arising from a structural abnormality that presents a physical barrier to the progression of gut contents. The term "ileus" is reserved for the paralytic or functional variety of gastric obstruction. [11, 12, 13, 14, 15, 16]
Mechanical small-bowel obstruction can be classified into 3 main groups, according to the cause of the intestinal obstruction, as follows:
Intraluminal (eg, foreign bodies, bezoars, food bolus)
Obstruction resulting from lesions in the bowel wall (eg, tumors, Crohn disease)
Extrinsic (eg, adhesions, hernias, volvulus)
Anatomy
The distal part of the duodenum (the jejunum, ileum, and colon proximal to the splenic flexure) develops from the embryologic midgut. A normal small-bowel is approximately 3-6 m in length, although the exact length is often difficult to assess because the small bowel can become considerably elongated or foreshortened in life. In most individuals, the jejunal loops lie in the left hypochondrium, and the ileum lies in the pelvic midline. The terminal ileum is the narrowest part of the small bowel, and peristalsis may be weaker in this segment than in more proximal segments. The valvulae conniventes are more prominent in the jejunum than in the ileum.
The intramural width of the small-bowel may be measured by taking plain abdominal radiographs of a gas-filled lumen. An intramural width of 3 cm is considered abnormal and may indicate obstruction or ileus. This measurement is reduced to 2.5 cm on CT scans. In most healthy adults, the small bowel contains little gas, and only 1 or 2 nondistended gas-filled loops may be seen in the small bowel; however, in the supine position, the duodenum cannot maintain an efficient water trap, and air may pass into the jejunum from the stomach. This is a common observation in patients undergoing intravenous urography who are supine during the procedure. In young children, gas-filled small-bowel loops are common normal findings; however, distention of these loops by gas or fluid should be regarded as abnormal.
The depiction of the small-bowel on sonograms is improved when the small-bowel is filled with water. A water-filled small bowel may occur normally, particularly after meals or the ingestion of a large volume of fluid. Sonography shows fluid-filled tubes lined by an echogenic mucosa that is thrown into folds or valvulae. These folds may lend a ribbed appearance to the inner wall of the bowel. The normal bowel wall is 3-5 mm thick, and normal loops of bowel are yielding and easily deformed during examination. The configuration of the loops may be altered as a result of peristalsis and distention with fluid and air. Progressive pathologic distention makes the bowel more tubular, with a loss of sharp angles between consecutive loops.
Limitations of techniques
The sensitivity of plain radiographic findings in the diagnosis of small-bowel obstruction is approximately 50-66%. When little or no gas is present in the small bowel, a diagnosis of small-bowel obstruction may be overlooked, especially if the condition is proximal. Barium studies should be avoided in patients with suspected perforations or complete small-bowel obstruction.
CT scans have poor sensitivity for low-grade, partial, or incomplete obstruction.
Although sonographic findings may suggest a diagnosis and etiology of small-bowel obstruction, the exact sensitivity of sonography is not known. In addition, bowel gas and obesity pose problems, and the technique remains operator dependent.
Radionuclide findings do not help with a specific diagnosis in bowel obstruction.
MRI is expensive and not universally available. The extent to which MRI will be used clinically in the future depends not only on the availability of an appropriate scanner but also on the overall sensitivity of the procedure compared with time-honored, simple methods, such as plain radiography. The sensitivity of MRI has yet to be established.
The requirement for nasogastric intubation and enteroclysis prior to CT scanning or MRI for virtual small-bowel imaging makes virtual imaging invasive and time consuming.
Medical/legal pitfalls
The most serious consequences of small-bowel obstruction are strangulation with ischemia, necrosis, perforation, peritonitis, and death. The prevalence of strangulated small-bowel obstruction is 5-42% of all patients. Expeditiously investigate clinical suspected strangulation because a delay may be lethal.
The use of barium suspensions for enteroclysis or retrograde examination may cause inspissation of the small bowel and convert a partial obstruction to a complete obstruction; therefore, if CT is available, CT scans should be obtained as an alternative to conventional contrast-enhanced studies.
The presence of a closed-loop obstruction and features of ischemia can be missed, even on CT scans. If an obvious discrepancy exists between CT and clinical findings in patients with obstruction, urgent surgery is mandatory.
Radiography
The following radiologic features may be of assistance in making a diagnosis of small-bowel obstruction:
-
In complete obstruction, loops of small bowel distend within 3-5 hours
-
A bowel larger than 3 cm in diameter is often associated with obstruction; gas and fluid are usually present in the distended small-bowel loops, and gas and fluid levels may be present at the same or different levels in the abdominal cavity [1]
-
In the past, it was suggested that gas and fluid levels at different heights indicated a mechanical obstruction, whereas gas and fluid levels at the same height more likely indicated an adynamic ileus; however, these findings are no longer considered to be reliable signs
-
A discrepancy often exists between the size of the loop of bowel proximal to the obstruction and the size of the loop of bowel distal to the obstruction, which is usually empty or of normal caliber
-
In long-standing obstruction, small-bowel dilatation may mimic a dilated colon; to differentiate the large bowel from the small bowel, an attempt should be made to identify the cecum, which is usually normal in caliber in the early stages of small-bowel obstruction; with time, however, the colon may empty completely and become difficult to depict
-
When distended, loops of small bowel are usually positioned in the center of the abdomen
-
With a proximal jejunal obstruction, a gas-fluid level usually exists in the stomach unless the patient has vomited recently
-
Occasionally, 1 or 2 loops of distended small bowel may be seen in the left upper quadrant
-
The more distal the obstruction, the more numerous the gas-fluid levels; at different heights, the levels reveal a stepladder appearance
-
With the patient in the supine position, fluid-filled loops of small bowel lie posteriorly, and gas-filled loops rise anteriorly and superiorly
-
With the patient erect, gas-filled loops are observed in the upper part of the abdomen
-
Grossly distended fluid-filled loops, particularly of the mid and distal small bowel, may appear as elongated soft-tissue masses
-
Valvulae conniventes (see the image below) are usually closely spaced and should be within 1-4 mm of each other; however, this distance is greater in small-bowel distention; a stretch sign may appear as a result of the erect valvulae conniventes encircling the bowel lumen; even when distended, the valvulae conniventes in the jejunum are usually preserved; in a distended terminal ileum, however, they flatten and the bowel often appears tubelike
-
An increase in peristaltic activity can give rise to the "string-of-beads" sign (see the image below), in which the "beads" represent gas trapped within the valvulae conniventes
-
In some patients, the outer border of the bowel is delineated by mesenteric fat, allowing for the differentiation of fluid-filled small-bowel loops and distention resulting from ascites
-
The small bowel may become massively dilated if the obstruction is chronic; an associated thickening of the intestinal wall often occurs, such that the distance between gas shadows in the small-bowel lumen increases
Less common radiologic signs are seen in specific circumstances. Most closed-loop obstructions (75%) are caused by adhesions. A closed-loop obstruction occurs when a loop of bowel is not decompressed by the caudal passage of gas and fluid. This obstruction may be associated with a U-shaped distended loop of small bowel. This loop may be fixed and does not change position over time. An increasing amount of fluid is incarcerated within the closed loop, and the coffee bean sign (a gas-filled loop) or a pseudotumor (fluid-filled loop) may be seen.
