Practice Essentials
A ventricular septal defect (VSD) is a defect in the interventricular septum, which is composed of muscular and membranous segments. The clinical presentation of patients with a ventricular septal defect varies according to the size of the defect and the pulmonary blood flow and pressure. [1, 2, 3, 4] [5] VSDs are classified into 3 main categories according to their location and the appearance of the margins of defects. The clinical significance of the VSD depends on its size and location, the level of pulmonary pressure, and the left ventricular (LV) outflow resistance associated with the VSD. A restrictive VSD produces a small shunt and does not cause significant hemodynamic derangement. In contrast, a large VSD may progressively lead to higher pulmonary resistance and, finally, to irreversible pulmonary vascular changes, producing the so-called Eisenmenger syndrome (reversal of shunt to right-to-left shunt). [6, 7, 8]
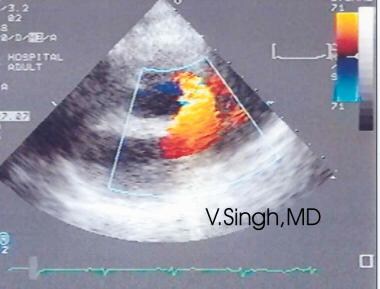
Clinically, VSDs produce a characteristic systolic murmur and are associated with recurrent upper respiratory infections. The anatomic localization of all VSDs is facilitated by using 2-dimensional (2D) echocardiographic images with a Doppler system and by superimposing a color-coded direction and velocity of blood flow on the real-time images. Clinically significant VSDs require surgical correction; clinical outcomes are usually excellent.
VSD, demonstrated in the image below, is the second most common cardiac malformation, accounting for approximately one fifth of all congenital cardiac anomalies. It is usually diagnosed during childhood. In adults, it is diagnosed less often, because during the patient's early years, large VSDs are corrected surgically, and smaller VSDs close spontaneously.
Echocardiography
Color Doppler transthoracic echocardiography (TTE) is the most valuable tool for diagnosis of VSD because of its high sensitivity, detecting up to 95% of VSDs, especially nonapical lesions larger than 5 mm. Color Doppler TTE provides morphologic information such as size, location, and the number of the defects, as well as hemodynamic information such as jet size, severity, and estimation of pulmonary arterial pressure. [6, 7, 8]
Two-dimensional (2D) and Doppler color-flow mapping may be used to identify the type of defect in the ventricular septum. [9] Perimembranous VSDs are characterized by septal dropout in the area adjacent to the septal leaflet of the tricuspid valve and below the right border of the aortic annulus. [10, 11, 12, 13, 14, 15]
The subaortic or anterior malalignment type of VSD appears just below the posterior semilunar valve cusps, entirely superior to the tricuspid valve. Subpulmonary VSD appears as echo dropout within the outflow septum and extending to the pulmonary annulus. One or two of the aortic cusps may be seen to be protruding through the defect into the right ventricular outflow tract. The inlet AV septal-type of VSD extends from the fibrous annulus of the tricuspid valve into the muscular septum; it is often entirely beneath the septal tricuspid leaflet.
Muscular defects may appear anywhere throughout the ventricular septum. They may be either large and single or small and multiple.
The anatomic localization of all VSDs is facilitated by coupling 2D sonograms with a Doppler system and by superimposing a color-coded direction and velocity of blood flow on the real-time images.
The 2D echocardiogram shows the position and size of the ventricular septal defect. Small defects, especially those of the muscular septum, may be difficult to image; they might be visualized only by means of color Doppler examination.
In defects of the membranous septum, a thin membrane may partially cover the defect and limit the volume of the left-to-right shunt. Although the membrane is called a ventricular septal aneurysm, it consists of tricuspid valve tissue.
Chest radiography
In patients with small VSDs, the results of chest radiographs are usually normal. With medium-size VSDs, minimal cardiomegaly and a borderline increase in pulmonary vasculature may be observed. In large VSDs, the chest radiograph shows gross cardiomegaly with prominence of both ventricles, the left atrium, and the pulmonary artery. The pulmonary vascular markings are increased, and frank pulmonary edema, including pleural effusions, may be present.
MRI and CT
Information provided by MRI may also be obtained by means of echocardiography; therefore, the clinical role of MRI is to supplement the information acquired with echocardiography. Morphologic information is provided by ECG-gated spin-echo and cine MRI. Ventricular volumes, mass, and function may be assessed by using cine MRI. The volumes of shunts, valvular function, and pressure gradients across valves and conduits may be estimated by use of velocity-encoded cine MRI (velocity-flow mapping). CT scans may show cardiomegaly, left atrial enlargement, and vascular engorgement. [16, 17]
Electrocardiography
The electrocardiogram (ECG) mirrors the size of the shunt and the degree of pulmonary hypertension. [18]
Small restrictive VSDs usually produce a normal tracing. Medium-sized VSDs produce a broad, notched P wave characteristic of left atrial overload. Signs of LV volume overload — namely, deep Q and tall R waves with tall T waves in leads V5 and V6 — are present. In addition, signs of atrial fibrillation are often present. Large VSDs produce right ventricular hypertrophy with right-axis deviation. With further progression, the ECG shows biventricular hypertrophy; P waves may be notched or peaked.
