Practice Essentials
Classified as a hereditary phakomatosis, von Hippel-Lindau syndrome (VHL) is an autosomal dominant, inherited, neurocutaneous dysplasia complex with an 80-100% penetrance and variable delayed expressivity. Sex distributions are equal, and 20% of cases are familial. VHL is characterized by a predisposition to bilateral and multicentric retinal angiomas, central nervous system (CNS) hemangioblastomas (HBs); renal cell carcinomas (RCCs); pheochromocytoma; islet cell tumors of the pancreas; endolymphatic sac tumors (ELSTs) [1] ; and renal, pancreatic, and epididymal cysts. [2, 3] CNS hemangioblastoma (Lindau tumor) is the most commonly recognized manifestation of VHL and occurs in 40% of patients. [4, 5]
Symptoms often begin in the second to third decades of life. Patients may present with ocular signs and/or symptoms due to retinal hemorrhage, retinal detachment, glaucoma, or uveitis. Funduscopic examination may reveal tortuous aneurysms of the retinal vessels, exudates on the fundus, and subretinal yellowish spots. Patients may present with neurologic symptoms such as headaches, ataxia, and blindness. The exact neurologic deficit depends on the site of the primary lesion.
Imaging modalities
Tumors at various sites are demonstrable by using different imaging modalities, including ultrasonography, CT, MRI, radionuclide studies, and angiography. The preferred examination depends on the site or organ involved. CT and MRI best depict intracranial lesions, but MRI is more appropriate for examining spinal lesions. Although retinal tumors are visualized best on sonograms, the kidneys and pancreas can be imaged by using MRI sonograms and/or CT scans. [6, 7] When asymptomatic patients and at-risk relatives are screened, noninvasive techniques should be emphasized. Preferably, those not involving ionizing radiation, such as ultrasonography and MRI, should be used. [8, 9, 10, 11, 12]
The limitation of various techniques depends on the size of the tumor and on problems with atypia. CT is an excellent modality for detecting tumors anywhere in the body, but it has the disadvantage of ionizing radiation, which may become problematic in screening asymptomatic patients and at-risk relatives.
According to guidelines recommendations, follow-up imaging in VHL disease is recommended every 2-3 years. [13] Most centers perform separate MRI exams for each body region (abdomen, brain, spine), necessitating multiple expensive examinations. CNS accumulation of gadolinium-based contrast agents has been reported in nearly all patients included in a screening program for VHL disease. [14] Focused whole-body MRI screening protocols have been proposed to reduce the exposure to contrast agents. [15]
(Images of VHL are shown below,)
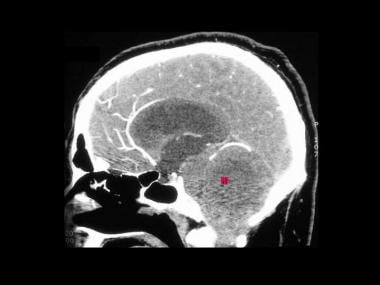
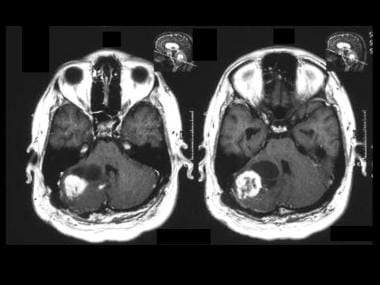
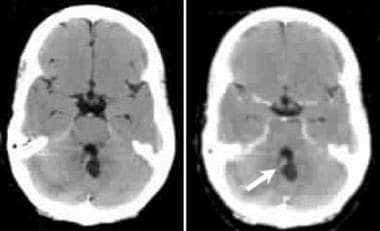 von Hippel-Lindau syndrome. Transaxial nonenhanced and contrast-enhanced CT scans through the cerebellum in a 34-year-old patient with a family history of VHL. Scans show a midline cerebellar cystic lesion with an enhancing nodule (arrow) due to cerebellar hemangioblastoma.
von Hippel-Lindau syndrome. Transaxial nonenhanced and contrast-enhanced CT scans through the cerebellum in a 34-year-old patient with a family history of VHL. Scans show a midline cerebellar cystic lesion with an enhancing nodule (arrow) due to cerebellar hemangioblastoma.
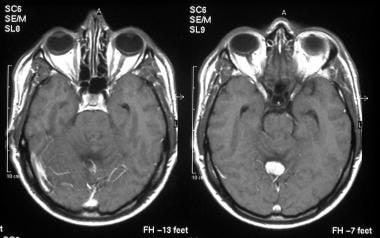 von Hippel-Lindau syndrome. T1-weighted transaxial gadolinium-enhanced MRIs of the same patient as in the previous image show a well-defined hypervascular enhancing mass.
von Hippel-Lindau syndrome. T1-weighted transaxial gadolinium-enhanced MRIs of the same patient as in the previous image show a well-defined hypervascular enhancing mass.
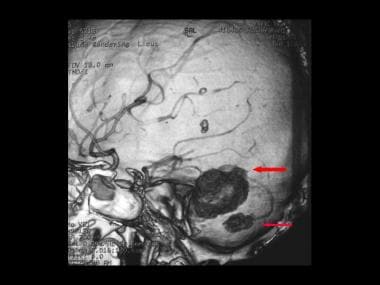
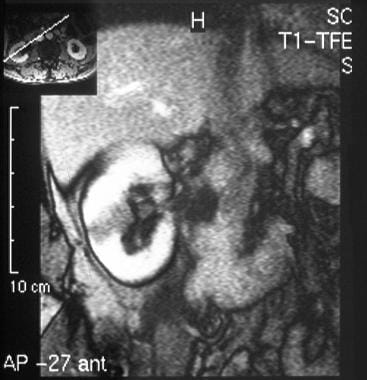
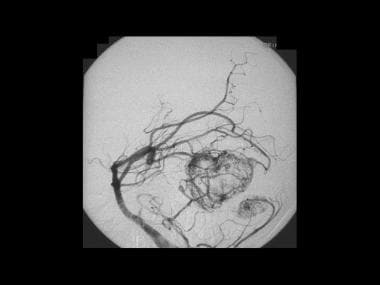
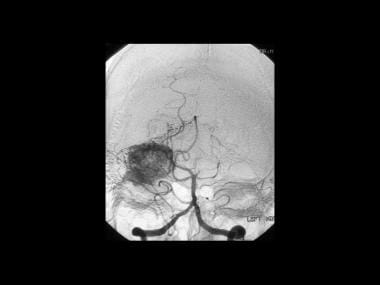
 von Hippel-Lindau syndrome. Coronal vertebral angiogram of the same patient as in the previous 2 images shows a hypervascular intramural nodule that demonstrates a prolonged and intense enhancement with a surrounding avascular area, which represents the cyst surrounding the mural nodule. Note the stretching around the cyst.
von Hippel-Lindau syndrome. Coronal vertebral angiogram of the same patient as in the previous 2 images shows a hypervascular intramural nodule that demonstrates a prolonged and intense enhancement with a surrounding avascular area, which represents the cyst surrounding the mural nodule. Note the stretching around the cyst.
