Practice Essentials
Upper extremity deep venous thrombosis (DVT) is an uncommon condition that can cause pulmonary embolism (PE) and septic thrombophlebitis and represents about 5-10% of cases of DVT. [1] Upper extremity DVT should be considered in patients with isolated unilateral upper limb swelling and primarily involves the brachial, axillary, and subclavian veins. [2] There are 2 types of upper extremity deep venous thrombosis: primary (Paget-Schroetter syndrome, or PSS) and secondary. [3, 4, 5] Ultrasonography can facilitate diagnosis in the emergency department. [6]
PSS is an underlying chronic venous compressive abnormality caused by musculoskeletal structures in the costoclavicular space that is present at the thoracic inlet and/or outlet. It typically occurs in the dominant arm of young athletes who are involved in sports that require excessive and repeated motion of the upper extremities, such as wrestling, swimming, gymnastics, football, baseball, and basketball. PSS accounts for only 10-20% of cases of upper extremity DVT. [2]
The secondary form occurs in 14-23% of patients with central venous catheterization or in patients with malignancy. [2] In 75% of patients with secondary thrombosis, hypercoagulability and indwelling central venous catheters are important contributing factors. With central venous catheterization, upper extremity and brachiocephalic venous thrombosis has become a more common problem. [7, 8, 9, 10]
Imaging modalities
Clinical suspicion of upper extremity DVT should be confirmed by imaging procedures such as duplex ultrasonography, CT scan, or MRI. [11] Ultrasonography is the imaging modality of choice. Real-time ultrasonography and color flow Doppler imaging are rapid, noninvasive means used for diagnosing DVT. [2, 12, 13, 14, 15, 16, 17] Lack of full compressibility, absence of color flow signal and augmentation, and visualization of thrombus facilitate the diagnosis.
CT venography and MR venography are not first-line imaging tests but are appropriate to assess central venous structures or to assess the full range of venous structures from the hand to the right atrium. Catheter venography is appropriate if therapy is required. Radionuclide venography and chest radiography usually are not appropriate. [18]
Central veins cannot always be accurately imaged sonographically; therefore, contrast-enhanced venography remains an important diagnostic tool. In assessment of effort-induced thrombosis, venographic views include abduction, external rotation, and extension views.
The strength of magnetic resonance venography lies in evaluation of central veins of the chest; the subclavian vein; the brachiocephalic vein; and the superior vena cava—an area poorly visualized on ultrasonography. Thrombosis is diagnosed as a filling defect in the vessel. [19]
In patients in whom there is a low suspicion of upper extremity DVT, a D-dimer test can help rule it out. Electrocardiography (ECG) should be performed and may show sinus tachycardia. [2] Kleinjan et al used an algorithm consisting of D-dimer testing, clinical decision score, and ultrasonography to exclude upper extremity DVT. [20]
(See the images below of DVT in the upper extremities.)
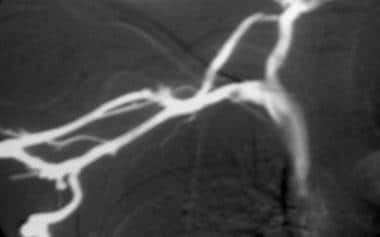
 This contrast-enhanced study was obtained through a Mediport placed through the chest wall through the internal jugular vein to facilitate chemotherapy. A thrombus has propagated peripherally from the tip of the catheter in the superior vena cava into both subclavian veins.
This contrast-enhanced study was obtained through a Mediport placed through the chest wall through the internal jugular vein to facilitate chemotherapy. A thrombus has propagated peripherally from the tip of the catheter in the superior vena cava into both subclavian veins.
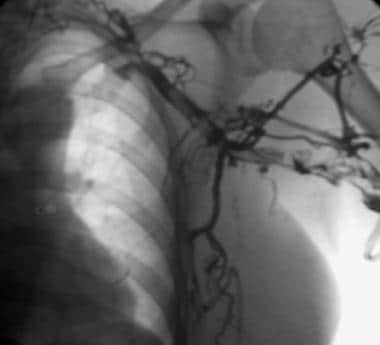
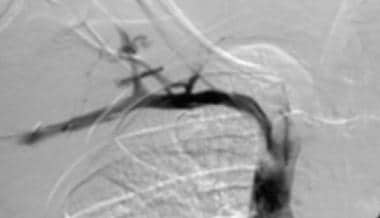
 Thoracic outlet compression syndrome secondary to hypertrophied musculofascial bands. Venogram of the right upper extremity shows a hemodynamically significant, notchlike stenotic defect in the subclavian vein with the patient's arm in the neutral position. Note filling of venous collaterals, even with the arm in the neutral position.
