Practice Essentials
Embryologic derivation of the collecting system of the urinary tract occurs from the fetal mesonephros. As a result of this development, tumors of the renal collecting system have cell origins different from those of the renal parenchyma. These tumors are classified on the basis of their respective mesodermal or epithelial tissue origin. Primary neoplasms of the renal collecting system represent 10% of renal tumors, of which approximately 80% are malignant. Most are transitional cell carcinomas (TCCs), which are also called urothelial carcinomas. Bladder TCCs are 50 times more common than renal pelvic tumors. Often, TCCs are multiple, involving any part or all of the collecting system. The tumors are traditionally classified into papillary and nonpapillary types. Nonpapillary tumors are considered malignant.
Preferred examination
Intravenous urography (IVU) is a common diagnostic test in patients with hematuria, although the early detection of small urothelial tumors may be difficult. A meticulous IVU technique is required.
Retrograde pyelography is useful when the kidney cannot be visualized by means of IVU or when IVU cannot be performed because of renal disease or an adverse response to the contrast agent. Retrograde pyelography also has the advantage of being able to be combined with various biopsy techniques. [1]
Computed tomography (CT) scanning is becoming increasingly sensitive for the staging of early transitional cell carcinoma (TCC). Developments such as virtual cystoscopy and postmicturition scanning should improve the overall accuracy of staging by the use of CT. Multidetector-row CT scanning with postprocessing image manipulation (contour imaging) is increasingly coming to challenge IVU. [2, 3, 4] On CT scans, a hyperattenuating TCC may be confused with a blood clot, particularly in the early stages of the disease. Also, inhomogeneous renal fatty attenuation of any cause in a patient with undiagnosed early-stage TCC may hinder accurate diagnosis. [5, 6]
Magnetic resonance imaging (MRI) has the advantages of high intrinsic soft tissue contrast, direct multiplanar capability, and the availability of nontoxic, renally excreted contrast agents. MRI appears to be at least as useful as CT in the evaluation of perivesical fat involvement, and it may be superior to CT in the detection of invasion of the adjacent organs. [6] However, MRI cannot depict well the superficial invasion by TCC of the upper urinary tract. [2, 7, 8, 9, 10, 11, 12, 13, 14, 15] MRI is expensive and has limited availability. False-positive diagnoses have been reported. In staging bladder TCC, tumor extension is overstaged according to the TNM classification in 7.5% of patients; it is understaged in 32.5% of patients.
CT and MRI have been shown to perform better than cystography in the diagnosis of tumors in the bladder diverticula that are not depicted on cystograms because of obstruction at the diverticular orifice.
Ultrasonography is inaccurate for diagnosing early TCC; it is useful in the diagnosis of obstructive uropathy. [16, 17, 18] Ureteric lesions are particularly difficult to visualize unless they cause hydronephrosis and hydroureter. Other limitations of ultrasonography are that it is inaccurate in the staging of bladder TCC, particularly Ta and T1 tumors, and in the detection of pelvic lymph node involvement. On sonograms, calculi may be confused with high-grade TCCs, which can be densely echogenic. No sonographic features are specific for TCC, and many filling defects within the renal collecting system and bladder have a nonspecific appearance. It is also difficult to discern nondilated ureters on ultrasonography.
Isotope renography is an extremely sensitive means of assessing relative renal function and obstructive uropathy before surgery. Isotope bone scanning is a useful technique in the investigation of skeletal metastases. [19]
Plain radiographic findings, such as calcifications (which has a wide differential diagnosis), are not specific in the diagnosis of urothelial tumors, and they usually contribute little to the diagnosis. Filling defects in the renal collecting system and the bladder, as seen with IVU, CT, and retrograde pyelography, are present in a number of other pathologies. These findings are not specific to TCC.
Hydronephrosis on preoperative axial CT at the time of diagnosis of upper-tract urothelial carcinoma is associated with advanced-stage cancer and is a predictor of poorer outcomes. Hydronephrosis can be a valuable prognostic tool for preoperative planning and counseling regarding disease outcomes. [20]
(See the images below.)
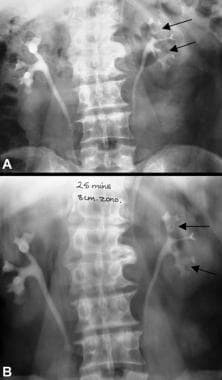
 A 21-year old man presented with a history of intermittent hematuria of 1-month duration. Three months previously, he had been assaulted and kicked in the right loin. A 30-minute intravenous urogram shows a moderate right hydronephrosis without filling of the renal pelvis, although some contrast material has passed into the upper ureter. Note also a polypoid intraluminal filling defect within the left side of the bladder (arrow).
A 21-year old man presented with a history of intermittent hematuria of 1-month duration. Three months previously, he had been assaulted and kicked in the right loin. A 30-minute intravenous urogram shows a moderate right hydronephrosis without filling of the renal pelvis, although some contrast material has passed into the upper ureter. Note also a polypoid intraluminal filling defect within the left side of the bladder (arrow).