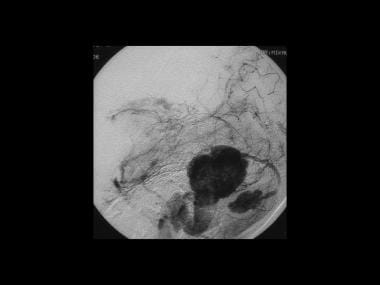
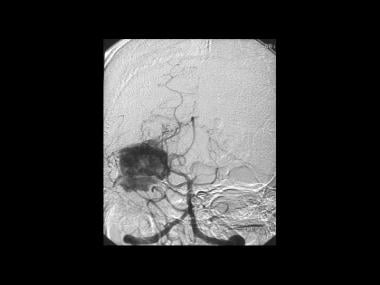
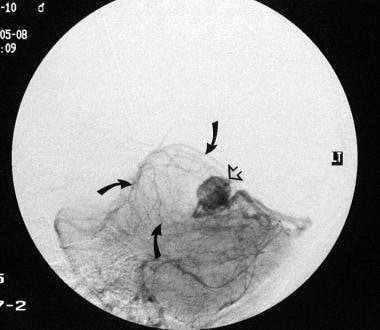 von Hippel-Lindau syndrome. Sagittal vertebral angiogram of the same patient as in the previous 3 images shows a hypervascular intramural nodule (open arrow) that demonstrates a prolonged and intense enhancement with a surrounding avascular area, representing the cyst surrounding the mural nodule (solid arrows). Note the stretching of vessels around the cyst. The final diagnosis was a cerebellar hemangioblastoma associated with von Hippel-Lindau syndrome (same patient as in Images 1-3).
von Hippel-Lindau syndrome. Sagittal vertebral angiogram of the same patient as in the previous 3 images shows a hypervascular intramural nodule (open arrow) that demonstrates a prolonged and intense enhancement with a surrounding avascular area, representing the cyst surrounding the mural nodule (solid arrows). Note the stretching of vessels around the cyst. The final diagnosis was a cerebellar hemangioblastoma associated with von Hippel-Lindau syndrome (same patient as in Images 1-3).
The clinical diagnosis of VHL can be made (1) in patients with a family history of VHL and at least 1 of the characteristic VHL-related tumors, including retinal hemangioblastomas (HBs), CNS HBs, clear cell renal cell carcinomas (RCCs), pancreatic neuroendocrine tumors (NETs), and endolymphatic sac tumors); (2) if 2 or more retinal or CNS HBs are present; or (3) in the presence of 1 retinal or CNS HB, along with at least 1 of the characteristic VHL-related visceral tumors, excluding renal and epididymal cysts. [16, 17]
Cambridge protocol
The Cambridge protocol was devised by Maher et al for screening patients with VHL disease or at-risk relatives. The protocol is as follows [18] :
Affected asymptomatic patient:
-
Annual physical examination and urine test
-
Annual direct and indirect ophthalmoscopy
-
Annual fluorescein angiography or angiography
-
Annual renal ultrasonographic examination
-
MRI or CT scan of the brain every 3 years to age 50 years then every 5 years thereafter
-
Abdominal CT scanning every 3 years (more often if multiple renal cysts are present)
-
Annual 24-hour urine collection for vanillylmandelic acid (VMA) levels
At-risk relatives - The same protocol is followed as for asymptomatic patients, apart from age limits, which are as follows:
-
Annual direct and indirect ophthalmoscopy from age 5 years
-
Annual fluorescein angiography or angiography from age 10 years until age 60 years
-
MRI or CT scanning of the brain every 3 years from ages 15-40 years, then every 5 years until age 60 years
-
Abdominal CT scanning every 3 years from ages 20-65 years
VHL Alliance Surveillance Guidelines
The VHL Alliance surveillance guidelines suggest that surveillance should start at birth and continue throughout the patient's life. Special precautions are required during pregnancy. The recommendations by age are as follow [13] :
At Birth:
-
Clinical evaluation for neurologic disturbance and routine newborn hearing tests
-
Ophthalmic exam to look for nystagmus, strabismus, white pupil, and other signs that may indicate need for a referral to a retinal specialist
Ages 1-4:
-
Annual comprehensive ophthalmic examination with indirect ophthalmoscope
-
Annual clinical evaluation for signs of neurologic disturbance, nystagmus, strabismus, white pupil, and abnormalities in blood pressure, hearing, or vision
Ages 5-15:
-
Annual physical examination and neurologic assessment, with particular attention to blood pressure (taken while lying down and standing), hearing impairment, neurologic disturbance, nystagmus, strabismus, white pupil, and other signs indicating retinal problems
-
Annual comprehensive ophthalmic examination with indirect ophthalmoscope
-
Annual biochemical tests, including plasma metanephrine or 24-hour urinary metanephrine levels
-
Annual abdominal ultrasonography from 8 years or earlier if indicated
-
Abdominal MRI or MIBG scintigraphy scan only if biochemical abnormalities found
-
Every 2-3 years, audiology assessment by an audiologist; then annually if any hearing loss, tinnitus, or vertigo is found
-
In the case of repeated ear infections, MRI with contrast of the internal auditory canal using thin slices, to check for a possible endolymphatic sac tumor (ELST)
Ages 16 and older:
-
Annual comprehensive ophthalmic examination with indirect ophthalmoscope
-
Annual clinical evaluation for signs of neurologic disturbance and abnormalities in blood pressure, hearing or vision
-
Quality ultrasound and at least every other year when not pregnant, and MRI scan of abdomen with and without contrast to assess kidneys, pancreas, and adrenals.
-
Annual biochemical tests, including plasma metanephrine or 24-hour urinary metanephrine levels
-
Abdominal MRI or MIBG scintigraphy scan only if biochemical abnormalities found
-
Every 2-3 years, MRI scans should be ordered as no less than a 1.5T MRI with and without contrast of brain, cervical, thoracic, and lumbar spine, with thin cuts through the posterior fossa, and attention to inner ear/petrous temporal bone to rule out both ELST and hemangioblastomas of the neuraxis.
