Practice Essentials
Tuberous sclerosis complex (TSC) is an autosomal-dominant disorder. TSC affects cellular degeneration, proliferation, and migration and results in hamartomatous lesions in virtually all organs during early development—most commonly the brain, skin, eyes, heart, kidneys, and lungs. Common features include cortical tubers, subependymal nodules (SENs), subependymal giant cell astrocytomas (SEGAs), facial angiofibromas, hypomelanotic spots known as Fitzpatrick patches (ash-leaf spots), cardiac rhabdomyomas, and renal angiomyolipomas. Approximately 50% of cases are inherited and 50% are sporadic, although the incidence of sporadic cases may be as high as 80%. Penetrance is believed to be high. The expression is variable. The severity of the disease appears to reflect the variable penetrance. Substantial genetic inhomogeneity exists. The disease is caused by mutations in either the TSC1 gene, on chromosome 9q34, or the TSC2 gene, on chromosome 16p13.3. [1, 2, 3, 4, 5, 6, 7]
Imaging procedures include CT or MRI of the brain, renal ultrasonography, and echocardiography. Abnormal radiologic findings are important in diagnosing this disease and include CNS lesions of cortical hamartomas, white-matter abnormalities, and subependymal nodules (ie, hamartomas). Patients also have subependymal giant cell astrocytomas. These intracranial neoplasms can result in obstructive hydrocephalus. Retinal lesions, nonatheromatous vascular stenoses and aneurysms, and mild ventricular enlargement without astrocytomas can be present. [8, 9, 10, 11, 5, 6, 7, 12, 13, 14]
Computed tomography (CT) and magnetic resonance imaging (MRI) of the brain are the most sensitive screening imaging studies. Brain CT or MRI can identify subependymal giant cell astrocytomas (SEGAs) before development of obstructive hydrocephalus and can identify the number of cortical tubers. MRI is considered the modality of choice for the evaluation of the brain in patients with diagnosed or suspected tuberous sclerosis. CT is the modality of choice for evaluating renal lesions because of its ability to delineate cystic from solid lesions and lipid-containing angiomyolipomas. [8, 15, 16, 17, 18, 9, 19, 20, 21, 22]
Fetal ultrasound and MRI imaging techniques may capture the following TSC-associated lesions: cardiac rhabdomyomas, subependymal nodules, cortical tubers and renal cysts. Often these represent an incidental finding during a routine ultrasound. Prenatal suspected cardiac rhabdomyoma should raise the suspicion of TSC. In fetuses with multiple tumors, especially the familial cases, genomic sequencing has a high yield of detecting TSC-causing genes. [10, 19, 20, 21, 22]
CT is much less sensitive than MRI in the identification of cortical hamartomas and neuronal migration streaks. MRI is less sensitive than CT in the identification of calcifications of the brain. CT cannot be used to differentiate non–lipid-containing angiomyolipomas from other renal tumors.
(See the images below.)
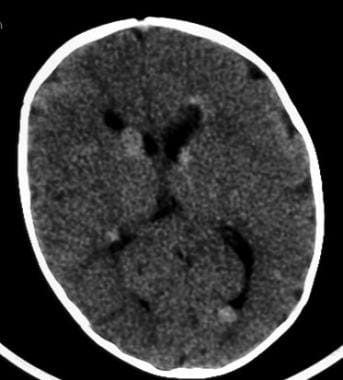
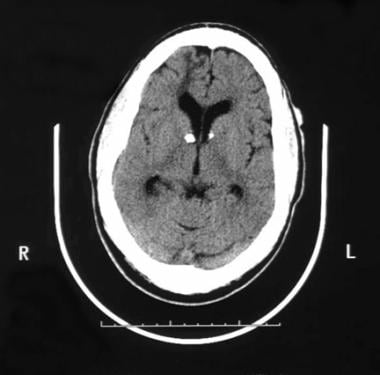 Axial nonenhanced CT image in a patient with tuberous sclerosis reveals subependymal calcifications. A hypointense right frontal lesion represents a white matter lesion or tuber; it extends from the lateral ventricle through the cerebral cortex.