Gallstone ileus (see the images below) is characterized by the presence of a calcified intraluminal stone (often in the terminal ileum), radiologic signs of a small-bowel obstruction above the ileus, and gas in the biliary tree as a result of the cholecystoduodenal fistula. [17]
 An erect plain abdominal radiograph of the abdomen in a 72-year-old woman that shows markedly distended jejunal loops with air-fluid levels. The air overlying the liver and a large laminated gallstone in the right iliac fossa (arrow) should be noted. The features are those of a gallstone ileus.
An erect plain abdominal radiograph of the abdomen in a 72-year-old woman that shows markedly distended jejunal loops with air-fluid levels. The air overlying the liver and a large laminated gallstone in the right iliac fossa (arrow) should be noted. The features are those of a gallstone ileus.
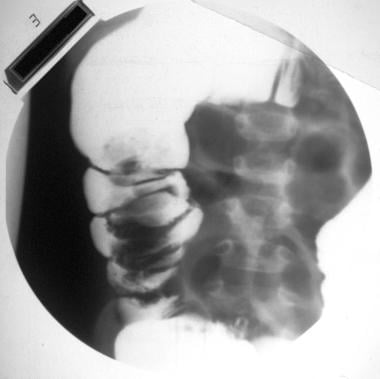
 An upper GI barium study performed through a nasogastric tube in a patient with clinical features of bowel obstruction but a gasless abdomen on plain abdominal radiograph. The barium study shows a fistulous communication between the gallbladder fossa and the duodenum and marked dilatation of the jejunum associated with stretched mucosal folds. At laparotomy, a gallstone ileus was confirmed.
An upper GI barium study performed through a nasogastric tube in a patient with clinical features of bowel obstruction but a gasless abdomen on plain abdominal radiograph. The barium study shows a fistulous communication between the gallbladder fossa and the duodenum and marked dilatation of the jejunum associated with stretched mucosal folds. At laparotomy, a gallstone ileus was confirmed.
In children with an intussusception (see the images below), plain abdominal radiographs may show a soft-tissue mass at the head of the intussusception. Usually, no gas is seen in the colon immediately proximal to the site of obstruction because the intussusceptum occupies the entire lumen. The right lower quadrant is occasionally effaced, and no bowel gas is seen in the region. The intussusceptum may form a large, convex, soft-tissue mass in the region of the ascending or transverse colon, and the large bowel immediately distal to the intussusception is dilated and filled with gas. Radiologic signs of a small-bowel obstruction may be seen above the intussusception.
 Part of a barium enema study in a 2-year-old child presenting with abdominal pain showing a polypoid filling defect within the ascending colon. The filling defect was constant on all images. At laparotomy, a chronic ileocolic intussusception was found.
Part of a barium enema study in a 2-year-old child presenting with abdominal pain showing a polypoid filling defect within the ascending colon. The filling defect was constant on all images. At laparotomy, a chronic ileocolic intussusception was found.
 A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
Intramural gas secondary to ischemia may eventually appear in an obstruction of any etiology. This is a poor prognostic sign.
Conventional barium follow-through examination and enteroclysis
Controversy exists around the type of contrast medium used in patients with suspected small-bowel obstruction. The use of water-soluble contrast material (see the image below), ionic or nonionic, has limitations because it is diluted by the intestinal fluid. As a result, making the diagnosis of obstruction and finding the site of obstruction are difficult. A barium suspension should be used only if no features of peritonism are present.
 Water-soluble contrast upper GI examination in a patient with clinical features of small-bowel obstruction and a history of surgery for large bowel cancer. The contrast-enhanced study shows dilated loops of small bowel, with stretching of the mucosal folds and a narrowed segment ending in a beak (arrow). At surgery, a small-bowel obstruction from extrinsic compression was found to be the result of mesenteric metastases.
Water-soluble contrast upper GI examination in a patient with clinical features of small-bowel obstruction and a history of surgery for large bowel cancer. The contrast-enhanced study shows dilated loops of small bowel, with stretching of the mucosal folds and a narrowed segment ending in a beak (arrow). At surgery, a small-bowel obstruction from extrinsic compression was found to be the result of mesenteric metastases.
One or all of the following radiologic features may assist in the diagnosis:
-
A delay in transit time on a conventional follow-through examination of greater than 12 hours is suggestive of an organic obstruction
-
A snakehead appearance may be observed, which is caused by the bulbous appearance of the bowel proximal to the site of an obstruction; the finding results from the attempts of peristaltic activity to overcome the obstruction
-
Abrupt changes may occur in the caliber of the small bowel at the site of the obstruction, with a dilated contrast-filled small bowel located proximally to the obstruction and a collapsed bowel located distally
-
The beak sign may be detected at the site of an obstruction as barium trickles through a narrow lumen
-
Fixation and kinking of the bowel may be clearly demonstrated
-
Stretched mucosal folds or valvulae conniventes may be apparent
Small-bowel obstruction has been subdivided into 3 groups on the basis of enteroclysis findings, as follows:
-
A low-grade or incomplete obstruction in which flow of contrast agent through the obstruction is sufficient to define the mucosal folds distal to the obstruction well
-
A high-grade obstruction in which stasis occurs and transit of the contrast material is delayed; dilution of the contrast material by intestinal fluid and the passage of minimal contrast material through the obstruction indicate that no details may be defined
-
A complete small-bowel obstruction in which no contrast agent passes the obstructed segment during the 3-24 hours after the start of the examination
Barium enema study
Barium enema (see the images below) has a limited role in patients with small-bowel obstruction. Although examining patients with an ileocecal intussusception or other causes of ileocecal obstruction is possible by using oral contrast material, in these patients barium enema studies are more quickly performed. Barium enema examination is particularly useful if a distal colonic obstruction cannot be excluded by using plain abdominal radiograph findings. In children with intussusception, barium enema studies are not only diagnostic but possibly therapeutic as well.