-
Audiology assessment by an audiologist every 2-3 years
Intervention
Preoperative embolization is not generally used but may be helpful before surgical resection of endolymphatic sac tumors and hemangioblastomas in selected cases. [19, 20, 1]
Treatment involves resection of the offending tumor, aspiration of the cysts causing pressure-related symptoms, photocoagulation, and cryotherapy of any retinal lesions. Radiology has a central role in managing VHL. Because a conservative approach to the treatment of VHL lesions is now more widely accepted, ongoing follow-up with careful ultrasonographic and MRI screening will play a central role in evaluating the progression of disease. [21]
Radiography
Plain radiographs have little to contribute to the diagnosis of von Hippel-Lindau syndrome. Calcification within the orbits in retinal lesions may be difficult to see. The rare, associated bone cysts and osseous hemangiomas may be fairly well defined on plain radiographs. [22, 23] Hemangiomas of the bone must be differentiated from osteoblastic metastases, lesions due to Paget disease, lymphoma, and monostotic fibrous dysplasia.
(See the image below.)
 von Hippel-Lindau syndrome. A 16-year-old female adolescent with a family history of von Hippel-Lindau syndrome presented with generalized bone pain, weight loss, and hypertension. This skull radiograph was part of the skeletal survey. The lateral skull radiograph demonstrates well-defined lytic lesions throughout the calvarium.
von Hippel-Lindau syndrome. A 16-year-old female adolescent with a family history of von Hippel-Lindau syndrome presented with generalized bone pain, weight loss, and hypertension. This skull radiograph was part of the skeletal survey. The lateral skull radiograph demonstrates well-defined lytic lesions throughout the calvarium.
Computed Tomography
Hemangioblastomas of the CNS are demonstrated as cystic lesions with a 3- to 15-mm mural nodule in 75% of patients. They are demonstrated as an enhancing lesion with multiple cystic areas in 15% of patients and as an enhancing solid mass in 10%. The cerebellum is most commonly involved, followed by the medulla, the spinal cord, and even the spinal nerve roots. Supratentorial hemangioblastomas are rare, but they have been reported. [22, 23, 24, 25]
Hemangioblastomas usually do not become calcified, and this is a finding that helps in differentiating these lesions from cystic astrocytomas (which are calcified in 25% of patients). Typical pilocytic cystic astrocytomas also occur in patients much younger than most patients with hemangioblastomas.
Choroidal capillary hemangiomas are aggressive lesions that are histologically similar to cerebellar hemangioblastomas. Approximately 25-30% of these lesions occur in patients with VHL. CT scans demonstrate enhancing lesions.
Retinal hemangiomas are too small to be depicted on CT scans, and the diagnosis chiefly depends on the results of an ophthalmoscopic examination.
CT has a low sensitivity in the detection of renal cell carcinoma associated with von Hippel-Lindau syndrome because of its inability to reliably differentiate cystic renal cell carcinomas, cancers within a cyst, and atypical cysts. Therefore, a multimodality approach is more appropriate.
Renal adenomas are potentially premalignant. These adenomas are usually smaller than 3 cm, are subcapsular cortical, and are impossible to differentiate from renal cell carcinomas. They are multiple in 25% of patients.
Endolymphatic sac tumors are destructive and contain calcification centered on the retrolabyrinthine region. All papillary endolymphatic sac tumors have a thin peripheral rim of calcification, representing the expanded cortex of petrous bone. Endolymphatic sac tumors are slow growing and spread in 2 directions (ie, laterally toward the external ear, in the direction of the jugular foramen, and medially into the cerebellopontine angle).
On CT scans, the margins of these tumors are geographic or moth-eaten in appearance, and the intratumoral bone appears reticular or spiculated. After the intravenous administration of contrast material, areas of patchy enhancement are interspersed with cystic areas. Although the lesion is a benign lesion, it typically has elevated tumor blood volume on perfusion CT, which is more typical for malignant lesions.
(See the following computed tomography scans depicting von Hippel-Lindau syndrome.)
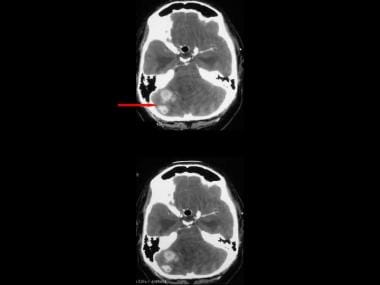
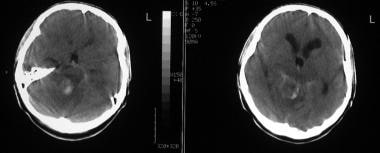 von Hippel-Lindau syndrome. Axial nonenhanced CT scan of the head in a patient with known von Hippel-Lindau syndrome and an acute neurologic presentation shows hyperattenuating areas within a right cerebellar tumor suggestive of hemorrhage. Note that the tumor is causing moderate hydrocephalus.
von Hippel-Lindau syndrome. Axial nonenhanced CT scan of the head in a patient with known von Hippel-Lindau syndrome and an acute neurologic presentation shows hyperattenuating areas within a right cerebellar tumor suggestive of hemorrhage. Note that the tumor is causing moderate hydrocephalus.
 von Hippel-Lindau syndrome. Transaxial bone-window CT scan through the head shows destructive lesions throughout the calvarium. Some lesions cross the entire thickness of the skull.
von Hippel-Lindau syndrome. Transaxial bone-window CT scan through the head shows destructive lesions throughout the calvarium. Some lesions cross the entire thickness of the skull.
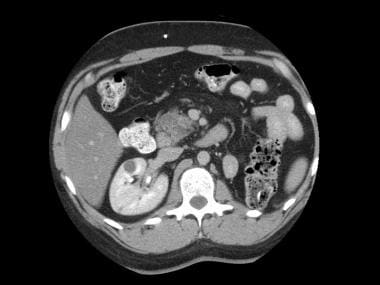
 von Hippel-Lindau syndrome. Axial CT scan through the abdomen shows soft-tissue retroperitoneal masses.
von Hippel-Lindau syndrome. Axial CT scan through the abdomen shows soft-tissue retroperitoneal masses.
