Practice Essentials
The biophysical profile (BPP) is a noninvasive test that predicts the presence or absence of fetal asphyxia and, ultimately, the risk of fetal death in the antenatal period. [1] When the BPP identifies a compromised fetus, measures can be taken to intervene before progressive metabolic acidosis leads to fetal death. [2, 3, 4] The BPP combines data from 2 sources: ultrasonographic imaging and fetal heart rate [FHR] monitoring. Dynamic real-time B-mode ultrasonography is used to measure the amniotic fluid volume (AFV) and to observe several types of fetal movement. The FHR is obtained using a pulsed Doppler transducer integrated with a high-speed microprocessor, which provides a continuously updated reading. [5, 6, 7, 8, 9, 10]
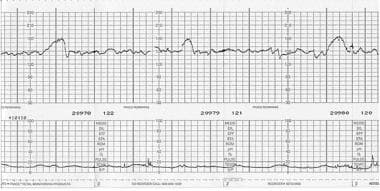 Reactive nonstress test. The top graph plots the fetal heart rate over time. Each small box represents 10 seconds along the horizontal axis and 10 beats per minute along the vertical axis. The baseline fetal heart rate is from 140-150 beats per minute. This tracing is reactive, since at least 2 accelerations of the fetal heart rate occur within less than 20 minutes.
Reactive nonstress test. The top graph plots the fetal heart rate over time. Each small box represents 10 seconds along the horizontal axis and 10 beats per minute along the vertical axis. The baseline fetal heart rate is from 140-150 beats per minute. This tracing is reactive, since at least 2 accelerations of the fetal heart rate occur within less than 20 minutes.
Originally described by Manning and colleagues, [11, 12] the BPP has become a standard tool for providing antepartum fetal surveillance. The BPP integrates 5 parameters to yield a biophysical profile score (BPS):
- The nonstress test (NST)
- Ultrasonographic measurement of the AFV
- Observation of the presence or absence of fetal breathing movements
- Gross body movements
- Tone
A basic principle of antepartum testing is that a more accurate prediction of fetal wellness is achieved in direct proportion to the number of variables considered. The BPP is a clinical tool that integrates levels of dynamic biophysical activities into a usable standard. [13] The BPP allows 2 points for each parameter that is present, yielding a maximum score of 10; however, if all ultrasonographic variables are normal, the FHR variable may be excluded because no change is made in the predictive accuracy of the BPP by including the FHR. If 1 or more ultrasonographic variables are abnormal, the NST should be performed. [14]
A biophysical profile is only able to diagnose oligohydramnios or polyhadramnios, with a score of 8 to 10 being normal. A score of 6 is considered equivoval or abnormal, a score of 2 to 4 is considered not reassuring, and a score of zero indicates urgent need for cesarean section to prevent asphyxia. [1, 15]
Table 1. Criteria for Coding Fetal Biophysical Variables as Normal or Abnormal (Open Table in a new window)
Biophysical Variable |
Normal (Score = 2) |
Abnormal (Score = 0) |
Fetal breathing movements* |
1 or more episodes of ≥20 s within 30 min |
Absent or no episode of ≥20 s within 30 min |
Gross body movements |
2 or more discrete body/ limb movements within 30 min (episodes of active continuous movement considered as a single movement) |
< 2 episodes of body/limb movements within 30 min |
Fetal tone |
1 or more episodes of active extension with return to flexion of fetal limb(s) or trunk (opening and closing of hand considered normal tone) |
Slow extension with return to partial flexion, movement of limb in full extension, absent fetal movement, or partially open fetal hand |
Reactive FHR |
2 or more episodes of acceleration of ≥15 beats per minute (bpm) and of >15 s associated with fetal movement within 20 min |
1 or more episodes of acceleration of fetal heart rate or acceleration of < 15 bpm within 20 min |
Qualitative AFV |
1 or more pockets of fluid measuring ≥2 cm in vertical axis |
Either no pockets or largest pocket < 2 cm in vertical axis |
*Note: The current clinical management guidelines from the American College of Obstetrics and Gynecology [1] maintain the original findings from Manning et al in 1987. [14] These include the following:
Reprinted with permission from Manning, 1999 |
||
Each of the movements evaluated in the BPP results from efferent signals originating in different central nervous system (CNS) centers, which mature at different gestational ages (see Table 2).
Table 2. Maturation of Central Nervous System Regulatory Centers (Open Table in a new window)
Activity |
Gestational Age of Maturation (wk) |
Gross body movements |
6 |
Breathing movements |
12-14 |
FHR accelerations resulting from fetal movement |
18-20 |
Sleep-wake cycles |
18-22 |
Integrated behavioral patterns |
28 |
Table 3 shows a variety of factors, other than hypoxemia, that have been shown to affect different BPP parameters.