Axial nonenhanced CT image in a patient with tuberous sclerosis reveals subependymal calcifications. A hypointense right frontal lesion represents a white matter lesion or tuber; it extends from the lateral ventricle through the cerebral cortex.
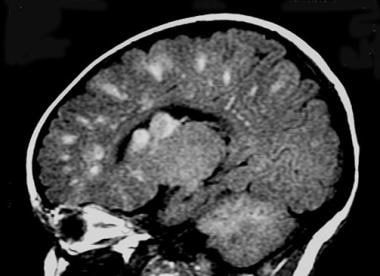 Sagittal T1-weighted MRI in an infant with tuberous sclerosis shows multiple hyperintense cortical and subependymal nodules.
Sagittal T1-weighted MRI in an infant with tuberous sclerosis shows multiple hyperintense cortical and subependymal nodules.
Manifestations of tuberous sclerosis can become apparent in persons of any age, but most patients have clinical symptoms before they are aged 10 years. The classic form of the disease is the triad of seizures, intellectual disability, and adenoma sebaceum, which is a papular facial nevus more accurately termed facial angiofibroma. This classic appearance occurs in less than half of patients, probably in one third.
Tuberous sclerosis is a multisystemic disorder. Non-CNS lesions of tuberous sclerosis include cutaneous manifestations. In addition to the lesions mentioned above, these include vitiligo and subungual patches. The renal abnormalities associated with TSC include angiomyolipoma, cysts, and renal cell carcinoma. [23] Findings also are observed in the heart; lungs; skeleton; and, occasionally, liver, spleen, and pancreas.
If left untreated, nearly 40% of TSC patients die by the age of 35 years, mainly due to renal failure or hemorrhage. [23]
The TOSCA study is a large natural history study encompassing 2093 patients with TSC. In this registry, the median age of diagnosis of TSC was one year (range 0–69). In 5.9% patients, the diagnosis was made prenatally. While cardiac rhabdomyoma were found in 34.3% patients, mean age of diagnosis of cardiac rhabdomyoma was 3.1 years. [24]
Follow-up examinations
Regular follow-up exams should include the following [25, 11, 14] :
-
Brain MRI every 1-3 years in asymptomatic individuals with TSC < 25 years to monitor for new SEGAs.
-
For those with asymptomatic SEGA in childhood, continued periodic imaging in adulthood.
-
For those with large or growing SEGA or SEGA causing ventricular enlargement, more frequent brain MRIs as clinically appropriate.
-
Screening for TSC-associated neuropsychiatric disorder (TAND) at least annually.
-
EEG in individuals with known or suspected seizure activity.
-
MRI of the abdomen every 1-3 years to assess for angiomyolipoma and renal cysts.
-
Assess renal function (glomerular filtration rate and blood pressure) at least annually.
-
Echocardiogram every 1-3 years in asymptomatic infants and children with cardiac rhabdomyomas until regression.
-
In women >18 years or those who report respiratory symptoms, clinical screening for pulmonary lymphangioleiomyomatosis (LAM) symptoms (exertional dyspnea and shortness of breath) at each visit.
-
High-resolution CT (HRCT) every 5-10 years in asymptomatic individuals at risk for lymphangioleiomyomatosis (LAM) (women >18 years) even if there are no signs of LAM on baseline examination.
-
Annual pulmonary function testing and HRCT every 2-3 years for individuals with lung cysts detected by HRCT.
-
Annual dermatologic examination.
-
Dental examination every 6 months.
-
Annual ophthalmology evaluation in those with previously identified ophthalmologic lesions or vision symptoms.
Radiography
Abnormal radiologic findings are important in diagnosing this disease and include CNS lesions of cortical hamartomas, white-matter abnormalities, and subependymal nodules (ie, hamartomas).