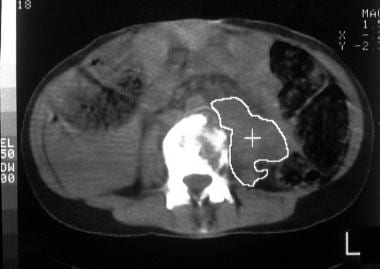 von Hippel-Lindau syndrome. Axial CT scan through the abdomen shows bone destruction. The histologic diagnosis was von Hippel-Lindau–associated malignant pheochromocytoma with extensive metastases (same patient as in the previous image).
von Hippel-Lindau syndrome. Axial CT scan through the abdomen shows bone destruction. The histologic diagnosis was von Hippel-Lindau–associated malignant pheochromocytoma with extensive metastases (same patient as in the previous image).
 von Hippel-Lindau syndrome. This 46-year-old man with known von Hippel-Lindau syndrome presented with gross hematuria. Intravenous urogram and sonogram showed a mass lesion within the midpoles/upper pole of the right kidney. CT was performed for further staging. Contrast-enhanced axial CT scan through the kidneys shows a hypoattenuating mass in the right kidney extending into the renal pelvis.
von Hippel-Lindau syndrome. This 46-year-old man with known von Hippel-Lindau syndrome presented with gross hematuria. Intravenous urogram and sonogram showed a mass lesion within the midpoles/upper pole of the right kidney. CT was performed for further staging. Contrast-enhanced axial CT scan through the kidneys shows a hypoattenuating mass in the right kidney extending into the renal pelvis.
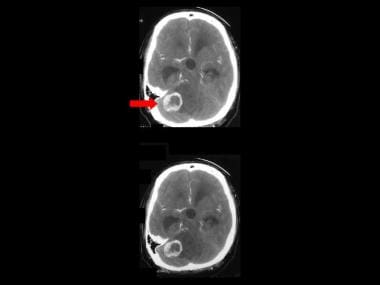 von Hippel-Lindau syndrome. Transaxial contrast-enhanced CT scans through the cerebellum on a 28-year-old patient with no family history of VHL. Scans show a right cerebellar enhancing partially cystic lesion with enhancing mural nodules (due to cerebellar hemangioblastoma (Note the secondary hydrocephalus)
von Hippel-Lindau syndrome. Transaxial contrast-enhanced CT scans through the cerebellum on a 28-year-old patient with no family history of VHL. Scans show a right cerebellar enhancing partially cystic lesion with enhancing mural nodules (due to cerebellar hemangioblastoma (Note the secondary hydrocephalus)
 von Hippel-Lindau syndrome. Transaxial contrast-enhanced CT scans through the cerebellum in the same patient as in the previous image (lower sections). Scans show multiple right cerebellar enhancing partially cystic lesion due to cerebellar hemangioblastoma.
von Hippel-Lindau syndrome. Transaxial contrast-enhanced CT scans through the cerebellum in the same patient as in the previous image (lower sections). Scans show multiple right cerebellar enhancing partially cystic lesion due to cerebellar hemangioblastoma.
 von Hippel-Lindau syndrome. Sagittal reconstruction of contrast-enhanced CT scans (same patient as in the previous 2 images). Scans show a posterior fossa mass a due to cerebellar hemangioblastoma.
von Hippel-Lindau syndrome. Sagittal reconstruction of contrast-enhanced CT scans (same patient as in the previous 2 images). Scans show a posterior fossa mass a due to cerebellar hemangioblastoma.
 von Hippel-Lindau syndrome. Sagittal volume rendering of contrast enhanced CT scan of the same patient as in the previous 3 images shows 2 intensely enhancing lesions in the posterior fossa with arterial supply derived from the posterior fossa circulation.
von Hippel-Lindau syndrome. Sagittal volume rendering of contrast enhanced CT scan of the same patient as in the previous 3 images shows 2 intensely enhancing lesions in the posterior fossa with arterial supply derived from the posterior fossa circulation.
 von Hippel-Lindau syndrome. Axial volume rendering of contrast enhanced CT scan (same patient in Images 18-40) shows 2 intensely enhancing lesions in the posterior fossa with arterial supply derived from the posterior fossa circulation.
von Hippel-Lindau syndrome. Axial volume rendering of contrast enhanced CT scan (same patient in Images 18-40) shows 2 intensely enhancing lesions in the posterior fossa with arterial supply derived from the posterior fossa circulation.
 von Hippel-Lindau syndrome. Axial contrast enhanced axial CT in the portal venous phase at the renal level. The scan was performed as a part of surveillance 12 months following surgery for cerebellar hemangioblastoma. The scan shows multiple pancreatic cysts, a small right renal cyst, and a solid 4.5 cm mass, mid pole left kidney, encroaching on the renal pelvis. A left nephrectomy was performed. Pathological diagnosis was that of a renal cell carcinoma.
von Hippel-Lindau syndrome. Axial contrast enhanced axial CT in the portal venous phase at the renal level. The scan was performed as a part of surveillance 12 months following surgery for cerebellar hemangioblastoma. The scan shows multiple pancreatic cysts, a small right renal cyst, and a solid 4.5 cm mass, mid pole left kidney, encroaching on the renal pelvis. A left nephrectomy was performed. Pathological diagnosis was that of a renal cell carcinoma.
 von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous image) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous image) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
 von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 2 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 2 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
 von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient in the previous 3 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient in the previous 3 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
 von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 4 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex [red arrow]). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize (blue area). The patient is awaiting a partial nephrectomy.
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 4 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex [red arrow]). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize (blue area). The patient is awaiting a partial nephrectomy.
 von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 5 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole right kidney posterior renal cortex). A smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 5 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole right kidney posterior renal cortex). A smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
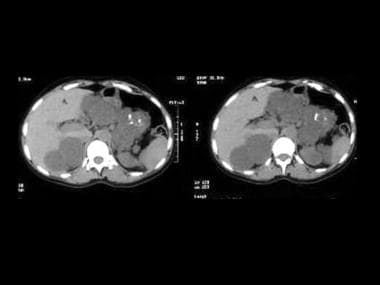 Axial upper abdominal CT scans unenhanced and enhanced show multiple small cysts within the pancreas and larger renal cysts. There are 2 enhancing lesions suggestive of microcystic adenomas.
Axial upper abdominal CT scans unenhanced and enhanced show multiple small cysts within the pancreas and larger renal cysts. There are 2 enhancing lesions suggestive of microcystic adenomas.
Degree of confidence
CT findings are not reliable in differentiating cystic renal cell carcinomas, cancers within a cyst, and atypical cysts. Differentiating a renal cell adenoma from a renal cell carcinoma is impossible.
Patients with VHL syndrome undergo frequent imaging for follow up of renal cell carcinoma. The use of liver windows settings improves the detection of small renal cell carcinomas on the unenhanced CT in VHL syndrome. [8]
The differential diagnosis of VHL should include sporadic hemangioblastoma, cystic astrocytoma, arachnoid cyst, cystic metastases, renal adenoma, renal cell carcinoma, renal cysts, pancreatic islet cell tumors, [3] and MEN 2. Tumors of the endolymphatic sac may mimic other cerebellopontine tumors.
