Practice Essentials
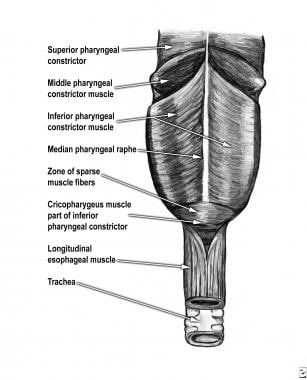
A diverticulum is an outpouching that protrudes from the wall of a viscus. As with the entire gastrointestinal tract, diverticula of the hypopharynx may be true or false, depending on the number of layers of the viscus wall that are involved. A Zenker diverticulum is a false diverticulum consisting of mucosa and submucosa that arises from the posterior portion of the inferior pharyngeal constrictor muscle. True diverticula consist of all layers of the wall, whereas false diverticula generally lack the muscularis layer. [1, 2, 3, 4, 5, 6, 7]
The prevalence of Zenker diverticulum has been reported to be between 0.01 and 0.11%. It rarely occurs in persons younger than 40 years, and is usually discovered in the 7th or 8th decade of life. [8, 6, 9, 10]
(See the images below.)
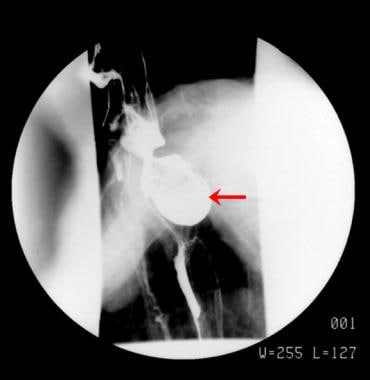 Single spot radiograph from a barium esophagographic series demonstrates a moderate-sized Zenker diverticulum (arrow) that protrudes posteriorly from the hypopharynx.
Single spot radiograph from a barium esophagographic series demonstrates a moderate-sized Zenker diverticulum (arrow) that protrudes posteriorly from the hypopharynx.
Preferred examination
Fluoroscopic barium esophagography is the mainstay for diagnosis of Zenker diverticulum. [4] Physical examination findings are rare, although some extremely large diverticula are occasionally palpable on examination. These are usually to the left of midline.
Barium swallow with videofluoroscopy provides information about the size, location, and character of the mucosal lining of the Zenker diverticulum (see the images below).
 Images obtained during barium swallow videofluoroscopy demonstrating an intermediate-sized Zenker diverticulum.
Images obtained during barium swallow videofluoroscopy demonstrating an intermediate-sized Zenker diverticulum.
 Illustrated barium swallow demonstrates the pouch retaining contrast and its connection to the esophagus immediately inferior and posterior to the larynx.
Illustrated barium swallow demonstrates the pouch retaining contrast and its connection to the esophagus immediately inferior and posterior to the larynx.
Fluoroscopic studies of the upper GI tract have shown that the prevalence of Zenker diverticulum is 0.01-0.1%. Zenker diverticulum is found in approximately 2% of patients with nonspecific dysphagia who are referred for fluoroscopy.
Preoperative assessment of dysphagia characteristics, using fiberoptic endoscopic evaluation of swallowing, in patients with Zenker diverticulum revealed that postswallow hypopharyngeal reflux (PSHR) is predictive of a diverticulum larger than 1 cm and may be useful in surgical planning. PSHR was less frequent in patients with small diverticula (17%) than in those with medium (91%) and large diverticula (87%). According to the authors of the study, PSHR is also helpful in identifying patients with recurrent or residual symptomatic Zenker diverticulum after surgical treatment. [11]
Zenker diverticulum may be found on endoscopy; however, fluoroscopy remains the diagnostic study of choice. Care must be taken in performing endoscopy in patients with known Zenker diverticulum, as passage of the endoscope into the diverticulum carries some risk of perforation. Endoscopy may be indicated if the radiographic findings suggest carcinoma. The main limitation of barium esophagography is patient cooperation.
When incidentally imaged on MRI or CT, a Zenker diverticulum appears as a structure arising posteriorly from the hypopharynx. It is filled with gas, fluid, or a mixture of these.
Staging
The following staging systems are used for Zenker diverticula, as assessed by barium swallow videofluoroscopy:
Lahey staging
Criteria of the Lahey staging system are as follows:
-
Stage I - A small mucosal protrusion is present
-
Stage II - A definite sac is present, but the hypopharynx and esophagus are in line
-
Stage III - The hypopharynx is in line with diverticulum, and the esophagus is indented and pushed anteriorly.