 Postevacuation image from part of a double-contrast barium enema study in a 47-year-old man presenting with features of small-bowel obstruction. The image shows a coiled-spring appearance in the region of the cecum suggestive of an intussusception (same patient as in the previous 2 images). At laparotomy, an ileocecal intussusception was found in association with a carcinoid tumor of the terminal ileum.
Postevacuation image from part of a double-contrast barium enema study in a 47-year-old man presenting with features of small-bowel obstruction. The image shows a coiled-spring appearance in the region of the cecum suggestive of an intussusception (same patient as in the previous 2 images). At laparotomy, an ileocecal intussusception was found in association with a carcinoid tumor of the terminal ileum.
 An erect abdominal image obtained as part of a double-contrast barium enema study shows multiple fluid levels in the centrally placed small bowel.
An erect abdominal image obtained as part of a double-contrast barium enema study shows multiple fluid levels in the centrally placed small bowel.
 Postevacuation image from part of a barium enema study in a 57-year-old man presenting with colicky abdominal pain and vomiting. The image shows a coiled-spring appearance at the hepatic flexure of the colon typical of an intussusception. At laparotomy, an ileocolic intussusception was found; this was secondary to a carcinoid tumor of the terminal ileum.
Postevacuation image from part of a barium enema study in a 57-year-old man presenting with colicky abdominal pain and vomiting. The image shows a coiled-spring appearance at the hepatic flexure of the colon typical of an intussusception. At laparotomy, an ileocolic intussusception was found; this was secondary to a carcinoid tumor of the terminal ileum.
 Part of a barium enema study in a 2-year-old child presenting with abdominal pain showing a polypoid filling defect within the ascending colon. The filling defect was constant on all images. At laparotomy, a chronic ileocolic intussusception was found.
Part of a barium enema study in a 2-year-old child presenting with abdominal pain showing a polypoid filling defect within the ascending colon. The filling defect was constant on all images. At laparotomy, a chronic ileocolic intussusception was found.
Degree of confidence
Despite its limited sensitivity of 50-66%, plain radiography remains the most useful noninvasive procedure in the radiographic diagnosis of small-bowel obstruction. When plain radiographic findings are combined with the clinical history and the results of physical and laboratory examinations, small-bowel obstruction can usually be diagnosed with confidence. [1, 18]
Differentiating an adynamic ileus from small-bowel obstruction may be particularly difficult, especially in the immediate postoperative period. Eventually, most intestinal obstructions may lead to an adynamic ileus (especially when strangulation is present). This finding is associated with perforation and peritonitis. Under these circumstances, gas may appear in the small bowel proximal to the obstruction, or it may be retained in the atonic colon, leading to diagnostic confusion. Little or no gas in the small bowel may lead to a false-negative diagnosis.
Differentiating a proximal obstruction, a Richter hernia, a gallstone ileus, or a volvulus of the midgut is notably difficult because all of these conditions are demonstrated as a relatively gasless abdomen on plain radiographs. The radiographic features of gallstone ileus are not consistent, as not all stones are radiopaque, and not all choledochoenteric fistulas allow reflux of air into the biliary tree. Gallstone ileus is one condition that causes accumulation of fluid rather than gas within the obstructed bowel; therefore, gallstone ileus should always be considered in the differential diagnosis of small-bowel obstruction accompanied by a relatively gasless abdomen.
In large-bowel obstruction, small-bowel dilatation may occur if the ileocecal valve is patent; this is a potential cause of confusion.
Computed Tomography
CT scanning is recommended when the clinical findings and the initial plain radiographs are inconclusive or when strangulation is suspected. CT scans clearly demonstrate abnormalities of the bowel wall, the mesentery, the mesenteric vessels, and the peritoneum. [11, 19, 18, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29]
CT scanning should be performed with intravenous contrast enhancement. Intraluminal contrast material may not be necessary, because fluid and gas accumulation in the bowel may provide sufficient contrast; however, oral administration of a 1-2% barium sulfate suspension or a 2% water-soluble contrast agent 30-120 minutes before scanning may be useful for accurately locating the site and degree of obstruction. [20, 7]
The diagnosis of obstruction is based on the identification of a dilated proximal loop and a collapsed distal loop of small bowel (see the images below).
 A nonenhanced CT scan at the level of the umbilicus in a 67-year-old man who presented with features of small-bowel obstruction. The scan shows dilated loops of fluid-filled small bowel, with a small amount of air. Note the collapsed right colon and beak-shaped transition of the small bowel (arrow).
A nonenhanced CT scan at the level of the umbilicus in a 67-year-old man who presented with features of small-bowel obstruction. The scan shows dilated loops of fluid-filled small bowel, with a small amount of air. Note the collapsed right colon and beak-shaped transition of the small bowel (arrow).
 Enhanced axial CT scan of the mid abdomen in a 67-year-old woman. The scan shows a dilated loop of small bowel with a beak-shaped cutoff.
Enhanced axial CT scan of the mid abdomen in a 67-year-old woman. The scan shows a dilated loop of small bowel with a beak-shaped cutoff.
A bowel diameter in excess of 2.5 cm is regarded as abnormal, but this criterion is insufficient to differentiate mechanical obstruction from an adynamic ileus.