Most findings detectable on plain radiographs are musculoskeletal or thoracic. One half of the patients with tuberous sclerosis have musculoskeletal lesions. Changes include osteoporosis and cystic defects in the metacarpals, metatarsals, and/or phalanges. Erosions of the tufts of the distal phalanges, the result of ungual angiofibromas, may be observed. A periosteal reaction is observed in tubular bone; some authors characterize this reaction as having an undulating appearance. Heterogeneous sclerosis can affect the entire axial skeleton. Multiple bone islands with an apparent natural propensity for the diploic space may be observed. Macrodactyly and expansile-enhanced bone density that is restricted to a single rib are described. Plain skull films often reveal sclerosis or widening of the diploic space, which is related to the administration of phenytoin.
Chest radiographs rarely can depict evidence of interstitial fibrosis or honeycombing. Occasionally, the appearance of the chest is compatible with its appearance in lymphangioleiomyomatosis (LAM). The connection between tuberous sclerosis and LAM is unclear. Pneumothorax is an infrequent complication in interstitial fibrosis and LAM. Approximately one fourth of patients can have cardiac rhabdomyomas, which places these patients at risk for congestive heart failure.
Renal angiomyolipomas occur in 50-90% of patients but only rarely contain enough adipose tissue to be observed on plain radiographs. Findings on excretory urograms or retrograde pyelograms can vary widely, depending on the number and size of cysts or angiomyolipomas. These findings include bilateral renal enlargement or distortion of the collecting systems caused by cysts or angiomyolipomas. Hamartomatous polyps can be present in the colon. Gastric polyposis also can occur; this can be depicted on barium studies.
Specificity with respect to plain radiographic findings in patients with tuberous sclerosis is problematic because many of these lesions occur in other conditions; however, conventional radiographic findings often support the diagnosis of tuberous sclerosis.
Degree of confidence
Occasionally, plain radiographs depict lucencies caused by fat in the angiomyolipoma; this finding can suggest the diagnosis of tuberous sclerosis. Distortion of the renal collecting system as a result of multiple cystic lesions may be indistinguishable from findings in autosomal dominant polycystic kidney disease.
Findings on excretory urograms and retrograde pyelograms can include bilateral renal enlargement or distortion of the collecting system; these can mimic the findings in autosomal-dominant polycystic kidney disease.
Computed Tomography
Overall, CT reveals intracranial abnormalities in 85% of patients with tuberous sclerosis. Frequently, CT can depict extracranial manifestations of tuberous sclerosis. CT readily depicts calcified cortical tubers and calcified subependymal nodules; the frequency of their calcification increases with patient age. According to one author, more than 80% of the lesions can become calcified. Cortical tubers are often seen as low-attenuating peripheral lesions on CT scans; these are more easily identified with MRI.
(See the images below.)
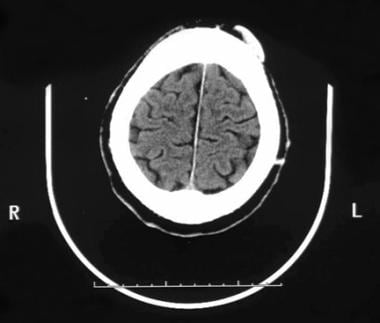
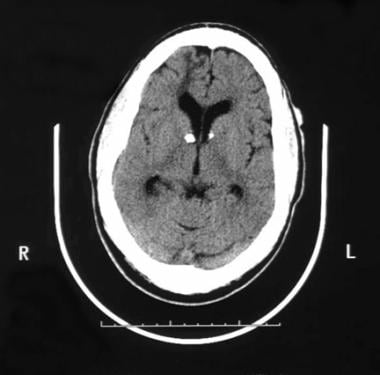 Axial nonenhanced CT image in a patient with tuberous sclerosis reveals subependymal calcifications. A hypointense right frontal lesion represents a white matter lesion or tuber; it extends from the lateral ventricle through the cerebral cortex.