Magnetic Resonance Imaging
MRI is the modality of choice for imaging the central nervous system in patients in whom hemangioblastoma is suggested and for screening asymptomatic patients with VHL and their relatives at risk for VHL.
Hemangioblastomas occur throughout the CNS, but they have several favored locations, including the cerebellum (most common site), medulla, spinal cord, and retina. Although hemangioblastomas can occur as isolated tumors, retinal tumors are mostly confined to VHL. [24, 22, 23, 10] MRI appearances of a hemangioblastoma are those of a well-demarcated cystic lesion with a highly vascular mural nodule that abuts on the pia mater.
Appearances of the cystic component vary depending on the protein concentration and/or presence of hemorrhage within the cyst. The cystic component may be isointense relative to cerebrospinal fluid (CSF) on images obtained with all pulse sequences, but more often, it is slightly hyperintense relative to CSF on T1- and T2-weighted images.
Mural nodules are slightly hypointense on T1-weighted images and hyperintense on T2-weighted images, and they are avidly enhancing after the administration of contrast material.
Large feeding or draining vessels are often present at the periphery and within the solid component, and they may show tubular areas of flow void on spin-echo images.
Although the lesion is benign, it may resemble malignant lesions on advanced MR images. It may have elevated relative tumor blood volume on perfusion MR. Similarly, it may show elevated choline on MR spectroscopy.
Endolymphatic sac tumors are heterogeneous on both T1- and T2-weighted images. They are associated with focal high signal intensity on T1-weighted images due to subacute hemorrhage and with areas of low signal intensity due to calcification or hemosiderin. Blood and protein-filled cysts have high signal intensity on both T1-weighted and T2-weighted images; a finding of these cysts may suggest the diagnosis. Tumors larger than 2 cm may have flow voids. After the administration of contrast material, the tumor enhances heterogeneously.
On MRIs, choroidal capillary hemangiomas associated with VHL are minimally hyperintense on T1-weighted images. They may mimic ocular melanoma, but unlike pigmented melanoma, they are usually hyperintense on T2-weighted images.
As a result of the small size of retinal hemangiomas (1.5-2.0 mm), they are usually not identified on MRIs.
Spinal hemangioblastomas are intramedullary tumors in most patients (75%), but they may be radicular (20%) or intradural extramedullary (5%). Most of these tumors are located in the cervicothoracic spine. They usually expand the cord and have an intratumoral cystic component. On MRIs, they appear as a well-demarcated gadolinium-enhancing mass. Spinal hemangioblastomas are an unusual cause of cryptic subarachnoid hemorrhage. Patients with subarachnoid hemorrhage with negative cerebral angiography may benefit from contrast-enhanced spinal MRI to rule out an occult spinal hemangioblastoma.
An intramural nodule that enhances intensely may be visible. Large dorsally placed draining veins may appear as curvilinear areas of signal void. A syrinx is a frequently associated finding.
A pheochromocytoma associated with VHL has MRI appearances no different from those of the sporadic form. The tumor appears isointense or slightly hypointense relative to the liver on T1-weighted images, and it is extremely hyperintense on T2-weighted images.
(Magnetic resonance images of von Hippel-Lindau syndrome are depicted below.)
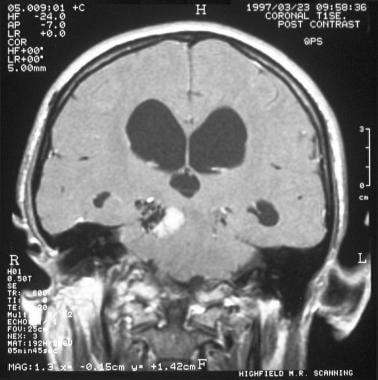 von Hippel-Lindau syndrome. Coronal T1-weighted MRI shows an enhancing lesion in the right cerebellar hemisphere compressing and displacing the aqueduct and fourth ventricle to the left. Note the tubular areas of flow void resulting from large blood vessels and the cystic tumor component.
von Hippel-Lindau syndrome. Coronal T1-weighted MRI shows an enhancing lesion in the right cerebellar hemisphere compressing and displacing the aqueduct and fourth ventricle to the left. Note the tubular areas of flow void resulting from large blood vessels and the cystic tumor component.
 von Hippel-Lindau syndrome. Coronal T1-weighted MRI (same patient as in the previous image) shows an enhancing lesion in the right cerebral hemisphere that compresses and displaces the aqueduct and fourth ventricle to the left. Note the tubular areas of flow void resulting from large blood vessels.
von Hippel-Lindau syndrome. Coronal T1-weighted MRI (same patient as in the previous image) shows an enhancing lesion in the right cerebral hemisphere that compresses and displaces the aqueduct and fourth ventricle to the left. Note the tubular areas of flow void resulting from large blood vessels.
 von Hippel-Lindau syndrome. Oblique coronal T1-weighted gadolinium-enhanced MRI through the right kidney shows a hypointense linear mass extending from the renal capsule to the renal pelvis. At surgery, a renal cell carcinoma was confirmed.
von Hippel-Lindau syndrome. Oblique coronal T1-weighted gadolinium-enhanced MRI through the right kidney shows a hypointense linear mass extending from the renal capsule to the renal pelvis. At surgery, a renal cell carcinoma was confirmed.
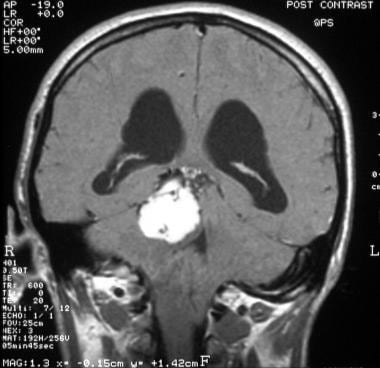
 von Hippel-Lindau syndrome. Coronal T1-weighted contrast enhanced MRI shows an intensely enhancing cerebellar lesion (red arrow) with a large cystic tumor component (white arrow).
von Hippel-Lindau syndrome. Coronal T1-weighted contrast enhanced MRI shows an intensely enhancing cerebellar lesion (red arrow) with a large cystic tumor component (white arrow).
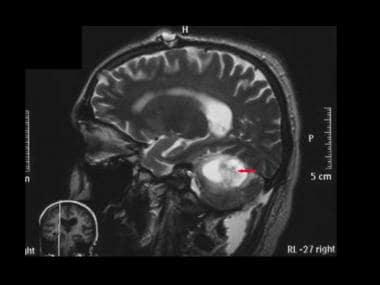
 von Hippel-Lindau syndrome. Coronal T1-weighted contrast enhanced MRI (same patient as in the previous image) shows, at lower sections, an intensely enhancing cerebellar lesion with a large cystic tumor component. Note also the enhancing mural nodules and intratumoral flow void due to large pathological vessels.
von Hippel-Lindau syndrome. Coronal T1-weighted contrast enhanced MRI (same patient as in the previous image) shows, at lower sections, an intensely enhancing cerebellar lesion with a large cystic tumor component. Note also the enhancing mural nodules and intratumoral flow void due to large pathological vessels.