The small-bowel feces sign is an uncommon but reliable sign of a mechanical obstruction if it is seen in conjunction with bowel dilatation (cystic fibrosis, infectious and metabolic enteropathies, and reflux through the ileocecal valve can result in this finding in nondilated bowel). The feces sign occurs when feces and gas intermingle and are observed proximal to the obstruction. [30]
The feces sign is most helpful in identifying the site of obstruction, which will usually be just distal to the area of feculent-appearing material. [30] Some reports suggest that the sign is associated with low-grade obstructions, which usually do not require surgical intervention; however, one report suggests that it may be be associated with higher-grade obstructions and bowel ischemia. [31]
The level of obstruction may be determined by identifying the transition from dilated to collapsed loops of bowel; the degree of collapse and the amount of residual content in the distal bowel beyond the obstruction are useful to note; the passage of contrast material into the distant collapsed segment indicates that the obstruction is partial or incomplete [32]
CT scans do not usually help in identifying an adhesive band. The diagnosis of adhesions is based on the abruptly changing caliber of the small-bowel lumen in the absence of radiologic evidence of another obstructive cause. Adhesions most frequently involve the terminal ileum, usually in association with the undersurface of an abdominal scar, the site of previous surgical intervention, or an inflammatory focus. [21, 8]
High-density intra-abdominal free fluid (>10 HU) on CT has been determined to be significantly associated with the need for surgical intervention in patients with adhesive small-bowel obstruction. In a study by Matsushima et al, sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of high-density intra-abdominal free fluid to predict need for surgical intervention were 83.9%, 65.3%, 75.4%, 76.2%, and 75.6 %, respectively. [33]
CT findings in a closed-loop obstruction depend on the length, the degree of distention, and the intra-abdominal orientation of the closed loop. Findings may include a U- or C-shaped loop of small bowel and a radial configuration of the mesentery, with stretched vessels converging on the site of a torsion. Tightly twisted mesentery is occasionally depicted as the whirl sign. At the site of the obstruction, collapsed loops are round, oval, or triangular. On longitudinal imaging, the beak sign appears as a fusiform tapering at the site of the obstruction. [20, 21, 28]
In a retrospective study of 148 patients with closed-loop small-bowel obstruction, increased attenuation of bowel wall and mesenteric vessels on non-contrast-enhanced CT had a specificity for bowel ischemia or necrosis of 100%, according to de Kok et al. [2]
The features of strangulation on CT scans may include evidence of small-bowel obstruction, a circumferential thickening of the bowel wall (with a high attenuation), the target sign, and congestion or hemorrhage in the mesentery attached to the closed loop. A serrated beak (see the image below) may be seen at the site of obstruction. Edema in the mesentery attached to the involved segment may result in a hazy appearance and diffuse engorgement, and the mesenteric vasculature may take an unusual course. After the intravenous administration of contrast material, the bowel wall may show delayed, poor, or no enhancement. In advanced cases, pneumatosis intestinalis may develop. [34] A large amount of ascites may be present. [21]
In determining strangulation in small bowel obstruction, Millet et al found that 2 CT findings can be particularly helpful in clinical practice: reduced bowl wall enhancement (specificity, 95%) and the absence of mesenteric fluid (sensitivity, 89%). In addition, bowel wall thickness had a sensitivity of 48% and a specificity of 83%). [29]
In a retrospective analysis of 164 unenhanced and contrast-enhanced CT studies from 158 consecutive patients with mechanical small-bowel enhancement, adding unenhanced CT to contrast-enhanced CT improved the sensitivity, diagnostic confidence, and interobserver agreement of the diagnosis of ischemia, a complication of mechanical small-bowel obstruction, on the basis of decreased bowel wall enhancement. [27]
 Enhanced axial CT scan of the mid abdomen in a 67-year-old woman. The scan shows a dilated loop of small bowel with a beak-shaped cutoff.
Enhanced axial CT scan of the mid abdomen in a 67-year-old woman. The scan shows a dilated loop of small bowel with a beak-shaped cutoff.
The CT findings of malrotation include the distribution of the small bowel to the right side of the abdomen and of the colon to the left side of it. Abnormal orientation of the superior mesenteric vessels and aplasia of the uncinate process of the pancreas may be seen. If a volvulus occurs, its radiologic appearance is similar to that of any closed-loop obstruction. [21, 35]
CT scanning is useful in the diagnosis of external hernia at unusual sites, particularly in patients with obesity. The technique can demonstrate visceral hernial contents and complications such as vascular compromise. The diagnosis of an internal hernia is always based on radiologic findings, and CT scanning is useful in depicting the precise site, type, and contents of the hernia. [19, 21]
The CT features of a paraduodenal hernia include the following:
-
A cluster of small bowel anterior and lateral to the pancreas
-
A saclike mass of small-bowel loops
-
Encapsulation of the small-bowel loops
-
A mass effect on the posterior wall of the stomach
-
Caudal displacement of the duodenojejunal junction
-
Stretching and/or engorgement of the mesenteric vessels, which may be displaced to the left or right of the aorta or the inferior vena cava, respectively
Less common CT findings include an established small-bowel obstruction, caudal or dorsal displacement of the transverse colon, and medial displacement of the ascending or descending colon. Similar features may be seen with the uncommon transmesenteric hernia, together with the additional finding of a deficiency in the omental fat overlying the herniated small bowel.
Any of the less-common causes of small-bowel obstruction can be demonstrated on CT scans, and many of them have specific radiologic features. In patients with Crohn disease, narrowing of the small-bowel lumen and mural thickening (see the image below) are well depicted. In the acute phase, the small bowel shows mural stratification, and, often, it has a target-like or double-halo appearance. With intravenous contrast enhancement, inflamed mucosa and serosa show marked enhancement, and the intensity of enhancement is correlated with the activity of disease. In chronic disease, mural stratification disappears and the diseased bowel has a typically uniform attenuation. Fat deposition in the bowel wall indicates inactive disease. [21]
 An enhanced axial CT scan at the level of the right iliac fossa in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows transmural thickening of the terminal ileum associated with mucosal irregularity.
An enhanced axial CT scan at the level of the right iliac fossa in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows transmural thickening of the terminal ileum associated with mucosal irregularity.
