Practice Essentials
Hemangioblastomas are vascular tumors that can be found throughout the neuraxis, primarily in the cerebellum and spinal cord. Hemangioblastomas of the spinal cord account for approximately 3% of all intramedullary spinal tumors. [1, 2] These tumors occur more commonly as sporadic isolated lesions (70-80% of cases) rather than as multiple lesions in the cerebellum and retina as part of the dominantly inherited familial cancer syndrome, von Hippel–Lindau disease (16-25% of cases). [3] Although considered histologically benign, hemangioblastomas may cause significant neurologic deficits, depending on their location. Advances in imaging and microsurgery have markedly improved the treatment of these intraspinal lesions. [4, 5]
Although hemangioblastoma is a rare tumor of uncertain histotype that typically arises in the cerebellum, quite often in the setting of von Hippel-Lindau disease, Doyle and Fletcher described 22 cases of hemangioblastoma arising at peripheral sites. All the tumors were solitary, except 1, and arose in the spinal nerve roots (12), kidney (3), intestine (2), orbit (1), forearm (1), peritoneum (1), periadrenal soft tissue (1), and flank (1). Five patients had von Hippel-Lindau disease, and another 5 had lesions suggestive of von Hippel-Lindau disease. [6]
Preferred examination
Magnetic resonance imaging (MRI) of the spine is the diagnostic imaging examination of choice. [7, 8, 9] Advances in 3-dimensional digital subtraction angiography (3-D DSA) have made it a useful adjunct in further characterization of the vascular lesion. [10, 11, 12] Computed tomography (CT) scans of the spine generally demonstrate an isoattenuating, contrast-enhancing lesion. Decreased attenuation, which represents the associated edema, may be present around the tumor. Intraoperative ultrasonography may be a useful adjunct during surgery to help identify the location of the cyst and/or syrinx in relation to the hemangioblastoma.
(See the images below.)
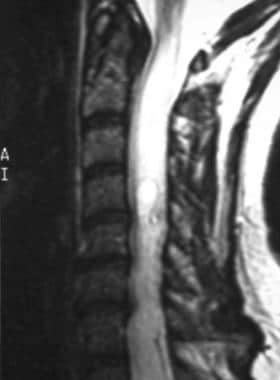
 Sagittal T1-weighted image demonstrates the dorsal location of the tumor, which enhances homogeneously. This tumor does not show any flow voids that may be seen with larger tumors. Note that the spinal cord rostral and caudal to the tumor is quite swollen from edema.
Sagittal T1-weighted image demonstrates the dorsal location of the tumor, which enhances homogeneously. This tumor does not show any flow voids that may be seen with larger tumors. Note that the spinal cord rostral and caudal to the tumor is quite swollen from edema.
 Spinal angiogram demonstrates a large cervical hemangioblastoma. Tumor blush is quite evident on this selective injection. The tumor receives a vascular supply from both the anterior and posterior spinal arteries. Embolization is not feasible for these tumors because of the small caliber of the feeding vessels. However, the angiogram is important to define the vascular anatomy for large tumors.
Spinal angiogram demonstrates a large cervical hemangioblastoma. Tumor blush is quite evident on this selective injection. The tumor receives a vascular supply from both the anterior and posterior spinal arteries. Embolization is not feasible for these tumors because of the small caliber of the feeding vessels. However, the angiogram is important to define the vascular anatomy for large tumors.
Magnetic Resonance Imaging
Because spinal hemangioblastomas are relatively rare and share some of the same imaging features with other intramedullary tumors, the diagnosis may be complicated. MRI is particularly helpful in the differential diagnosis. These tumors are almost always associated with a syrinx or significant edema. The edema that accompanies the syrinx varies; some patients have extensive swelling of the spinal cord and only a small neoplasm. Hemangioblastomas and, less often, astrocytomas have the highest proportion of syrinx formation.
Gadolinium-enhanced MRI is the primary diagnostic imaging modality for hemangioblastomas of the spine. The tumors are located mainly on the dorsal aspect of the spinal cord in the cervical and thoracic regions and appear as cystic lesions with mural nodules (see the images below). T1-weighted images show a homogeneously enhancing tumor with a rostral-caudal cyst. Serpentine signal voids on the dorsal surface of the spinal cord may be present.
 Sagittal T1-weighted image demonstrates the dorsal location of the tumor, which enhances homogeneously. This tumor does not show any flow voids that may be seen with larger tumors. Note that the spinal cord rostral and caudal to the tumor is quite swollen from edema.