Radiography
The chest radiograph reflects the magnitude of the shunt as well as the degree of pulmonary hypertension. A shunt of moderate size causes signs of left atrial, right ventricular, and LV dilation, with some pulmonary overcirculation. Over time, a large shunt produces pulmonary hypertension in association with enlarged central pulmonary arteries, peripheral pruning, and Eisenmenger physiology. With these developments, the enlarged cardiac chamber may normalize.
VSD is usually diagnosed in children. In infants, the examining physician usually suspects the diagnosis because of a harsh systolic murmur at the lower left sternal border. The ECG and chest radiographic findings are within normal limits in the immediate neonatal period because appreciable left-to-right shunting occurs only after pulmonary vascular resistance decreases as the pulmonary vessels lose their fetal characteristics.
After the first year of life, a variable clinical picture emerges in children with VSD. If a small defect is present, the child is usually asymptomatic, the ECG usually appears normal, and the chest radiograph shows normal or mildly increased pulmonary vascular markings.
The ECG reveals left ventricular hypertrophy or combined ventricular hypertrophy, and the chest radiograph and CT scan show cardiomegaly, left atrial enlargement, and vascular engorgement.
Computed Tomography
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) has multiple capabilities in the evaluation of congenital heart disease. Morphologic information is provided by ECG-gated spin-echo and cine MRI. Ventricular volumes, mass, and function may be assessed by using cine MRI. The volumes of shunts, valvular function, and pressure gradients across valves and conduits may be estimated by use of velocity-encoded cine MRI (velocity-flow mapping).
However, information provided by MRI may also be obtained by means of echocardiography, the equipment for which is more portable. Consequently, the current clinical role of MRI is to supplement the information acquired with echocardiography.
Reports from several centers indicate the effectiveness of MRI for the evaluation of children and adults with congenital heart disease. [19] In several studies in which the results of MRI were corroborated with those of angiography and/or 2D echocardiography, an accurate anatomic diagnosis of anomalies was achieved with MRI in more than 90% of patients.
MRI has also shown substantial utility in the anatomic and functional evaluation of congenital heart disease after palliative and total correction. The visceroatrial situs, the type of ventricular loop, and the relationship of the great vessels may be identified in all patients in whom studies encompassing the entire heart are performed.
The diagnostic accuracy of MRI exceeds 90% for abnormalities of arterioventricular connections; for great vessel anomalies, such as coarctation and vascular rings; for ventricular and atrial septal defects; and for abnormalities of venous connections. [20, 21, 22, 23, 24, 17]
False-positive and false-negative results associated with VSD are uncommon with MRI.
Ultrasonography
Doppler color-flow and 2D mapping may be used to identify the type of defect in the ventricular septum. Perimembranous VSDs are observed as septal dropout in the area adjacent to the septal leaflet of the tricuspid valve and below the right border of the aortic annulus. (See the image below.) [14, 15]
The subaortic or anterior malalignment type of VSD appears just below the posterior semilunar valve cusps, entirely superior to the tricuspid valve. Subpulmonary VSD appears as echo dropout within the outflow septum and extending to the pulmonary annulus. One or two of the aortic cusps may be seen to be protruding through the defect into the right ventricular outflow tract. The inlet AV septal-type of VSD extends from the fibrous annulus of the tricuspid valve into the muscular septum; it is often entirely beneath the septal tricuspid leaflet.
Muscular defects may appear anywhere throughout the ventricular septum. They may be either large and single or small and multiple.
The anatomic localization of all VSDs is facilitated by coupling 2D images with a Doppler system and by superimposing a color-coded direction and velocity of blood flow on the real-time images. [10, 25, 11, 26, 27, 28, 29, 12, 13]
The degree of confidence in echocardiography is high, and false-positive and false-negative results are rare.
Angiography
The hemodynamics of a VSD may be demonstrated by means of cardiac catheterization.
Catheterization is usually performed only under the following conditions: (1) uncertainty remains regarding the size of the shunt, following a comprehensive clinical evaluation; (2) laboratory data do not fit well with the clinical findings; or (3) pulmonary vascular disease is suspected.
Oximetry demonstrates an increase in oxygen content in the right ventricle, because with some defects, blood is ejected almost directly into the pulmonary artery (a phenomenon known as streaming). This increase is occasionally apparent only when pulmonary arterial blood is sampled.
Small, restrictive VSDs are associated with normal right-sided heart pressures and pulmonary vascular resistance. Large, nonrestrictive VSDs are associated with equal or near-equal pulmonary and systemic systolic pressures. Pulmonary blood flow may be 2-4 times greater than systemic blood flow. In patients with large, nonrestrictive VSDs who have hyperdynamic pulmonary hypertension, the pulmonary vascular resistance is only minimally elevated (pulmonary vascular resistance is equal to the pressure divided by the flow).
If Eisenmenger syndrome is present, pulmonary artery systolic and diastolic pressures are elevated, the degree of left-to-right shunting is minimal, and desaturation of blood in the LV is encountered. The size, location, and number of ventricular defects are demonstrated by left ventriculography. Contrast medium passes across the defect or defects to opacify the right ventricle and the pulmonary artery.
The degree of confidence for angiography is high in VSD, and false-positive and false-negative results are rare.
-
Ventricular septal defect (VSD) as seen by means of color Doppler echocardiography.