On CT scans, the appearance of intussusception (see the image below) depends on the severity and duration of the condition. On cross-sectional imaging, the intussusception may appear as a target, with alternating layers of low and high attenuation, or it may be seen as a sausage-shaped or reniform mass. [21, 36]
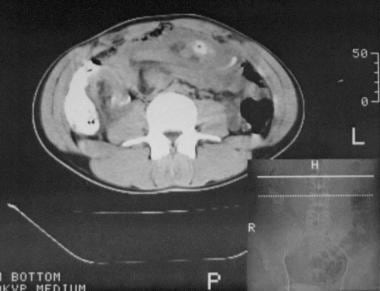 A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
When small-bowel obstruction is secondary to bowel adhering to an inflamed mass in appendicitis or diverticular disease, the CT findings may help in making the diagnosis. CT scans can demonstrate appendicitis and its complications, such as an inflammatory mass, abscess, or peritonitis. In diverticular disease, mural thickening may be demonstrated clearly together with edema of the mesentery and the complications of paracolic and pelvic abscess and peritonitis. [21]
In radiation enteropathy, CT scans demonstrate the features of small-bowel obstruction, as well as the abnormalities of an irradiated segment of small bowel, which, in most instances, lies within the pelvis. Mural thickening, luminal narrowing, and mesenteric fibrosis occur. [21]
In intestinal tuberculosis, CT scans may demonstrate only slight asymmetric mural thickening if the inflammation is mild; however, with gross disease, the bowel wall is thickened and an inflammatory mass is demonstrated. This mass has a heterogeneous appearance. Large regional lymph nodes with low-attenuation centers may also be demonstrated. [21]
In gallstone ileus (see the image below), CT scans may demonstrate the gallstone and gas within the shrunken gallbladder or biliary tree, in addition to small-bowel obstruction. [17]
 An enhanced axial CT scan at the level of the pelvic brim in a 67-year-old woman. The scan shows a gallstone obstructing the small bowel.
An enhanced axial CT scan at the level of the pelvic brim in a 67-year-old woman. The scan shows a gallstone obstructing the small bowel.
The CT appearance of an intramural hematoma is nonspecific and depends on the age of the hematoma. Soon after hemorrhage occurs, the attenuation is low; however, as time passes, its attenuation increases. Once lysis of the clot begins, the attenuation again decreases. It may also be centripetal, which gives rise to the ring sign, with a crescent of high attenuation. [21]
If a bezoar is the cause of small-bowel obstruction, CT scanning may demonstrate the bezoar as a mass in the obstructed segment of bowel. The bezoar may be outlined by fluid in the proximally dilated small bowel, and the mass may be mottled as a result of air trapped within it. [21, 37]
Malignancy involving the small bowel may have a variety of CT appearances. Although rare, adenocarcinoma may be seen, particularly in the duodenum and proximal jejunum. The tumor is usually detected only at an advanced stage, and in patients with small-bowel obstruction, the mass may be seen as mural thickening with luminal compromise in a transitional zone between dilated and collapsed bowel. [21]
Primary non-Hodgkin small-bowel lymphoma rarely causes obstruction; however, nodal lymphoma may arise in the mesentery and invade the small bowel by means of direct infiltration to cause small-bowel obstruction. A mesenteric mass invading, kinking, or compressing the small bowel may be seen on CT scans. [21]
Small-bowel obstruction is a major complication of a carcinoid tumor, one largely caused by the desmoplastic reaction (see the image below) that may occur in the mesentery; therefore, mural thickening and retraction of bowel loops around a segment of mesentery may occur. Metastatic nodular masses may be present. [21]
 A CT scan of a 36-year-old woman with Gardner syndrome presented with features of small-bowel obstruction. The axial contrast-enhanced CT scan through the midabdomen shows an extrinsic mass compressing a loop of small bowel. At laparotomy, a desmoid tumor of the mesentery was found; this caused the small-bowel obstruction.
A CT scan of a 36-year-old woman with Gardner syndrome presented with features of small-bowel obstruction. The axial contrast-enhanced CT scan through the midabdomen shows an extrinsic mass compressing a loop of small bowel. At laparotomy, a desmoid tumor of the mesentery was found; this caused the small-bowel obstruction.
Peritoneal carcinomatosis may be recognized by the demonstration of omental masses kinking or compromising the small bowel, thereby resulting in small-bowel obstruction. [21]
In all malignant tumors causing small-bowel obstruction, CT scans are useful in depicting local extent of the disease and the presence of distant metastases (when appropriate).
With the advent of multisection CT, CT angiography may provide a future alternative to angiography for assessing intestinal ischemia.
In one study of 44 patients, increased bowel-wall attenuation on unenhanced 64-section multidetector CT images was found to be a specific sign for ischemia complicating small-bowel obstruction. [38]
Degree of confidence
The reported sensitivity of CT scanning for detecting small-bowel obstruction is 78-100% in high-grade or complete obstruction. If the obstruction is partial or intermittent, the accuracy is low. [20, 21, 39]
CT can be helpful in excluding closed-loop small-bowel obstruction, according to Makar et al. In their study, sensitivity and specificity of MDCT for closed-loop small-bowel obstruction were 53% and 83%, respectively. [28]
If the entire small bowel is distended, a barium enema study should be performed to exclude a large-bowel obstruction and a patent ileocecal valve. A distended loop of small bowel may migrate from its expected anatomic location; therefore, determining the site of obstruction on the basis of a transitional zone alone may be misleading.
Carcinoid tumors, intestinal tuberculosis, and desmoid tumors all may have CT features similar to those of peritoneal carcinomatosis. Although the presence of ascites suggests a strangulated obstruction, intra-abdominal fluid may occur in less complicated forms of obstruction. Feces in the small bowel can mimic the mottled appearance of a bezoar if stasis above a complete blockage is severe. [21]
Magnetic Resonance Imaging
Although MRI does have a role in imaging of the small bowel, the plethora of contrast media and techniques available indicates that its role is not yet fully established and further clinical trials are required. The technique has been used to evaluate chronic mesenteric ischemia. The results of animal studies suggest that a lack of enhancement after the intravenous injection of contrast material may be a useful early sign of acute ischemia. [40, 41, 42]
Because MRI can be used to demonstrate vessels, quantitate blood flow, assess oxygenation, and depict associated morphologic changes, it may become the modality of choice in detecting acute ischemia in the future. MRI will therefore have a role in the assessment of small-bowel obstruction associated with strangulation. Small-bowel obstruction has been diagnosed by using T1-weighted MRI sequences combined with antiperistaltic agents and retrograde insufflation. Subsecond RARE imaging (rapid acquisition with relaxation enhancement) may produce similar results. [11, 35, 40]
Clinical experience with MRI in the diagnosis of acute small-bowel disease is limited, and its use in this capacity depends on the availability of suitable equipment.