Table 3. Factors Affecting the Biophysical Profile (Open Table in a new window)
Activity |
FHR Accelerations |
Tone |
Gross Movement |
Fetal Breathing |
AFV |
Fetal sleep |
⇓ |
⇓ |
⇓ |
⇓ |
|
Early gestational age (< 33 wk) |
⇓ |
|
|
⇓ |
|
Late gestational age (>42 wk) |
⇓ |
⇓ |
|
⇓ |
⇓ |
Maternal glucose ingestion |
— |
|
— |
⇑ |
|
Maternal alcohol ingestion |
|
⇓/— |
|
⇑/— |
|
Maternal magnesium administration |
⇓ |
|
|
⇓ |
|
Artificial rupture of membranes |
|
|
|
⇓ |
⇓ |
Premature rupture of membranes |
|
|
|
|
⇓ |
Labor |
|
|
|
⇓ |
|
Key: A blank box indicates that no data are available for that parameter. Horizontal lines indicate that the parameter has been studied and that no change is demonstrated. Arrows indicate that the parameter has been studied and that it increases or decreases as shown. |
|||||
Application of the Biophysical Profile
Antepartum testing using the biophysical profile (BPP) or any other method should not be performed earlier than the gestational age at which extrauterine survival or active intervention for fetal compromise is possible. Furthermore, no indications exist for testing in a fetus at term when likelihood of successful induction is high or when vaginal delivery is contraindicated for obstetric reasons. For patients with a low probability of successful induction, the BPP is a useful tool that can be used while waiting for cervical ripening. In these patients, the purpose of the BPP is to avoid the maternal morbidity resulting from failed induction followed by cesarean delivery.
The frequency of testing varies according to the clinical variables in each patient. In most high-risk pregnancies, testing plans start with weekly testing, [16] although twice-weekly testing is the standard for pregnancies beyond 42 weeks and for patients with insulin-dependent diabetes. [17] Frequency of testing increases in direct proportion to the severity of the maternal or fetal condition.
In unstable pregnancies with progressive deterioration of the fetal condition, abnormal umbilical cord blood flow patterns occur first. Subsequently, FHR variation is reduced, followed by loss of breathing movements, while general fetal movements and tone are the last parameters to demonstrate abnormal results. Frequent assessment of fetal BPP movements may help prolong the pregnancy in fetuses with a marginally reduced FHR variation.
An abnormal BPS should prompt further evaluation or intervention depending on the circumstances. If an abnormal score occurs in a term fetus, preparation should be made for delivery. An abnormal score in a fetus remote from term requires conservative management, since the risk of fetal death is similar to the neonatal mortality rate resulting from prematurity. In these patients, daily testing often is performed.
Modified Biophysical Profile
The modified BPP (mBPP) combines the NST, as a short-term indicator of fetal acid–base status, with an amniotic fluid volume assessment, as an indicator of long-term placental function. Thus, the results of the mBPP are considered normal if the NST is reactive and the amniotic fluid volume is greater than 2 cm in the deepest vertical pocket and are considered abnormal if either the NST is nonreactive or amniotic fluid volume in the deepest vertical pocket is 2 cm or less (ie, oligohydramnios is present). [18] If either the NST or the amniotic fluid volume is abnormal, a complete BPP or a contraction stress test (CST) is performed. [1]
Guidelines
According to the American College of Radiology (ACR) apporpriateness criteria, the judicious use of tests of fetal well-being is recommended to optimize perinatal outcome in pregnancies with higher rates of stillbirth. Maternal factors that may increase the reisk of poor perinatal outcome include the following: advanced maternal age, obesity, hypertension, cyanotic heart disease, thrombophilia, diabetes, thyroid disorders, chronic renal disease, connective tissue disease, cholestasis, hemoglobinopathies, isoimmunization, and a history of unexplained stillbirth. Fetal factors include intrauterine fetal growth restriction (IUGR), certain structural anomalies, genetic syndromes, fetal arrhythmias, blood group incompatibilities, fetal anemia, congenital infections, and multiple gestations. [18]
The American College of Obstetricians and Gynecologists guidelines recommend the following [1] :
-
Antepartum fetal testing at 32 weeks' gestation is appropriate for most high-risk patients.
-
If the maternal medical condition is stable and test results are reassuring, fetal monitoring (NST, BPP, modified BPP, or CST) are typically repeated at weekly intervals.
