Practice Essentials
Systemic sclerosis is a multisystem disease of connective tissue that is accompanied by vasculopathy. Scleroderma, its original name, means hard skin. Progressive systemic sclerosis (PSS) is a connective tissue disease associated with small vessel arterial vasculopathy and inflammatory and immunologic processes. The peak incidence is between 45 and 64 years of age. [1, 2] Clinically, PSS is classified as diffuse or limited depending on the distribution of skin disease. PSS is considered limited when involvement is restricted to the distal extremities and face. The limited form is associated with a lower risk of visceral involvement, although pulmonary hypertension is more common. [3, 4, 5, 6]
Interstitial lung disease (ILD) is the leading cause of mortality in patients with systemic sclerosis. High-resolution CT is recommended in all patients with the disease. [7, 8, 9, 10, 11] Risk stratification by measuring the extent of disease on HRCT of the chest, by longitudinal decline in pulmonary function tests (PFTs), and by mortality prediction models help identify significant interstitial lung disease. [12, 13]
(See the images below.)
 Posteroanterior chest radiograph reveals irregular reticular opacities in the lower lobes. Two years later, the findings are more marked.
Posteroanterior chest radiograph reveals irregular reticular opacities in the lower lobes. Two years later, the findings are more marked.
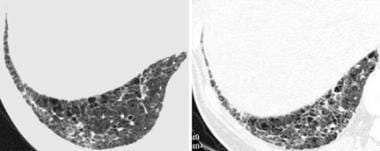
 High-resolution CT of biopsy-proven nonspecific interstitial pneumonia. The image shows abnormal reticular opacities in a background of ground-glass opacity, with associated traction bronchiectasis indicating lung fibrosis.
High-resolution CT of biopsy-proven nonspecific interstitial pneumonia. The image shows abnormal reticular opacities in a background of ground-glass opacity, with associated traction bronchiectasis indicating lung fibrosis.
Diffuse cutaneous systemic sclerosis (dcSSc) and limited cutaneous systemic sclerosis (lcSSc) scleroderma overlap the following syndromes [14] :
-
CREST syndrome (calcinosis, Raynaud phenomenon, esophageal dysmotility, skin pigmentation, telangiectasias)
-
Mixed connective tissue disease (controversial whether this is a separate entity or an intermediate stage in the progression to connective tissue disease)
-
Scleromyositis (coexisting features of dermatomyositis without features of systemic lupus erythematosus)
-
Polymyositis synthetase (interstitial lung disease, myositis, Raynaud phenomenon, arthritis)
-
Morphea (focal cutaneous scleroderma)
Imaging modalities
Chest radiography is insensitive, since findings are abnormal in only two thirds of patients with pulmonary disease.
High-resolution computed tomography (HRCT) scanning is the best imaging test for assessing the extent and severity of pulmonary disease. Reported detection of fibrosis with HRCT is 60-90%, compared with 60-100% at autopsy. [15, 16, 17, 18, 19, 1, 20, 21] HRCT findings are abnormal in most patients with functional impairment. False-negative HRCT imaging study findings have occurred in the setting of alveolitis using bronchoalveolar lavage in patients with normal pulmonary function tests. [22]
Echocardiographic measurements of systolic pulmonary arterial pressure correlate well with right heart catheterization values. [23] Early detection of cardiac and renal involvement even in asymptomatic patients is recommended to avoid further complications. Cardiac magnetic resonance imaging has been found to identify markers for vacular and fibrotic damage. [24]
Echocardiography is the most frequently used modality for pulmonary artery hypertension, which is present in 10-15% of patients with systemic sclerosis. The specificity and sensitiviy of echocardiography are 75% and 90%, respectively. [8]
High-resolution ultrasound imaging of skin involvement may be helpful to quantitatively evaluate dermal thickness in systemic sclerosis. [9, 25, 26] In some studies, lung ultrasonography has been identified as a noninvasive, radiation-free technique for the diagnosis of interstitial lung disease with both high sensitivity and high specificity. [27, 28, 29]
Radiographs in women who are pregnant are limited to a single PA view to minimize radiation exposure. Shielding is used when appropriate. If HRCT examination is considered essential during pregnancy, it can be tailored to minimize radiation exposure.
Intervention
A collaborative approach between pulmonologists and thoracic radiologists is important in the diagnosis and management of interstitial lung disease. Analysis of HRCT images of the chest can guide video-assisted thoracoscopic lung biopsy. An increased incidence of lung cancer is seen in patients with scleroderma, and the radiologist is involved in detection and diagnosis through CT-guided percutaneous lung biopsy.
Perform percutaneous drainage of complicated parapneumonic effusions and empyemas with CT or ultrasonographic guidance.
Radiography
Early radiographic findings include subpleural reticular or reticulonodular opacity in a basal predominant distribution.
Late radiographic findings include the following:
-
Fibrotic changes involving the lower two thirds of the lung, with associated volume loss and honeycombing
-
Pulmonary artery enlargement and cardiomegaly
Ancillary findings include diffuse esophageal dilation with a resultant "air esophagram sign," which is useful when present to differentiate progressive systemic sclerosis (PSS) from idiopathic pulmonary fibrosis (IPF), asbestosis, and rheumatoid arthritis.
(See the image below.)
 Posteroanterior chest radiograph reveals irregular reticular opacities in the lower lobes. Two years later, the findings are more marked.
Posteroanterior chest radiograph reveals irregular reticular opacities in the lower lobes. Two years later, the findings are more marked.
Chest radiography is relatively insensitive in early disease, and findings may be minimal even in advanced disease; however, chest radiographic findings are observed in as many as two thirds of symptomatic patients, with findings suggestive of fibrosis demonstrated in 25-45% of patients.