Axial nonenhanced CT image in a patient with tuberous sclerosis reveals subependymal calcifications. A hypointense right frontal lesion represents a white matter lesion or tuber; it extends from the lateral ventricle through the cerebral cortex.
 Axial CT image reveals no enhancement in the white matter lesion in the right frontal lobe after the intravenous administration of contrast material.
Axial CT image reveals no enhancement in the white matter lesion in the right frontal lobe after the intravenous administration of contrast material.
 Contrast-enhanced head CT scan reveals a low-attenuating cortical tuber (arrow) in a 10-year-old patient with tuberous sclerosis.
Contrast-enhanced head CT scan reveals a low-attenuating cortical tuber (arrow) in a 10-year-old patient with tuberous sclerosis.
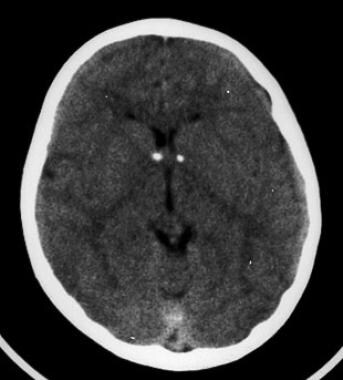
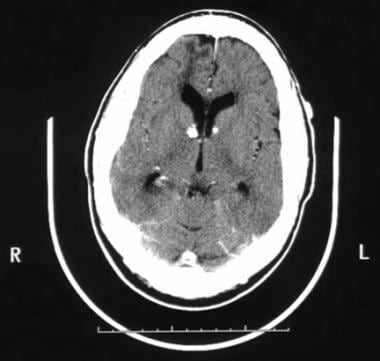
 Axial nonenhanced CT scan obtained in the same patient as in the previous image shows multiple hyperattenuating subependymal tubers.
Axial nonenhanced CT scan obtained in the same patient as in the previous image shows multiple hyperattenuating subependymal tubers.
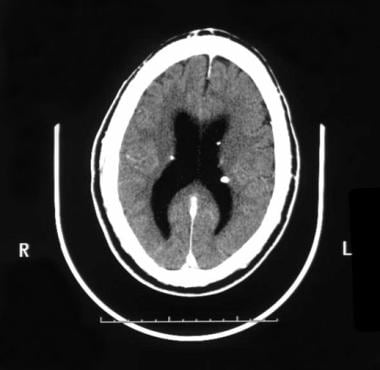 In tuberous sclerosis, the subependymal hamartomas depicted on CT scans have a high propensity to become calcified, and the incidence of calcification increases with patient age. The images reveal calcified subependymal nodules that have a typical appearance and location.
In tuberous sclerosis, the subependymal hamartomas depicted on CT scans have a high propensity to become calcified, and the incidence of calcification increases with patient age. The images reveal calcified subependymal nodules that have a typical appearance and location.
Subependymal nodules are found mostly along the lateral ventricles. They may appear as localized projections into the ventricular cavity. These nodules may enhance after the intravenous administration of contrast material, although contrast enhancement is more difficult to recognize on CT scans than on other images, particularly in calcified lesions. Contrast enhancement does not imply malignant transformation.
In 10-15% of patients, subependymal nodules may transform into giant cell astrocytomas. These tumors are benign and usually occur at or near the foramen of Monro. These lesions typically appear inhomogeneous and usually have an inhomogeneous enhancement pattern after the intravenous administration of contrast material. They frequently are calcified, usually enlarge over time, and commonly cause obstructive hydrocephalus.
(See the image below.)
 Image obtained in a patient who presented at age 16 years with progressive headaches, papilledema, and vomiting shows a giant cell astrocytoma at the right foramen of Monro.
Image obtained in a patient who presented at age 16 years with progressive headaches, papilledema, and vomiting shows a giant cell astrocytoma at the right foramen of Monro.