Sagittal T1-weighted image demonstrates the dorsal location of the tumor, which enhances homogeneously. This tumor does not show any flow voids that may be seen with larger tumors. Note that the spinal cord rostral and caudal to the tumor is quite swollen from edema.
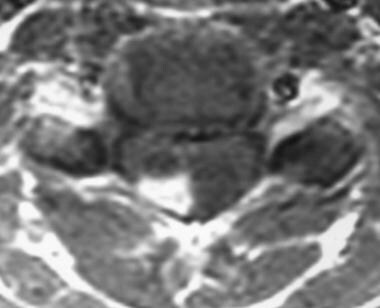 Axial T1-weighted image confirms the dorsal hemangioblastoma that abuts the pial surface, whose position is typical of these tumors and makes removal easy.
Axial T1-weighted image confirms the dorsal hemangioblastoma that abuts the pial surface, whose position is typical of these tumors and makes removal easy.
T2-weighted images more clearly demonstrate the extent of the associated edema and cyst formation (see the following image). Gadolinium-enhanced MRIs may highlight a mural nodule within the cyst wall. [13]
 T2-weighted image demonstrates the extensive edema typically associated with hemangioblastomas of the spine. This edema extends rostrally to the medulla and caudally to the upper thoracic spinal cord. If the tumor is left untreated, the edema develops into a syrinx.
T2-weighted image demonstrates the extensive edema typically associated with hemangioblastomas of the spine. This edema extends rostrally to the medulla and caudally to the upper thoracic spinal cord. If the tumor is left untreated, the edema develops into a syrinx.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD).
Angiography
Spinal angiography is indicated for large neoplasms when the diagnosis is indeterminate on MRI. [14] Angiography reveals a hypervascular, well-delineated tumor mass, as shown in the image below. No arteriovenous shunting occurs in these tumors. Angiograms clearly delineate the feeding and draining vessels; these findings may be helpful for surgical planning and tumor resection. [10, 15, 7]
 Spinal angiogram demonstrates a large cervical hemangioblastoma. Tumor blush is quite evident on this selective injection. The tumor receives a vascular supply from both the anterior and posterior spinal arteries. Embolization is not feasible for these tumors because of the small caliber of the feeding vessels. However, the angiogram is important to define the vascular anatomy for large tumors.
Spinal angiogram demonstrates a large cervical hemangioblastoma. Tumor blush is quite evident on this selective injection. The tumor receives a vascular supply from both the anterior and posterior spinal arteries. Embolization is not feasible for these tumors because of the small caliber of the feeding vessels. However, the angiogram is important to define the vascular anatomy for large tumors.
Typically, the neoplasms are present on the dorsal surface of the spinal cord. These tumors receive their blood supply from the lateral or posterior spinal arteries. The anterior spinal artery mainly supplies neoplasms that abut the ventral pial surface. In contrast, the venous drainage pattern is unpredictable on MRI. These tumors may drain through the anterior or posterior surface veins and in a rostral or caudal direction. However, more extensive edema appears to be present on T2-weighted MRIs when the drainage predominantly occurs via the anterior surface veins.
One study reported on the use of intraoperative indocyanine green (ICG) videoangiography during surgical resection of spinal cord hemangioblastomas in 7 patients. According to the authors, ICG videoangiography clearly revealed the feeding arteries and enlarged draining veins and assisted in defining the tumor borders in 5 of the 7 patients. One patient had a devascularized residual tumor deep in the spinal cord parenchyma that did not take up the fluorescent dye and therefore was not visualized by ICG videoangiography. In another patient, only the draining veins could be visualized in the ventrolateral tumor because it was covered by the spinal cord parenchyma. [16]
-
Sagittal T1-weighted image demonstrates the dorsal location of the tumor, which enhances homogeneously. This tumor does not show any flow voids that may be seen with larger tumors. Note that the spinal cord rostral and caudal to the tumor is quite swollen from edema.
-
T2-weighted image demonstrates the extensive edema typically associated with hemangioblastomas of the spine. This edema extends rostrally to the medulla and caudally to the upper thoracic spinal cord. If the tumor is left untreated, the edema develops into a syrinx.
-
Axial T1-weighted image confirms the dorsal hemangioblastoma that abuts the pial surface, whose position is typical of these tumors and makes removal easy.
-
Spinal angiogram demonstrates a large cervical hemangioblastoma. Tumor blush is quite evident on this selective injection. The tumor receives a vascular supply from both the anterior and posterior spinal arteries. Embolization is not feasible for these tumors because of the small caliber of the feeding vessels. However, the angiogram is important to define the vascular anatomy for large tumors.