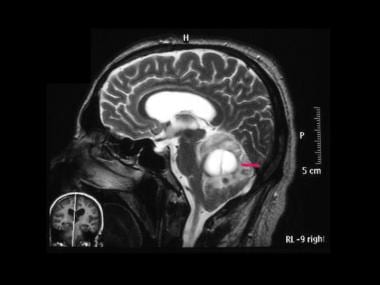 von Hippel-Lindau syndrome. Sagittal T2-weighted MRI (same patient as in the previous 2 images) shows a cerebellar lesion with a large septate cystic component (arrow). Note the hydrocephalus.
von Hippel-Lindau syndrome. Sagittal T2-weighted MRI (same patient as in the previous 2 images) shows a cerebellar lesion with a large septate cystic component (arrow). Note the hydrocephalus.
 von Hippel-Lindau syndrome. Sagittal T2-weighted MRI (same patient as in the previous 3 images) shows a cerebellar lesion with a central low signal component related to intratumoral hemorrhage.
von Hippel-Lindau syndrome. Sagittal T2-weighted MRI (same patient as in the previous 3 images) shows a cerebellar lesion with a central low signal component related to intratumoral hemorrhage.
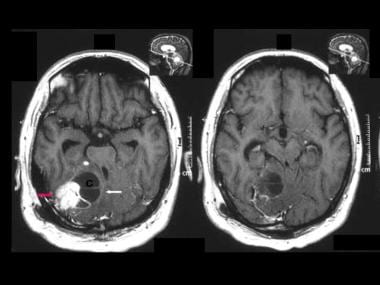
 von Hippel-Lindau syndrome. Axial T2-weighted MRI shows high signal nodules in the region of previous surgical resection of hemangioblastoma in an 18-month surveillance scan. An earlier scan showed no nodular lesions in this region. The appearance suggests a recurrence of hemangioma.
von Hippel-Lindau syndrome. Axial T2-weighted MRI shows high signal nodules in the region of previous surgical resection of hemangioblastoma in an 18-month surveillance scan. An earlier scan showed no nodular lesions in this region. The appearance suggests a recurrence of hemangioma.
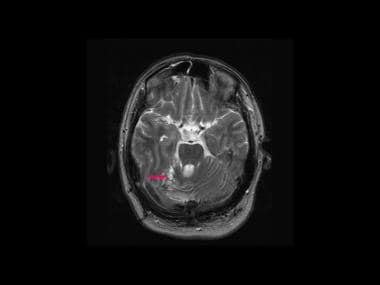 von Hippel-Lindau syndrome. Axial T2-weighted MRI (same patient as in the previous image) shows high signal nodules in the region of previous surgical resection of hemangioblastoma in an 18-month surveillance scan. An earlier scan showed no nodular lesions in this region. The appearance suggests a recurrence of hemangioma.
von Hippel-Lindau syndrome. Axial T2-weighted MRI (same patient as in the previous image) shows high signal nodules in the region of previous surgical resection of hemangioblastoma in an 18-month surveillance scan. An earlier scan showed no nodular lesions in this region. The appearance suggests a recurrence of hemangioma.
Gadolinium
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. Characteristics of NSF/NFD include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
False positives/negatives
False-positive diagnoses may occur with cystic astrocytomas, which are usually smaller than 5 cm in diameter; these may be calcified, and they usually have thicker walls. Cystic metastases occasionally resemble a hemangioblastoma superficially. Spinal hemangioblastomas must be differentiated from intramedullary hemorrhage.
Endolymphatic sac tumors may mimic other cerebellopontine tumors. Nonfunctioning adrenal adenomas, adrenocortical adenomas, and adrenal cysts must be differentiated from pheochromocytomas associated with VHL.
Ultrasonography
The sensitivity of ultrasonography in the detection of the primary lesion in renal cell carcinoma is comparable to that of CT. Ultrasonography is the modality of choice in screening the abdomen in patients with known VHL. This is a useful examination for imaging the retina; sonograms may show small hypoechoic masses, most often in the temporal retina. [23]
Ultrasonography is an excellent modality for screening the abdomen in patients with known VHL or their at-risk relatives. It has a high sensitivity in depicting cystic intra-abdominal masses and in characterizing the contents of cysts.
Differentiating a renal cell adenoma from a renal cell carcinoma may not be possible. Similarly, difficulties may be encountered in differentiating a complex benign cyst from cystic malignant transformation.
Nuclear Imaging
Radionuclide studies are increasingly valuable in diagnosing CNS neoplasms, in monitoring therapy, and in defining functional characteristics that are not demonstrated well on conventional cross-sectional images. [23, 12]
Much of the present value of nuclear medicine is in positron emission tomography (PET). PET with fluorodeoxyglucose (FDG) provides an indication of metabolic activity of CNS tumors; this finding is well correlated with the tumor growth rate in most tumors. However, this correlation may not be applicable to some tumors such as pilocytic astrocytomas and hemangioblastomas, which are histologically benign but may resemble high-grade lesions on FDG-PET.
FDG-PET scans are unaffected by postoperative reactions or steroids, and they can provide information about residual tumor or tumor recurrence. Many centers prefer to use perfusion MR/CT instead of PET for essentially the same purpose.
Kulkarni et al have reported an incidental detection of clinically occult pancreatic malignancy on FDG-PET in a patient with VHL syndrome who underwent restaging for a previously treated endolymphatic sac tumor (ELST). [9]
Radionuclides can also be used (1) to detect bone metastases resulting from primary malignant bone lesions due to malignancies associated with VHL and (2) to assess renal function prior to resection of renal tumors. Iodine-131 metaiodobenzylguanidine (131I MIBG) is a useful scanning agent in the detection of pheochromocytoma. This technique is particularly useful when clear clinical and laboratory evidence of tumor exists but when CT scans and MRIs demonstrate no abnormality. [26]
Iodine-131 MIBG can be used for whole-body scintigraphy in which functioning metastasis from a malignant pheochromocytoma may also be detected; this approach may provide the future therapeutic options (eg,131I MIBG methods to treat metastases).
Iodine-131 MIBG uptake has a sensitivity of 80-90% and a specificity of 98% in the detection of pheochromocytoma. Uptake may occur in medullary carcinoma of the thyroid, carcinoid tumors, neuroblastoma, and paragangliomas.