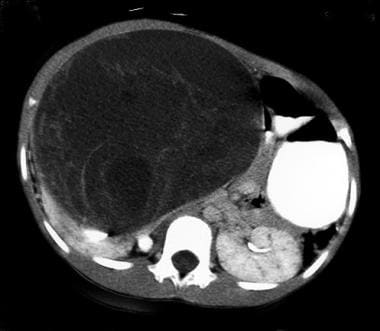
Angiomyolipomas often have low attenuation values if they contain sufficient fat, but they are indistinguishable from other renal tumors if they contain little or no lipid. Varying amounts of nonlipid tissue and hemorrhage can be visualized on CT scans of angiomyolipomas. Generally, calcification is not seen in angiomyolipomas. (See the image below
Cystic lesions commonly occur in this disease, and they are well characterized at CT. However, cystic lesions are indistinguishable from simple cysts, including those with well-defined walls, and they have attenuation similar to that of fluid and mural calcification. Multiple cysts can distort the renal collecting system; with this finding alone, tuberous sclerosis is indistinguishable from polycystic kidney disease.
CT reveals the cystic and interstitial changes in the lungs of patients with tuberous sclerosis. Abnormal findings include interstitial thickening, alveolar destruction, and honeycomb lung; these are pathologically indistinguishable from those in lymphangioleiomyomatosis (LAM). Some authors consider LAM to be a forme fruste of tuberous sclerosis.
Degree of confidence
The cortical tubers seen on CT may be somewhat nonspecific if they are not calcified. The lesions can be isoattenuating on CT scans and therefore escape detection.
In the neonate, periventricular calcifications are usually secondary to toxoplasmosis, other agents (syphilis, varicella-zoster, parvovirus B19), rubella, cytomegalovirus, and herpes simplex (TORCH) infection rather than tuberous sclerosis.
The appearance of cystic lesions in tuberous sclerosis can be indistinguishable from that of simple cysts or polycystic kidney disease; however, the presence of 1 or more simple cysts in tuberous sclerosis without angiomyolipomas is rare.
In tuberous sclerosis, renal cysts are identical to simple cysts on CT scans. The presence of multiple cysts can distort the renal collecting system, and they can be indistinguishable from those of polycystic kidney disease, including those with smooth walls. These cysts also have attenuation levels in the range of that of fluid and mural calcification.
Angiomyolipomas with minimal or no fat can mimic other lesions on CT scans, including renal cell carcinoma, which can occur in patients with tuberous sclerosis.
Magnetic Resonance Imaging
MRI is the imaging modality of choice for evaluating intracranial lesions of tuberous sclerosis. Cortical tubers, or hamartomas, are the most characteristic lesions of tuberous sclerosis; they are detected on MRIs in 95% of patients. The appearance of cortical tubers on MRIs varies with patient age. In neonates and young children, the cortical tubers and subependymal nodules are hyperintense on T1-weighted images and hypointense on T2-weighted images. In older children and adults, the cortical and subependymal lesions are isointense or hypointense on T1-weighted images. They are hyperintense relative to gray matter, as well as white matter, on T2-weighted images, depending on the presence of calcification. [16, 17, 18, 26, 19, 20, 21, 27]
(See the images below.)
 Axial T1-weighted MRI in a 15-year-old patient with tuberous sclerosis shows tiny a subependymal nodule in the right lateral ventricle (arrow). Another subtle nodule is present near the left foramen of Monro.
Axial T1-weighted MRI in a 15-year-old patient with tuberous sclerosis shows tiny a subependymal nodule in the right lateral ventricle (arrow). Another subtle nodule is present near the left foramen of Monro.
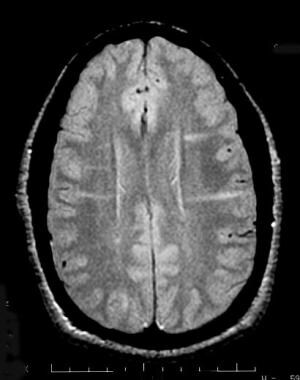 Axial proton density–weighted MRI in a 10-year-old girl with tuberous sclerosis (TS) demonstrates bilateral isointense transcortical linear streaks that are compatible with the neuronal migration anomalies seen in TS.