Thoracic outlet compression syndrome secondary to hypertrophied musculofascial bands. Venogram of the right upper extremity shows a hemodynamically significant, notchlike stenotic defect in the subclavian vein with the patient's arm in the neutral position. Note filling of venous collaterals, even with the arm in the neutral position.
Radiography
Plain radiographic findings of a clavicle or first rib fracture or the presence of a cervical rib can increase the suspicion of thoracic outlet syndrome and venous thrombosis.
(See the radiographic images below.)
 This contrast-enhanced study was obtained through a Mediport placed through the chest wall through the internal jugular vein to facilitate chemotherapy. A thrombus has propagated peripherally from the tip of the catheter in the superior vena cava into both subclavian veins.
This contrast-enhanced study was obtained through a Mediport placed through the chest wall through the internal jugular vein to facilitate chemotherapy. A thrombus has propagated peripherally from the tip of the catheter in the superior vena cava into both subclavian veins.
 This image follows a 16-hour catheter-directed thrombolytic infusion of tissue-type plasminogen activator (tPA) into the left axillo-subclavian vein. Interval clot dissolution has occurred, and central flow in the venous system has been restored.
This image follows a 16-hour catheter-directed thrombolytic infusion of tissue-type plasminogen activator (tPA) into the left axillo-subclavian vein. Interval clot dissolution has occurred, and central flow in the venous system has been restored.
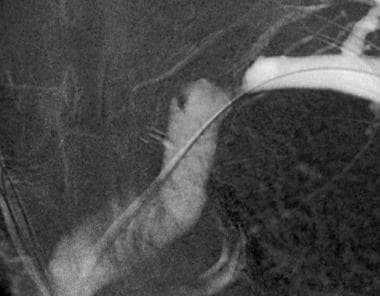
 This image shows thoracic outlet compression syndrome. Percutaneous transluminal angioplasty (PTA) was performed with a 10-mm balloon catheter to treat venous stenosis, which persisted after transaxillary resection of the first rib. Note the significant waist in the balloon before it is completely inflated.
This image shows thoracic outlet compression syndrome. Percutaneous transluminal angioplasty (PTA) was performed with a 10-mm balloon catheter to treat venous stenosis, which persisted after transaxillary resection of the first rib. Note the significant waist in the balloon before it is completely inflated.
Computed Tomography
Computed tomography (CT) is readily available and is widely used in evaluation of UEDVT. Upper extremity or central venous thrombosis is often incidentally diagnosed on contrast-enhanced CT scans of the chest. The thrombus is hypoattenuating compared with the hyperattenuating vein.
This cross-sectional imaging modality provides excellent information about soft tissue structures (eg, tumor, lymphadenopathy) surrounding the vein that may account for thrombosis.
(See the CT images below.)
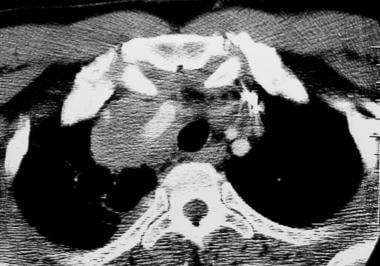
 Superior vena cava syndrome in a patient with lung cancer. CT scan shows a hypoattenuating thrombus that fills the superior vena cava. The patient was treated with anticoagulation alone.
Superior vena cava syndrome in a patient with lung cancer. CT scan shows a hypoattenuating thrombus that fills the superior vena cava. The patient was treated with anticoagulation alone.
Ultrasonography
Compression ultrasonography (CUS) is considered to be the first-line imaging test for diagnosing upper extremity DVT, but it often yields inconclusive test results. Contrast venography (radiography of a vein after injection of a radiopaque fluid) is still considered the diagnostic standard but is an invasive technique. [21]
Compression duplex ultrasonography has been reported to have a sensitivity of 97% and a specificity of 96% for upper extremity DVT. Other imaging modalities, such as MR and CT venography, have been found to be superior to ultrasonography, but their limitations include high cost, radiation exposure, and availability. [2]
The American College of Radiology (ACR) states that ultrasound duplex Doppler imaging is the most appropriate imaging modality to assess upper extremity DVT. It is noninvasive and can be performed at the bedside. Ultrasonography can directly identify thrombus through visualization of echogenic material in the vein and the lack of compression of vein walls from manual external pressure. It can indirectly identify thrombus from altered blood flow patterns and is most appropriate for evaluation of veins peripheral to the brachiocephalic vein. [18]
Angiography
Patients with effort-induced thrombosis (PSS) should undergo bilateral upper extremity venography with provocative maneuvers.
For patients with renal insufficiency or allergy to contrast material, carbon dioxide–based and gadolinium-based materials are alternative contrast agents for venography. These agents can be used for diagnostic venography and for guidance of catheter-directed thrombolysis.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). This disease has occurred in patients with moderate to end-stage renal disease after they were given a gadolinium-based contrast agent to enhance magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA) scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
The patient is positioned with the arm in neutral, extended, and hyperabducted positions. The diagnosis is made when an intraluminal filling defect is seen or when a deep venous structure does not fill and collateral veins are visualized.