(See the image below.)
 Posteroanterior and lateral chest radiographs reveal hazy opacity in both bases, with elevation of diaphragms suggestive of restrictive lung disease.
Posteroanterior and lateral chest radiographs reveal hazy opacity in both bases, with elevation of diaphragms suggestive of restrictive lung disease.
Interstitial lung disease with a predominant lower lobe distribution on chest radiography may have numerous etiologies, including PSS. Clinical history and esophageal dilation on radiographs suggest PSS. Any phase of IPF, asbestosis, interstitial pulmonary edema, lymphangitic metastases, pulmonary hemorrhage, and other diffuse lung diseases may mimic PSS on chest radiographs. On the posteroanterior (PA) view, the breast shadows can mimic increased markings over the lower lung zones. Lateral view is critical so as to obtain a less obscured view of the lower lobes.
Computed Tomography
Patients with suggested or known diagnosis of PSS should undergo the following examinations [30] :
-
Standard resolution CT (SRCT) to exclude a lung neoplasm (which is slightly more common than in the general population) and to evaluate pleuropericardial, esophageal, cardiac, and pulmonary arterial abnormalities
-
HRCT to evaluate lung parenchymal involvement
Interstitial lung disease (ILD) is the leading cause of mortality in patients with systemic sclerosis. High-resolution CT is recommended in all patients with the disease. [7, 8, 9, 10, 11]
Imaging findings
Pulmonary fibrosis and pulmonary hypertension are the most common findings. Overlap syndromes or CREST syndrome are suggested when pulmonary hypertension is out of proportion to the degree of fibrosis.
HRCT findings of pulmonary fibrosis include the following:
-
Architectural distortion
-
Subpleural cysts or honeycombing
-
Interlobular septal thickening
-
Visceral pleural thickening
-
Parenchymal micronodules
Ground-glass opacity may indicate acute inflammation (alveolitis). Honeycombing (demonstrated in the image below) favors a histologic usual interstitial pneumonitis (UIP) pattern.
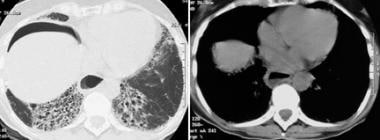 High-resolution CT demonstrates extensive basal honeycombing suggestive of lung fibrosis. Note the extraluminal peritoneal cavity air presumed to be secondary to benign pneumatosis intestinalis and the dilated esophagus with an air-fluid level.
High-resolution CT demonstrates extensive basal honeycombing suggestive of lung fibrosis. Note the extraluminal peritoneal cavity air presumed to be secondary to benign pneumatosis intestinalis and the dilated esophagus with an air-fluid level.
Mixed reticulation and ground-glass opacity with little or absent honeycombing favor histologic nonspecific interstitial pneumonia (NSIP).
Distribution of disease
Fibrosis is subpleural and basal predominant.
A less marked involvement of the upper lobes favors PSS or other collagen vascular disease as the etiologic cause of the UIP pattern, rather than IPF or chronic hypersensitivity pneumonitis.
HRCT identified fibrotic interstitial lung disease (ILD) in 16 of 43 patients with systemic sclerosis. The main pattern of ILD was identified with nonspecific interstitial pneumonia (NSIP). [20]
Ancillary findings
Mediastinal adenopathy is found; the prevalence is increased in more extensive lung disease. Esophageal dilation is present on CT scans in 80% of patients with diffuse lung disease resulting from PSS.
Degree of confidence
Studies have shown that HRCT is diagnostically accurate in specific subsets of patients with diffuse lung disease. In a study of 85 patients with diffuse lung disease by Swensen et al, [31] radiologists more frequently had a high level of confidence in diagnosing UIP than any other pattern and listed it as the number one diagnosis in 89% of patients with that histologic finding. Imaging diagnoses were most accurate (90% correct) when a high level of confidence was present.
Remy-Jardin and colleagues correlated HRCT findings with functional parameters and bronchoalveolar lavage (BAL) results in patients with PSS. [22] BAL findings were abnormal in 7 of 21 patients with normal imaging and PFTs, suggesting that it is more sensitive than HRCT in detecting subclinical alveolitis. The extent of parenchymal destruction, which correlated with functional abnormality, was better depicted by HRCT.
Diot and colleagues assigned point values to each abnormal finding present on HRCT of 52 patients with progressive systemic sclerosis (PSS). Total scores were inversely proportional to total lung capacity and diffusing capacity for carbon monoxide (DLCO). Receiver operator curve analysis demonstrated that an HRCT score of 7 or greater minimized false negatives (sensitivity of 0.60) while achieving a specificity of 0.83. The positive predictive value of HRCT in this study was 0.82. [15]
False negatives have been documented in patients with subclinical alveolitis. [22]
-
Posteroanterior chest radiograph reveals irregular reticular opacities in the lower lobes. Two years later, the findings are more marked.
-
High-resolution CT reveals intralobular interstitial thickening and mild traction bronchiectasis in the lung base, with progression over a 2-year period.
-
Posteroanterior and lateral chest radiographs reveal hazy opacity in both bases, with elevation of diaphragms suggestive of restrictive lung disease.
-
High-resolution CT of biopsy-proven nonspecific interstitial pneumonia. The image shows abnormal reticular opacities in a background of ground-glass opacity, with associated traction bronchiectasis indicating lung fibrosis.
-
High-resolution CT demonstrates extensive basal honeycombing suggestive of lung fibrosis. Note the extraluminal peritoneal cavity air presumed to be secondary to benign pneumatosis intestinalis and the dilated esophagus with an air-fluid level.