(Scintigraphic images of VHL are shown below.)
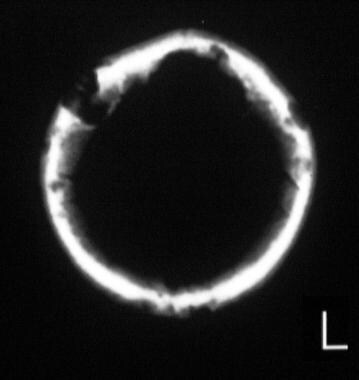
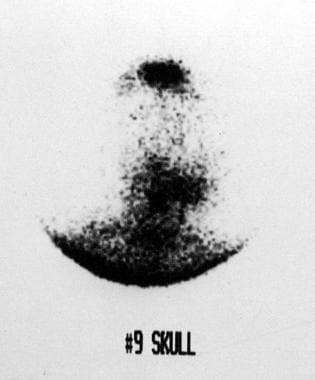 von Hippel-Lindau syndrome. Scintigraphic image of the skull after iodine-131 metaiodobenzylguanidine administration shows multiple foci of isotope uptake.
von Hippel-Lindau syndrome. Scintigraphic image of the skull after iodine-131 metaiodobenzylguanidine administration shows multiple foci of isotope uptake.
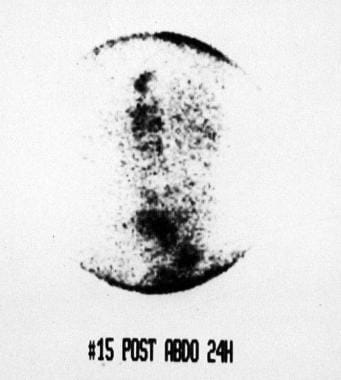 von Hippel-Lindau syndrome. Scintigraphic image of the retroperitoneum (same patient as in the previous image) after iodine-131 metaiodobenzylguanidine administration shows multiple foci of isotope uptake.
von Hippel-Lindau syndrome. Scintigraphic image of the retroperitoneum (same patient as in the previous image) after iodine-131 metaiodobenzylguanidine administration shows multiple foci of isotope uptake.
In a study of patients with VHL by Shell et al, gallium-68-DOTATATE PET/CT detected a total of 206 lesions, CT detected 208 lesions, and MRI detected 94 lesions in 61, 66, and 33 scans, respectively. Gallium-68-DOTATATE PET/CT (3.4 ± 0.1 per scan) was superior than CT (3.2 ± 0.1 per scan, P=0.02), with similar results when compared with MRI (2.8 ± 0.1 per scan, P=0.03) in detecting lesions in any anatomic locations. [27]
In a prospective study of patients with von Hippel-Lindau syndrome, Prasad et al found that 68Ga-DOTATOC PET/CT had a high sensitivity for the diagnosis and staging of neuroendocrine tumors. Neuroendocrine tumors of the pancreas occur in 8-17% of patients with von Hippel-Lindau disease, and 11-20% progress to metastatic disease. [28]
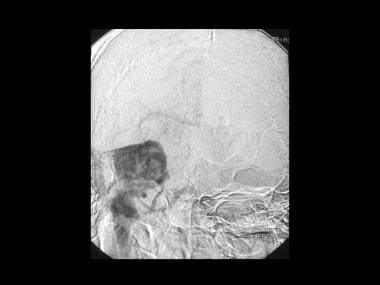
Angiography
Angiography of hemangioblastoma reveals a hypervascular lesion with intense and prolonged early enhancement of the mural nodule associated with dilated feeding vessels. Endolymphatic sac tumors are hypervascular on angiography, and the blood supply is derived from the external carotid artery. Large tumors have an additional blood supply from the internal carotid artery and posterior circulation.
Angiographic appearances are nonspecific and can occur with other vascular tumors. Cystic meningioma and a meningeal hemangiopericytoma may resemble a hemangioblastoma superficially, but confusion is unlikely when the clinical presentation and the other imaging findings are considered.
(See the images below.)
 von Hippel-Lindau syndrome. Sagittal vertebral angiogram shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
von Hippel-Lindau syndrome. Sagittal vertebral angiogram shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
 von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous image) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous image) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
 von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 2 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 2 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
 von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 3 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 3 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
 von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 4 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 4 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
 von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 5 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 5 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
Retinal hemangioblastomas are characteristic of VHL, and some studies have shown good results with fundus fluorescein angiography (FFA) features of retinal hemangioblastomas using ultra-widefield (UWF) imaging. [29, 30]
-
von Hippel-Lindau syndrome. Transaxial nonenhanced and contrast-enhanced CT scans through the cerebellum in a 34-year-old patient with a family history of VHL. Scans show a midline cerebellar cystic lesion with an enhancing nodule (arrow) due to cerebellar hemangioblastoma.
-
von Hippel-Lindau syndrome. T1-weighted transaxial gadolinium-enhanced MRIs of the same patient as in the previous image show a well-defined hypervascular enhancing mass.
-
von Hippel-Lindau syndrome. Coronal vertebral angiogram of the same patient as in the previous 2 images shows a hypervascular intramural nodule that demonstrates a prolonged and intense enhancement with a surrounding avascular area, which represents the cyst surrounding the mural nodule. Note the stretching around the cyst.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram of the same patient as in the previous 3 images shows a hypervascular intramural nodule (open arrow) that demonstrates a prolonged and intense enhancement with a surrounding avascular area, representing the cyst surrounding the mural nodule (solid arrows). Note the stretching of vessels around the cyst. The final diagnosis was a cerebellar hemangioblastoma associated with von Hippel-Lindau syndrome (same patient as in Images 1-3).
-
von Hippel-Lindau syndrome. Axial nonenhanced CT scan of the head in a patient with known von Hippel-Lindau syndrome and an acute neurologic presentation shows hyperattenuating areas within a right cerebellar tumor suggestive of hemorrhage. Note that the tumor is causing moderate hydrocephalus.
-
von Hippel-Lindau syndrome. Coronal T1-weighted MRI shows an enhancing lesion in the right cerebellar hemisphere compressing and displacing the aqueduct and fourth ventricle to the left. Note the tubular areas of flow void resulting from large blood vessels and the cystic tumor component.
-
von Hippel-Lindau syndrome. Coronal T1-weighted MRI (same patient as in the previous image) shows an enhancing lesion in the right cerebral hemisphere that compresses and displaces the aqueduct and fourth ventricle to the left. Note the tubular areas of flow void resulting from large blood vessels.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram shows a hypervascular lesion with intense and prolonged enhancement.