-
In the absence of obstetric contraindications, delivery of the fetus with an abnormal test result often may be attempted by induction of labor, with continuous intrapartum monitoring of the FHR and uterine contraction
Reliability
The biophysical profile (BPP) is a reliable method of predicting fetal survival. Testing methods are usually evaluated by comparing the false-negative mortality rate for each method. The false-negative mortality rate is defined as the number of fetal deaths, corrected for lethal congenital anomalies and unpredictable causes of demise, that occur within 1 week of a normal test result. The BPP has a false-negative mortality rate of 0.77 deaths per 1000 tests. Furthermore, the BPS highly correlates with the antepartum fetal umbilical venous cord pH level. [18, 19, 20, 21]
Biophysical Profile Procedure
The ultrasonographic portion of the biophysical profile (BPP) should begin with notation of the starting time. The profile may be completed when all of the variables have been observed; however, a full 30 minutes must elapse before the profile is judged to be abnormal. The scan should start with a general survey, noting the position of the fetus and the presence of cardiac activity. Although not part of the BPP, surveying the placental position and grade and the fetal morphology is common practice during observation of fetal activity.
Amniotic fluid volume (AFV) is assessed as normal if 1 or more pockets of fluid are detected that measure at least 2 cm along the vertical axis. Oligohydramnios is present if the largest pocket measures less than 2 cm.
The pressure applied to the transducer by the sonographer is inversely proportional to the depth of the fluid pocket. [22] Careful attention to transducer pressure is required to avoid a false diagnosis of oligohydramnios, which can result from excessive transducer pressure compressing the maternal abdomen.
Fetal movements are judged as normal or abnormal according to the criteria established in Table 1. The first video below shows breathing movements, while the second video shows movements that can be mistaken for fetal breathing.
The following videos demonstrate gross movements of the lower and upper body and tone.
The video below demonstrates the amniotic fluid index (AFI) by measuring 4 pockets of fluid.
Amniotic Fluid Index
The AFI is a semiquantitative method for evaluating the AFV. The AFI is derived by adding the largest vertically measured fluid pocket from each uterine quadrant. This method appears to be at least as accurate as the largest–pocket-of-fluid method and can reasonably be substituted as an alternative method for evaluating AFV in the biophysical profile (BPP). Using this method, oligohydramnios is defined as an AFI of less than 5. [23, 24, 25]
To obtain an AFI, the mother must be in the supine position and the linear ultrasonographic probe must be parallel to the maternal spine and perpendicular to the floor for all measurements. The abdomen is divided into 4 quadrants, with the umbilicus delineating the upper and lower halves and the linea nigra delineating the left and right halves.
The largest pocket of fluid in each quadrant is measured along the vertical dimension, which is the dimension perpendicular to the ultrasonographic probe. The pockets must be free of umbilical cord or fetal extremities, although brief appearances of these are acceptable. The video below demonstrates measurement of the AFI.
-
Reactive nonstress test. The top graph plots the fetal heart rate over time. Each small box represents 10 seconds along the horizontal axis and 10 beats per minute along the vertical axis. The baseline fetal heart rate is from 140-150 beats per minute. This tracing is reactive, since at least 2 accelerations of the fetal heart rate occur within less than 20 minutes.
-
Fetal breathing movements. Video shows a rhythmic deflection of the fetal chest wall and diaphragm that is clearly distinct from the rhythmic motion of the fetal heart. Note that the image begins in the transverse view, but the ultrasound transducer is then rotated to show a sagittal view and, finally, an oblique view. The episode of continuous fetal breathing lasts well in excess of the required 20-second period.
-
False fetal breathing movements. Although some transient fetal breathing movements are seen, the video does not include 20 seconds of continuous fetal breathing. Note that the maternal breathing and aortic pulse seen posteriorly and the fetal aortic pulse seen on the sagittal view, along with fetal cardiac activity, can cause deflections of the fetal chest wall, which can be mistaken for fetal breathing movements.
-
Gross fetal movements and tone. Video demonstrates generalized movements of the fetal lower extremities, including 1 episode of flexion and extension.
-
Gross fetal movements and tone. Video demonstrates generalized movements of the fetal upper extremities. The upper extremity rests in front of the fetal chest and chin. Although the ultrasound transducer is moving laterally across the maternal abdomen, 2 distinct episodes of flexion and extension are seen. Note the many cross-sectional views of the 3-vessel umbilical cord and the floating echogenic particles of vernix in the amniotic fluid.
-
Amniotic fluid index. The largest pocket of fluid is measured in each quadrant of the maternal abdomen in the vertical dimension. Then, each value is added to yield the amniotic fluid index.