Axial proton density–weighted MRI in a 10-year-old girl with tuberous sclerosis (TS) demonstrates bilateral isointense transcortical linear streaks that are compatible with the neuronal migration anomalies seen in TS.
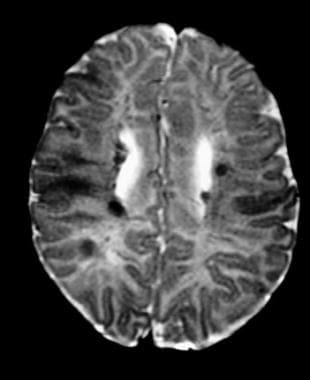 Axial T2-weighted MRI in an infant with tuberous sclerosis shows multiple low-signal-intensity subependymal and cortical tubers.
Axial T2-weighted MRI in an infant with tuberous sclerosis shows multiple low-signal-intensity subependymal and cortical tubers.
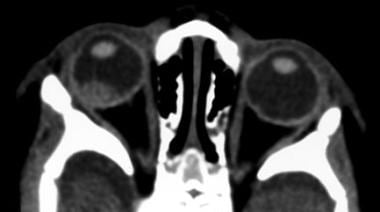
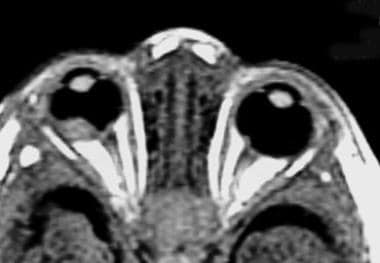 Axial T1-weighted contrast-enhanced MRI in an infant with tuberous sclerosis shows a minimally enhancing right retinal tuber and smaller left retinal tuber.
Axial T1-weighted contrast-enhanced MRI in an infant with tuberous sclerosis shows a minimally enhancing right retinal tuber and smaller left retinal tuber.
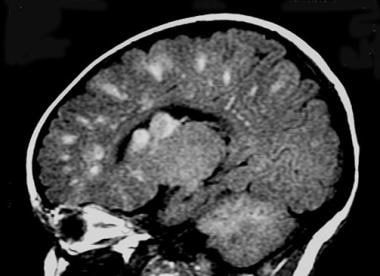 Sagittal T1-weighted MRI in an infant with tuberous sclerosis shows multiple hyperintense cortical and subependymal nodules.
Sagittal T1-weighted MRI in an infant with tuberous sclerosis shows multiple hyperintense cortical and subependymal nodules.
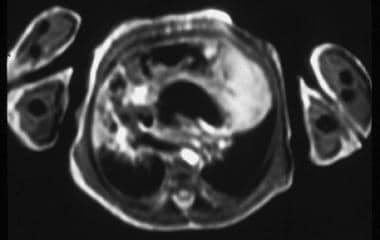 Contrast-enhanced cardiac-gated T1-weighted MRI shows an enhancing left ventricular mass. At autopsy, this mass was found to be a cardiac rhabdomyoma.
Contrast-enhanced cardiac-gated T1-weighted MRI shows an enhancing left ventricular mass. At autopsy, this mass was found to be a cardiac rhabdomyoma.
 Coronal T1-weighted cardiac-gated MRI in the same patient as in the previous image shows a hyperintense left ventricular mass.
Coronal T1-weighted cardiac-gated MRI in the same patient as in the previous image shows a hyperintense left ventricular mass.
Enhancement of cortical and subcortical lesions is uncommon and occurs in fewer than 5% of the cases. When enhancement is present, it does not suggest neoplasia. Enhancement of subependymal nodules is common, and it is better visualized on MRIs than on CT scans.