Ultrasonography
Ultrasonography may demonstrate the features and causes of small-bowel obstruction, and it is of particular value in looking at the dynamics of the small bowel (see the images below). [11] In patients with small-bowel obstruction, ultrasonography may clearly demonstrate loops of distended bowel. The loops have a rounded contour and are not deformed by the pressure of adjacent bowel loops. The loss of definition and prominence of the valvulae conniventes are demonstrated. US can help accurately predict the level of small-bowel obstruction by helping locate the dilated loops and analyze the fold patterns.
 A sonogram of the right iliac fossa in a 2-year-old child presenting with abdominal pain that shows a bowel mass demonstrated as the pseudokidney sign.
A sonogram of the right iliac fossa in a 2-year-old child presenting with abdominal pain that shows a bowel mass demonstrated as the pseudokidney sign.
 Abdominal sonogram in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The sonogram shows a complex mass of concentric rings of alternating hypoechoic and hyperechoic layers surrounding a highly reflective center. The mass was located in the epigastrium.
Abdominal sonogram in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The sonogram shows a complex mass of concentric rings of alternating hypoechoic and hyperechoic layers surrounding a highly reflective center. The mass was located in the epigastrium.
Unlike other radiologic techniques, ultrasonography may be used to assess peristalsis. Close to the site of an obstruction, the distended bowel loses its muscular activity; more proximally, the peristaltic activity may be marked in cases of acute obstruction. These features help differentiate a mechanical obstruction from the adynamic ileus of the postoperative state or peritonitis.
Occasionally, the cause of a small-bowel obstruction can be identified directly. Gallstones, foreign bodies, and mural thickening from inflammatory or neoplastic disease may be revealed. A bezoar may appear as an echogenic intraluminal mass. If a bezoar contains air or is surrounded by fluid, it may cast an acoustic shadow.
The sonographic appearance of intussusception is specific; a target, atypical target, or doughnut appearance on the transverse section of the bowel may be seen as a complex mass of concentric rings of alternating hypoechoic and hyperechoic layers surrounding a highly reflective center. The head of the intussusception may be visible within a dilated loop of small bowel, and left-right inversion of the superior mesenteric vessels may be evident. The presence of free peritoneal fluid is a less specific sonographic finding. Certain sonographic appearances have been proposed as predictors of the irreducibility of an intussusception. These appearances include a large amount of fluid within the intussusceptum and the presence of a doughnut-like appearance with a thick, echo-poor rim.
Color-flow Doppler images depict the viability of the bowel; therefore, the absence of flow suggests necrosis. This finding has been linked to the success rate of hydrostatic intussusception reduction. When blood flow is present, the success rate is in excess of 90%, but the rate decreases to only 30% when no blood flow is demonstrated.
The sonographic diagnosis of midgut malrotation is based on the inversion of the relationship of the superior mesenteric artery and vein; however, this finding is not sensitive or specific for this diagnosis. A hyperpulsatile superior mesenteric artery and a thickened and highly reflective small-bowel wall suggest volvulus.
With gallstone ileus, the classic triad of a calcified gallstone in an ectopic position, gas in the biliary tree, and small-bowel obstruction may be demonstrated.
Regarding intestinal ascariasis, individual worms may appear as hypoechoic longitudinal tubular structures with echogenic walls. If the alimentary tract of the worm is empty, the worm may appear as an echogenic line. If its alimentary tract is distended, the worm can appear as parallel hypoechoic bands. On transverse sections, the worm appears as a target sign with an echogenic body wall and a central dot representing its gut. Prolonged scanning may demonstrate movement of the worm. A tangle of worms mixed with feces and gas may appear as a complex intraluminal mass.
With a small-bowel lymphoma, eccentric mural thickening by lymphomatous infiltrate and aneurysmal dilatation of the bowel lumen and mesenteric lymphadenopathy may produce a so-called sandwich sign; this distinguishes lymphoma from Crohn disease. A lymphomatous infiltrate is usually anechoic, but hemorrhage and clotting may give rise to echogenic areas. Anechoic deposits may mimic duplication cysts. [35]
In patients with jejunoileal atresia and meconium ileus, sonography may demonstrate dilated loops of bowel containing gas and fluid proximal to an atretic segment. Peristalsis may be reduced or increased. In meconium ileus, multiple loops of bowel are filled with highly echogenic material. [35]
According to Rosano et al, a complete ultrasound abdominal examination should be performed to rule out other pathologies, with assessment of the intestinal loops being performed via the global view technique, in which the intestine is examined from the bottom upward and with vertical movement of the probe starting from the right iliac fossa, followed by horizontal movements from the right side to the left side. [9]
Degree of confidence
Ultraonography is able to depict small-bowel obstruction well because intraluminal fluid is a natural contrast medium. Numerous studies have shown the value and effectiveness of US in the diagnosis of small-bowel obstruction, but its exact sensitivity remains uncertain. In patients with intussusception, the sensitivity is 95-100%, with a positive predictive value of 100%. Because sonographic findings in patients with malrotation are nonspecific, barium examination remains the preferred study in patients in whom malrotation is suspected. [18]
When intraluminal air is associated with small-bowel obstruction, the air may obscure the ultrasonographer's field of view; however, by paying attention to detail and using graded compression, an examination of all regions of the abdomen is possible. Scanning in the coronal plane through the flank may also be of value. The variation that may occur in peristalsis in patients with small-bowel obstruction may cause confusion. Occasionally, differentiating an ileus from an obstruction is difficult, particularly if peristalsis is reduced or absent in the bowel immediately proximal to an obstruction.