Morton staging
Criteria of the Morton staging system are as follows:
-
Small sacs are less than 2 cm in length
-
Intermediate sacs are 2-4 cm in length
-
Large sacs are greater than 4 cm in length
Van Overbeek staging
Criteria of the van Overbeek system are as follows:
-
Small sacs are less than 1 vertebral body in length
-
Intermediate sacs are 1-3 vertebral bodies in length
-
Large sacs are greater than 3 vertebral bodies in length
Radiography
The fluoroscopic barium esophagram is the primary tool for the diagnosis of Zenker diverticulum. (See the image below.) The diverticulum appears as an outpouching arising from the midline of the posterior wall of the distal pharynx near the pharyngoesophageal junction. [12] This is best identified during swallowing and is best seen on the lateral view, on which the diverticulum is typically noted at the C5-6 level.
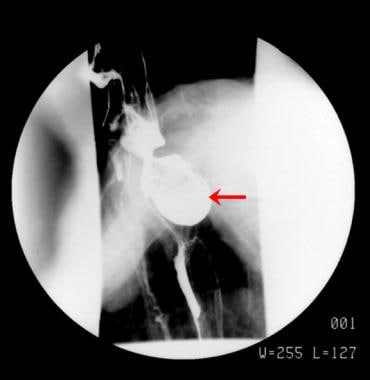 Single spot radiograph from a barium esophagographic series demonstrates a moderate-sized Zenker diverticulum (arrow) that protrudes posteriorly from the hypopharynx.
Single spot radiograph from a barium esophagographic series demonstrates a moderate-sized Zenker diverticulum (arrow) that protrudes posteriorly from the hypopharynx.
Frequently, a posterior bar representing a prominent cricopharyngeus muscle is noted as the contrast bolus passes. As the contrast bolus normally travels quickly through the pharynx and upper esophagus, careful observation during fluoroscopy is necessary, and videofluoroscopy is helpful for documentation purposes. [13]
When the diverticulum is large enough to protrude laterally, it protrudes to the left in 90% of cases. After the contrast agent bolus passes the upper esophagus, the diverticulum is typically seen extending posterior to the cricopharyngeus muscle, and contrast material that was trapped within the diverticulum may be regurgitated back into the hypopharynx.
A Valsalva maneuver may be helpful in visualizing the diverticulum after swallowing. Occasionally, a patient may aspirate contrast material from the diverticulum. Pay attention to the lumen of the diverticulum because irregularities or filling defects within the diverticulum may indicate the rare complication of squamous cell carcinoma.
When Zenker diverticulum is demonstrated on fluoroscopy, clearing of any residual contrast material within the diverticulum should be confirmed, as aspiration can occur.
Barium may become trapped above a cricopharyngeal muscle that has closed before the pharyngeal contraction has passed, and this may mimic the appearance of a Zenker diverticulum. This pseudo-Zenker diverticulum can be distinguished from a true Zenker diverticulum by means of fluoroscopic observation. The pseudo-Zenker diverticulum does not protrude beyond the expected location of the posterior pharyngeal wall, and it generally does not persist after the contrast agent bolus has passed.
Computed Tomography
When incidentally imaged on computed tomography (CT) scans, a Zenker diverticulum appears as a structure arising posteriorly from the hypopharynx and is filled with gas, fluid, oral contrast material, or a mixture of these. (See the image below.)
 A Zenker diverticulum (arrow) is noted incidentally on a thoracic CT scan. It is filled with gas and particulate matter.
A Zenker diverticulum (arrow) is noted incidentally on a thoracic CT scan. It is filled with gas and particulate matter.
Ultrasonography
Although barium esophagram is usually used to confirm the diagnosis, a study by Cui et used swallow contrast-enhanced ultrasound to detect Zenker diverticulum. In 10 patients, Zenker diverticulum appeared as a pouch-shaped structure at the posterior pharyngoesophageal junction that retained ultrasound contrast agent for longer than 3 minutes. All 10 patients underwent a barium esophagram as the gold standard. Contrast-enhanced ultrasound can provide bedside availability without radiation exposure. [14]
-
Single spot radiograph from a barium esophagographic series demonstrates a moderate-sized Zenker diverticulum (arrow) that protrudes posteriorly from the hypopharynx.
-
A Zenker diverticulum (arrow) is noted incidentally on a thoracic CT scan. It is filled with gas and particulate matter.
-
Zenker diverticulum. Anatomy of the pharynx.
-
Images obtained during barium swallow videofluoroscopy demonstrating an intermediate-sized Zenker diverticulum.
-
Illustrated barium swallow demonstrates the pouch retaining contrast and its connection to the esophagus immediately inferior and posterior to the larynx.