Compressive features associated with provocative maneuvers during contrast-enhanced venography can be seen in asymptomatic patients; therefore, not all patients with venous compression have venous thrombosis.
(See the images below.)
 Thoracic outlet compression syndrome secondary to hypertrophied musculofascial bands. Venogram of the right upper extremity shows a hemodynamically significant, notchlike stenotic defect in the subclavian vein with the patient's arm in the neutral position. Note filling of venous collaterals, even with the arm in the neutral position.
Thoracic outlet compression syndrome secondary to hypertrophied musculofascial bands. Venogram of the right upper extremity shows a hemodynamically significant, notchlike stenotic defect in the subclavian vein with the patient's arm in the neutral position. Note filling of venous collaterals, even with the arm in the neutral position.
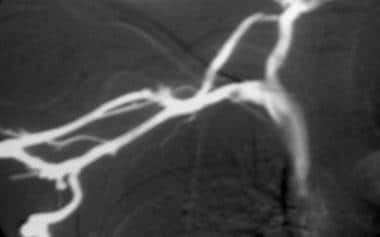
 Postangioplasty contrast-enhanced venogram shows successful treatment of residual venous stenosis after thoracic outlet compression syndrome (TOCS) surgery to decompress the vascular space.
Postangioplasty contrast-enhanced venogram shows successful treatment of residual venous stenosis after thoracic outlet compression syndrome (TOCS) surgery to decompress the vascular space.
 Contrast-enhanced venogram shows critical stenosis of the left subclavian vein in a patient with end-stage renal disease and an arteriovenous fistula in the left arm. The access site in the fistula bleeds excessively after dialysis.
Contrast-enhanced venogram shows critical stenosis of the left subclavian vein in a patient with end-stage renal disease and an arteriovenous fistula in the left arm. The access site in the fistula bleeds excessively after dialysis.
 Contrast-enhanced venogram shows successful treatment of critical stenosis in the left subclavian vein. Good flow has been reestablished.
Contrast-enhanced venogram shows successful treatment of critical stenosis in the left subclavian vein. Good flow has been reestablished.
-
This contrast-enhanced study was obtained through a Mediport placed through the chest wall through the internal jugular vein to facilitate chemotherapy. A thrombus has propagated peripherally from the tip of the catheter in the superior vena cava into both subclavian veins.
-
This image demonstrates thrombus in the left subclavian and axillary veins.
-
This image follows a 16-hour catheter-directed thrombolytic infusion of tissue-type plasminogen activator (tPA) into the left axillo-subclavian vein. Interval clot dissolution has occurred, and central flow in the venous system has been restored.
-
Thoracic outlet compression syndrome secondary to hypertrophied musculofascial bands. Venogram of the right upper extremity shows a hemodynamically significant, notchlike stenotic defect in the subclavian vein with the patient's arm in the neutral position. Note filling of venous collaterals, even with the arm in the neutral position.
-
This image was obtained with the right arm abducted. Note occlusion of the subclavian vein and marked filling of venous collaterals.
-
This image shows thoracic outlet compression syndrome after first rib resection on the right side.
-
This image shows thoracic outlet compression syndrome. Percutaneous transluminal angioplasty (PTA) was performed with a 10-mm balloon catheter to treat venous stenosis, which persisted after transaxillary resection of the first rib. Note the significant waist in the balloon before it is completely inflated.
-
In this image, after full inflation, the waist in the balloon catheter has been eliminated.
-
Postangioplasty contrast-enhanced venogram shows successful treatment of residual venous stenosis after thoracic outlet compression syndrome (TOCS) surgery to decompress the vascular space.
-
Superior vena cava syndrome in a patient with lung cancer. CT scan shows a hypoattenuating thrombus that fills the superior vena cava. The patient was treated with anticoagulation alone.
-
Contrast-enhanced venogram shows critical stenosis of the left subclavian vein in a patient with end-stage renal disease and an arteriovenous fistula in the left arm. The access site in the fistula bleeds excessively after dialysis.
-
Critical stenosis in the left subclavian vein is treated with a Wallstent with 12-mm balloon angioplasty. Stenosis had recurred 3 times after balloon angioplasty alone was performed.
-
Contrast-enhanced venogram shows successful treatment of critical stenosis in the left subclavian vein. Good flow has been reestablished.
-
CT scan in a patient with non-Hodgkin lymphoma shows a soft tissue mass surrounding a hyperintense right brachiocephalic vein.
-
Contrast-enhanced venogram shows circumferential narrowing of the right brachiocephalic vein in a patient with non-Hodgkin lymphoma.