Fluid trapped within an intussuscepted mesentery can mimic duplication cysts or hematomas. The target appearance of small bowel referred to above is not specific and may occur in a multitude of inflammatory and neoplastic disorders. Vessel inversion can be found in patients with normal gut anatomy, and documented malrotations have occurred with normally related superior mesenteric vessels.
Nuclear Imaging
Radionuclide scanning has no specific role in the diagnosis of small-bowel obstruction, with an exception for white blood cell scanning for the detection and localization of intra-abdominal inflammatory disease that may result in obstruction (see the image below). Scanning for technetium-99m hexamethylpropyleneamine oxime (99mTc HMPOA) uptake is useful for demonstrating disease activity in patients with Crohn disease. [11] Technetium-99m HMPOA granuloscintigraphy has been shown to have a sensitivity of 79% and a specificity of 98% for small-bowel obstruction. Tc-99m HMPOA uptake is not specific for Crohn disease, and activity may be observed with other causes of inflammation or infection.
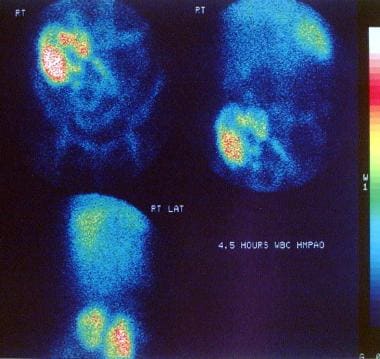 Technetium-99m hexamethylpropyleneamine oxime (99mTc HMPAO)–labeled white blood cell scan in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows active uptake of the radionuclide in the terminal ileum and the cecum/ascending colon indicative of an active inflammatory process. The patient was treated for active Crohn disease.
Technetium-99m hexamethylpropyleneamine oxime (99mTc HMPAO)–labeled white blood cell scan in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows active uptake of the radionuclide in the terminal ileum and the cecum/ascending colon indicative of an active inflammatory process. The patient was treated for active Crohn disease.
Angiography
Superior mesenteric angiography has been used in the diagnosis of internal herniation, intussusception, volvulus, malrotation, and adhesions. Findings are of particular importance when vascular compromise is associated.
Although angiography is a sensitive method for demonstrating vascular occlusion, it is invasive, and its role is limited in patients who are ill, particularly because alternative and less invasive techniques are available. Color Doppler imaging and CT angiography may provide the same information by alternative means.
-
Plain abdominal radiograph in a 6-year-old boy who presented with vomiting and acute pain in the right iliac fossa. The loops of the small bowel are dilated, and small calcific nodules are seen in the right iliac fossa. These findings are suggestive of appendicoliths. At laparotomy, an appendiceal mass was found; this had caused the small-bowel obstruction.
-
Plain abdominal radiograph in a 9-year-old patient with a past history of appendicitis complicated by peritonitis who presented with abdominal pain and vomiting. The clinical diagnosis was small-bowel obstruction resulting from adhesions. This radiograph shows markedly distended loops of small bowel, with effacement of the valvulae in the mid abdomen. The child recovered with conservative treatment.
-
Lateral decubitus radiograph of a newborn who presented with features of bowel obstruction. The radiograph shows markedly distended loops of small bowel.
-
Plain abdominal radiograph of the abdomen in a newborn after 10 days of conservative treatment (same patient as in the previous image). The radiograph shows only mild dilatation of the loops of the small bowel. Note the fine grainy calcification in the right iliac fossa. Meconium peritonitis (arrow), caused by the small-bowel obstruction, was diagnosed.
-
An erect plain abdominal radiograph in a 4-year-old patient from a region in which roundworms are known to be endemic. The radiograph shows multiple dilated loops of small bowel, with air-fluid levels and tangled roundworms (arrow).
-
This plain abdominal radiograph of a 55-year-old woman presenting with features of intestinal obstruction shows dilated loops of the small bowel associated with thickened edematous valvulae conniventes and a strangulated left inguinal hernia (arrow).
-
Plain abdominal radiograph of the abdomen in a 72-year-old man with a history of intermittent abdominal pain over several years that settled spontaneously. On this occasion, his pain was severe. The abdominal radiograph shows dilated loops of small bowel, but the concentration of several loops of small bowel in the right hypochondrium should be noted as this finding is suggestive of malrotation. At surgery, a midgut volvulus caused by malrotation was found. The patient's age is unusual for those presenting with a midgut volvulus.
-
An upper GI barium series in a 32-year-old man with a history of intermittent small-bowel volvulus that lasted several years and settled spontaneously. The barium study shows the jejunal loops in the right hypochondrium; this finding is suggestive of bowel malrotation.
-
An erect plain abdominal radiograph of the abdomen in a 72-year-old woman that shows markedly distended jejunal loops with air-fluid levels. The air overlying the liver and a large laminated gallstone in the right iliac fossa (arrow) should be noted. The features are those of a gallstone ileus.
-
Plain abdominal radiograph of the abdomen in a 52-year-old woman presenting with features of small-bowel obstruction. At laparotomy, a cecal volvulus was found to be the cause of the obstruction. Note that the cecum occupies the middle of the abdomen and that the cecal pole is directed laterally.
-
A plain abdominal radiograph of the abdomen in a 36-year-old man shows features of mid small-bowel obstruction caused by a paraumbilical hernia (arrow).
-
An upper GI barium study performed through a nasogastric tube in a patient with clinical features of bowel obstruction but a gasless abdomen on plain abdominal radiograph. The barium study shows a fistulous communication between the gallbladder fossa and the duodenum and marked dilatation of the jejunum associated with stretched mucosal folds. At laparotomy, a gallstone ileus was confirmed.
-
Erect plain abdominal radiograph of the abdomen in a 69-year-old woman presenting with features of small-bowel obstruction. Radiograph shows air in the biliary tree, a string-of-beads sign (arrows), and a faint opacity in the right lower pelvis suggestive of a gallstone (not depicted well).
-
An upper GI barium series performed via a nasogastric tube in a 69-year-old woman presenting with features of small-bowel obstruction showing reflux of barium into the biliary tree and the gallbladder fossa (same patient as in the previous image). Note the mild dilatation of the duodenum.