MRIs depict several distinct patterns of white matter lesions, including straight or curvilinear radial cerebral bands, wedge-shaped abnormalities, nonspecific conglomerate lesions, and cerebellar radial bands. White matter lesions in older children and adults typically are isointense or hypointense on T1-weighted images compared with white matter and hyperintense on T2-weighted images compared with gray matter and white matter. A small percentage of white matter lesions enhance after the administration of contrast material.
Subependymal nodules (SENs) are detected in 95% of patients. Subependymal giant cell astrocytomas appear inhomogeneous, with intense enhancement after the administration of contrast material. The fat in angiomyolipomas usually can be recognized; however, MRI has no specific advantage in its depiction compared with CT.
SENs are located in the ventricles and often become calcified. The lesions are best detected using CT, although they are sometimes found using MRI or plain radiography if they are calcified. SENs demonstrate a candle-dripping appearance. SENs may grow and give rise to subependymal giant cell astrocytomas (SEGAs). Detection of SEGAs is slightly more sensitive using MRI than using CT scanning.
The inability of MRI to definitively depict calcification does not undermine its diagnostic accuracy because MRI can delineate cortical tubers, white matter lesions, subependymal nodules, and subependymal giant cell astrocytomas.
Ultrasonography
Ultrasonography (US) is more sensitive than CT in detecting renal lesions. US is performed at initial diagnosis or evaluation and in family members of patients with TSC. Surveillance studies are then performed every 1-3 years. In those with renal lesions, US is repeated every 6-12 months until there is no further growth or there is regression of lesions.
Hamartoma of the kidney, which has the histologic features of an angiomyolipoma, is one of the primary manifestations of renal involvement. Hamartomas contain varying amounts of mature adipose tissue, smooth muscle, and blood vessels and usually develop in young adults and enlarge slowly. Usually, hamartomas are asymptomatic; however, they can cause flank pain, hematuria, or an abdominal mass, which may be palpable. Hamartomas usually are multiple and bilateral. Malignant degeneration of hamartomas into renal cell carcinoma can occur, but this change appears to be rare. On sonograms, the lesions are highly echogenic because of their high fat content. A finding of multiple angiomyolipomas with a high fat content is highly suggestive of tuberous sclerosis.
Angiomyolipomas can bleed and cause renal parenchymal hemorrhage, as well as subcapsular or retroperitoneal hemorrhage. Renal cysts are another primary manifestation of renal involvement. Cysts almost always are multiple; typically, they are bilateral. On sonograms, cysts are anechoic and may be indistinguishable from findings in autosomal dominant polycystic kidney disease. The kidneys may be enlarged.
Multiple angiomyolipomas in patients of either sex or an angiomyolipoma in a male patient is suggestive of tuberous sclerosis and indicates the need for further workup. Sporadic angiomyolipomas can be unrelated to tuberous sclerosis. These usually are solitary and occur in middle-aged women.
Angiomyolipomas usually are intensely hyperechoic on sonograms, but they may be difficult to distinguish from renal cell carcinoma, which also can be hyperechoic. Rarely, a renal cell carcinoma may contain some fat.
Cystic lesions of tuberous sclerosis may mimic simple renal cysts, as well as the cysts of autosomal-dominant polycystic kidney disease.
Nuclear Imaging
Nuclear medicine studies may have a minor role in the assessment of this condition. In patients who have intractable seizures, epileptogenic foci may originate from a single tuber. Single-photon emission CT (SPECT) imaging of the brain is useful during the ictal phase of seizures to detect the hyperperfusion of a seizure focus; this information can be valuable because surgery can be an option.
Positron emission tomography (PET) imaging may also be helpful in patients with seizures. PET imaging with F-18-fluorodeoxyglucose can localize tubers, which appear hypometabolic. Experimental studies using C-11 alpha methyl tryptophan (AMT) may become useful. In early studies, tubers acting as seizure foci appear hyperintense on a C-11 AMT PET images.
Renal scintigraphy demonstrates multiple hypoperfused and hypofunctioning lesions, such as cysts or angiomyolipomas; however, these findings are nonspecific.