-
von Hippel-Lindau syndrome. Coronal vertebral angiogram shows a hypervascular lesion with intense and prolonged enhancement. The final diagnosis was von Hippel-Lindau syndrome–associated cerebellar hemangioblastoma (same patient as in the previous image).
-
von Hippel-Lindau syndrome. A 16-year-old female adolescent with a family history of von Hippel-Lindau syndrome presented with generalized bone pain, weight loss, and hypertension. This skull radiograph was part of the skeletal survey. The lateral skull radiograph demonstrates well-defined lytic lesions throughout the calvarium.
-
von Hippel-Lindau syndrome. Transaxial bone-window CT scan through the head shows destructive lesions throughout the calvarium. Some lesions cross the entire thickness of the skull.
-
von Hippel-Lindau syndrome. Scintigraphic image of the skull after iodine-131 metaiodobenzylguanidine administration shows multiple foci of isotope uptake.
-
von Hippel-Lindau syndrome. Scintigraphic image of the retroperitoneum (same patient as in the previous image) after iodine-131 metaiodobenzylguanidine administration shows multiple foci of isotope uptake.
-
von Hippel-Lindau syndrome. Axial CT scan through the abdomen shows soft-tissue retroperitoneal masses.
-
von Hippel-Lindau syndrome. Axial CT scan through the abdomen shows bone destruction. The histologic diagnosis was von Hippel-Lindau–associated malignant pheochromocytoma with extensive metastases (same patient as in the previous image).
-
von Hippel-Lindau syndrome. This 46-year-old man with known von Hippel-Lindau syndrome presented with gross hematuria. Intravenous urogram and sonogram showed a mass lesion within the midpoles/upper pole of the right kidney. CT was performed for further staging. Contrast-enhanced axial CT scan through the kidneys shows a hypoattenuating mass in the right kidney extending into the renal pelvis.
-
von Hippel-Lindau syndrome. Oblique coronal T1-weighted gadolinium-enhanced MRI through the right kidney shows a hypointense linear mass extending from the renal capsule to the renal pelvis. At surgery, a renal cell carcinoma was confirmed.
-
von Hippel-Lindau syndrome. Transaxial contrast-enhanced CT scans through the cerebellum on a 28-year-old patient with no family history of VHL. Scans show a right cerebellar enhancing partially cystic lesion with enhancing mural nodules (due to cerebellar hemangioblastoma (Note the secondary hydrocephalus)
-
von Hippel-Lindau syndrome. Transaxial contrast-enhanced CT scans through the cerebellum in the same patient as in the previous image (lower sections). Scans show multiple right cerebellar enhancing partially cystic lesion due to cerebellar hemangioblastoma.
-
von Hippel-Lindau syndrome. Sagittal reconstruction of contrast-enhanced CT scans (same patient as in the previous 2 images). Scans show a posterior fossa mass a due to cerebellar hemangioblastoma.
-
von Hippel-Lindau syndrome. Sagittal volume rendering of contrast enhanced CT scan of the same patient as in the previous 3 images shows 2 intensely enhancing lesions in the posterior fossa with arterial supply derived from the posterior fossa circulation.
-
von Hippel-Lindau syndrome. Axial volume rendering of contrast enhanced CT scan (same patient in Images 18-40) shows 2 intensely enhancing lesions in the posterior fossa with arterial supply derived from the posterior fossa circulation.
-
von Hippel-Lindau syndrome. Coronal T1-weighted contrast enhanced MRI shows an intensely enhancing cerebellar lesion (red arrow) with a large cystic tumor component (white arrow).
-
von Hippel-Lindau syndrome. Coronal T1-weighted contrast enhanced MRI (same patient as in the previous image) shows, at lower sections, an intensely enhancing cerebellar lesion with a large cystic tumor component. Note also the enhancing mural nodules and intratumoral flow void due to large pathological vessels.
-
von Hippel-Lindau syndrome. Sagittal T2-weighted MRI (same patient as in the previous 2 images) shows a cerebellar lesion with a large septate cystic component (arrow). Note the hydrocephalus.
-
von Hippel-Lindau syndrome. Sagittal T2-weighted MRI (same patient as in the previous 3 images) shows a cerebellar lesion with a central low signal component related to intratumoral hemorrhage.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous image) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 2 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 3 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 4 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
-
von Hippel-Lindau syndrome. Sagittal vertebral angiogram (same patient as in the previous 5 images) shows a hypervascular lesion with intense and prolonged enhancement with an avascular cystic component. Note the large draining vein.
-
von Hippel-Lindau syndrome. Axial contrast enhanced axial CT in the portal venous phase at the renal level. The scan was performed as a part of surveillance 12 months following surgery for cerebellar hemangioblastoma. The scan shows multiple pancreatic cysts, a small right renal cyst, and a solid 4.5 cm mass, mid pole left kidney, encroaching on the renal pelvis. A left nephrectomy was performed. Pathological diagnosis was that of a renal cell carcinoma.
-
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous image) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
-
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 2 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
-
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient in the previous 3 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
-
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 4 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole, right kidney, posterior renal cortex [red arrow]). A further smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize (blue area). The patient is awaiting a partial nephrectomy.
-
von Hippel-Lindau syndrome. Axial contrast enhanced upper abdominal CT scans (same patient as in the previous 5 images) in the portal venous phase. These scans were performed 6 months following left nephrectomy. Note cysts within the pancreas and the right kidney. Note also a solid 3 cm lesion (mid pole right kidney posterior renal cortex). A smaller lesion is seen in the renal cortex more anteriorly, which is too small to characterize. The patient is awaiting a partial nephrectomy.
-
von Hippel-Lindau syndrome. Axial T2-weighted MRI shows high signal nodules in the region of previous surgical resection of hemangioblastoma in an 18-month surveillance scan. An earlier scan showed no nodular lesions in this region. The appearance suggests a recurrence of hemangioma.
-
von Hippel-Lindau syndrome. Axial T2-weighted MRI (same patient as in the previous image) shows high signal nodules in the region of previous surgical resection of hemangioblastoma in an 18-month surveillance scan. An earlier scan showed no nodular lesions in this region. The appearance suggests a recurrence of hemangioma.
-
Axial upper abdominal CT scans unenhanced and enhanced show multiple small cysts within the pancreas and larger renal cysts. There are 2 enhancing lesions suggestive of microcystic adenomas.
-
Axial upper abdominal CT scans unenhanced (same patient as in the previous image) and enhanced show multiple small cysts within the pancreas and larger renal cysts. There are 2 enhancing lesions suggestive of microcystic adenomas.