-
Follow-up barium study in the small bowel of a 69-year-old woman presenting with features of small-bowel obstruction (same patient as in the previous 2 images) showing obstruction caused by a large laminated gallstone (arrow).
-
Water-soluble contrast upper GI examination in a patient with clinical features of small-bowel obstruction and a history of surgery for large bowel cancer. The contrast-enhanced study shows dilated loops of small bowel, with stretching of the mucosal folds and a narrowed segment ending in a beak (arrow). At surgery, a small-bowel obstruction from extrinsic compression was found to be the result of mesenteric metastases.
-
Plain abdominal radiograph of the abdomen in a 53-year-old woman with Crohn disease who presented with features of small-bowel obstruction. The radiograph shows a long stricture of the terminal ileum.
-
Upper GI barium series in a patient with features of intermittent small-bowel obstruction. Multiple strictures and polypoid filling defects are noted in the proximal small bowel caused by deposits of non-Hodgkin lymphoma.
-
Plain abdominal radiograph of the abdomen in a 47-year-old man presenting with features of small-bowel obstruction. The radiograph shows markedly dilated loops of small bowel in the central and upper abdomen, with little air seen in the colon.
-
An erect plain abdominal radiograph in a 47-year-old man presenting with features of small-bowel obstruction. The image shows multiple fluid levels in the small bowel (same patient as in the previous image).
-
Postevacuation image from part of a double-contrast barium enema study in a 47-year-old man presenting with features of small-bowel obstruction. The image shows a coiled-spring appearance in the region of the cecum suggestive of an intussusception (same patient as in the previous 2 images). At laparotomy, an ileocecal intussusception was found in association with a carcinoid tumor of the terminal ileum.
-
An erect abdominal image obtained as part of a double-contrast barium enema study shows multiple fluid levels in the centrally placed small bowel.
-
A radiograph of the terminal ileum showing a stricture and shouldering of the terminal ileum caused by an adenocarcinoma (same patient as in the previous image).
-
A supine abdominal radiograph in a 57-year-old man presenting with colicky abdominal pain and vomiting that shows multiple dilated loops of small bowel in the central abdomen and a possible mass in the right hypochondrium.
-
Postevacuation image from part of a barium enema study in a 57-year-old man presenting with colicky abdominal pain and vomiting. The image shows a coiled-spring appearance at the hepatic flexure of the colon typical of an intussusception. At laparotomy, an ileocolic intussusception was found; this was secondary to a carcinoid tumor of the terminal ileum.
-
A sonogram of the right iliac fossa in a 2-year-old child presenting with abdominal pain that shows a bowel mass demonstrated as the pseudokidney sign.
-
Part of a barium enema study in a 2-year-old child presenting with abdominal pain showing a polypoid filling defect within the ascending colon. The filling defect was constant on all images. At laparotomy, a chronic ileocolic intussusception was found.
-
Abdominal sonogram in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The sonogram shows a complex mass of concentric rings of alternating hypoechoic and hyperechoic layers surrounding a highly reflective center. The mass was located in the epigastrium.
-
A nonenhanced CT scan of the abdomen in a 16-year-old male adolescent with cystic fibrosis who presented with intermittent colicky epigastric pain of 6 weeks' duration. The scan shows a complex mass of concentric rings of alternating low- and high-attenuating layers surrounding a very high attenuation center caused by intraluminal Gastrografin. At laparotomy, a chronic jejunojejunal intussusception was found.
-
A CT scan of a 36-year-old woman with Gardner syndrome presented with features of small-bowel obstruction. The axial contrast-enhanced CT scan through the midabdomen shows an extrinsic mass compressing a loop of small bowel. At laparotomy, a desmoid tumor of the mesentery was found; this caused the small-bowel obstruction.
-
A supine abdominal radiograph of a 47-year-old man who presented with intermittent abdominal pain and weight loss of 3 months' duration. The radiograph shows mildly dilated loops of small bowel. Note the air in the transverse colon; this can be traced to the rectum.
-
A contrast-enhanced axial CT scan through the midabdomen showing a marked mural thickening associated with mucosal irregularity at the hepatic flexure of the colon. At laparotomy, a carcinoma was found; this involved the ascending colon and hepatic flexure.
-
A plain abdominal radiograph of a 67-year-old man who presented with features of small-bowel obstruction. The radiograph demonstrates gasless findings.
-
A nonenhanced CT scan at the level of the umbilicus in a 67-year-old man who presented with features of small-bowel obstruction. The scan shows dilated loops of fluid-filled small bowel, with a small amount of air. Note the collapsed right colon and beak-shaped transition of the small bowel (arrow).
-
A nonenhanced transaxial CT scan at the level of the umbilicus in a 67-year-old man who presented with features of small-bowel obstruction. The scan shows a dilated loop of air-fluid–filled small bowel leading into an incarcerated umbilical hernia.
-
Enhanced axial CT scan of the mid abdomen in a 67-year-old woman. The scan shows a dilated loop of small bowel with a beak-shaped cutoff.
-
An enhanced axial CT scan at the level of the pelvic brim in a 67-year-old woman. The scan shows a gallstone obstructing the small bowel.
-
A Barium follow-through study in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction that shows mucosal edema and stricturing of the terminal ileum and the cecum.
-
An enhanced axial CT scan at the level of the right iliac fossa in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows transmural thickening of the terminal ileum associated with mucosal irregularity.
-
Technetium-99m hexamethylpropyleneamine oxime (99mTc HMPAO)–labeled white blood cell scan in a 63-year-old woman who presented with features of recurrent attacks of small-bowel obstruction. The scan shows active uptake of the radionuclide in the terminal ileum and the cecum/ascending colon indicative of an active inflammatory process. The patient was treated for active Crohn disease.
-
This abdominal radiograph (left) shows a dilated loop of small bowel in the mid abdomen (hollow arrow). There is a soft tissue density overlying the left pubic bone, with a vague air density suggestive of an inguinal hernia. An axial CT scan confirms the presence of fat density within the scrotum. At surgery, a nonstrangulated small-bowel loop was released from the left inguinal canal.