Angiography
Angiography is dominant in the characterization of vascular derangements associated with tuberous sclerosis. Some authors believe that progressive degenerative changes or compromise of the media results in aneurysms. Thoracic and abdominal aneurysms can develop in patients as young as 10 years. Intracranial aneurysms also can be present, and one source proposes that these should be included as a nonprimary diagnostic feature of tuberous sclerosis.
Generally, angiography is not necessary to evaluate the kidney. However, if performed, angiography may demonstrate hypervascularity, neovascularity, and small arterial aneurysms in the angiomyolipomas. Cystic lesions are avascular. Findings believed to be suggestive of angiomyolipomas include pseudoaneurysms and a lack of arteriovenous (AV) shunting. AV shunting is common in renal cell carcinoma.
Percutaneous embolization may be helpful in controlling intratumoral hemorrhage from renal angiomyolipomas, especially if multiple lesions are present; in this situation, surgery may be difficult or impossible to perform.
Angiographic findings of hypervascularity, neovascularity, and small artery aneurysms also can be observed in renal cell carcinoma. These entities may be difficult to distinguish on angiograms. The presence of AV shunting may help distinguish the entities because AV shunting is common in renal cell carcinoma but rarely, if ever, observed in angiomyolipomas of tuberous sclerosis.
-
Axial nonenhanced CT image in a patient with tuberous sclerosis reveals subependymal calcifications. A hypointense right frontal lesion represents a white matter lesion or tuber; it extends from the lateral ventricle through the cerebral cortex.
-
Hyperattenuating cutaneous lesion in the left frontal region represents a calcified shagreen patch.
-
Axial CT image reveals no enhancement in the white matter lesion in the right frontal lobe after the intravenous administration of contrast material.
-
Contrast-enhanced head CT scan reveals a low-attenuating cortical tuber (arrow) in a 10-year-old patient with tuberous sclerosis.
-
Nonenhanced head CT scan reveals bilateral calcified subependymal nodules at the foramina of Monro.
-
Image obtained in a patient who presented at age 16 years with progressive headaches, papilledema, and vomiting shows a giant cell astrocytoma at the right foramen of Monro.
-
Axial T1-weighted MRI in a 15-year-old patient with tuberous sclerosis shows tiny a subependymal nodule in the right lateral ventricle (arrow). Another subtle nodule is present near the left foramen of Monro.
-
Axial proton density–weighted MRI in a 10-year-old girl with tuberous sclerosis (TS) demonstrates bilateral isointense transcortical linear streaks that are compatible with the neuronal migration anomalies seen in TS.
-
Axial T2-weighted MRI in an infant with tuberous sclerosis shows multiple low-signal-intensity subependymal and cortical tubers.
-
Nonenhanced CT scan shows large right retinal tuber in an infant with tuberous sclerosis.
-
Axial nonenhanced CT scan obtained in the same patient as in the previous image shows multiple hyperattenuating subependymal tubers.
-
Axial T1-weighted contrast-enhanced MRI in an infant with tuberous sclerosis shows a minimally enhancing right retinal tuber and smaller left retinal tuber.
-
Sagittal T1-weighted MRI in an infant with tuberous sclerosis shows multiple hyperintense cortical and subependymal nodules.
-
Contrast-enhanced cardiac-gated T1-weighted MRI shows an enhancing left ventricular mass. At autopsy, this mass was found to be a cardiac rhabdomyoma.
-
Coronal T1-weighted cardiac-gated MRI in the same patient as in the previous image shows a hyperintense left ventricular mass.
-
Image in a 16-year-old adolescent with bilateral renal angiomyolipomas.
-
Image in a 15-year-old boy with a right-sided abdominal mass, which is a renal cell carcinoma.
-
In tuberous sclerosis, the subependymal hamartomas depicted on CT scans have a high propensity to become calcified, and the incidence of calcification increases with patient age. The images reveal calcified subependymal nodules that have a typical appearance and location.