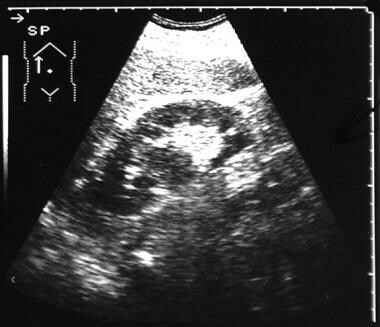
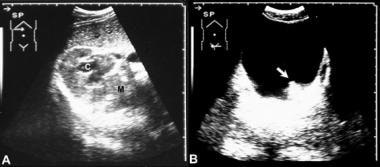 Left, transverse sonogram of the right kidney in the same patient as in the previous image shows a centrally placed solid mass within the renal pelvis with low-level echoes and with proximal hydronephrosis. Right, transverse sonogram through the bladder shows a polypoid filling defect in the bladder.
Left, transverse sonogram of the right kidney in the same patient as in the previous image shows a centrally placed solid mass within the renal pelvis with low-level echoes and with proximal hydronephrosis. Right, transverse sonogram through the bladder shows a polypoid filling defect in the bladder.
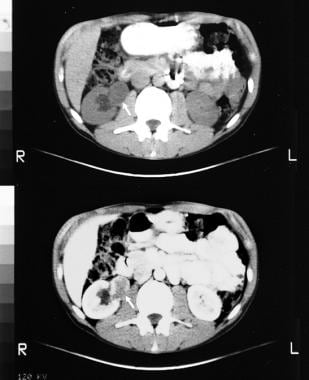 Nonenhanced (top) and enhanced (bottom) CT scans through the kidneys show a mass in the right renal pelvis. The histologic diagnosis was a right renal pelvis neurofibroma and a bladder transitional cell carcinoma.
Nonenhanced (top) and enhanced (bottom) CT scans through the kidneys show a mass in the right renal pelvis. The histologic diagnosis was a right renal pelvis neurofibroma and a bladder transitional cell carcinoma.
Radiography
Plain radiography
Plain radiographs may first alert the radiologist to presence of a renal mass or a bladder mass. Occasionally, a large renal outline may be seen in a completely obstructed kidney. Uncommonly, radiographically discernible areas of punctate calcification may be seen in transitional cell carcinoma (TCC). The calcification is on the surface of the tumor and not within the mass duct. Intrinsic calcifications suggest an adenocarcinoma or an unusual cell type.
TCC is associated with analgesic nephropathy. Plain radiographic findings of displacement of renal calcifications, which occur in analgesic nephropathy, may be the first sign of TCC. Surface calcification of a bladder tumor may be seen on plain radiographs in 1% of cases. Osseous expansive destruction or lung metastases may be seen in the presence of renal malignancy.
Intravenous urography
The most common findings in TCC of the kidney are single or multiple filling defects in the renal pelvis, as seen in 35% of cases. In about 26% of patients with renal TCC, the calyx is dilated; such dilation is caused by partial or complete obstruction of the infundibulum. Amputation of the calyx may be seen in 19% of cases.
In 13-31% of cases, the affected kidney is not visualized. Such failure to visualize the kidney is usually secondary to hydronephrosis but can be the result of tumor infiltrating and replacing functioning kidney or of occlusion of the renal vein. Hydronephrosis with renal enlargement caused by tumoral obstruction of the ureteropelvic junction may be seen in 6% of cases.
(See the images below.)
 Localized views of the right vesicoureteric junction obtained after intravenous urography shows a polypoid filling defect in the lower right ureter due to a transitional cell carcinoma.
Localized views of the right vesicoureteric junction obtained after intravenous urography shows a polypoid filling defect in the lower right ureter due to a transitional cell carcinoma.
 A 10-minute intravenous urogram in a 56-year-old man presenting with hematuria. The image shows a mass lesion in the right renal pelvis that bisects the renal sinus and splays the adjacent calyces.
A 10-minute intravenous urogram in a 56-year-old man presenting with hematuria. The image shows a mass lesion in the right renal pelvis that bisects the renal sinus and splays the adjacent calyces.
 Scout radiograph in a 53-year-old man presenting with hematuria shows a few small vague opacities in the left renal area; these are suggestive of renal calculi.
Scout radiograph in a 53-year-old man presenting with hematuria shows a few small vague opacities in the left renal area; these are suggestive of renal calculi.
 Intravenous urogram shows 2 filling defects: 1 in the upper pole and 1 in the lower-pole calyces. Conventional tomographic results (bottom) confirm the findings.
Intravenous urogram shows 2 filling defects: 1 in the upper pole and 1 in the lower-pole calyces. Conventional tomographic results (bottom) confirm the findings.
 An intravenous urogram in a 36-year old woman who presented with evidence of a urinary tract infection and gross hematuria. A 10-minute intravenous urogram shows a filling defect in the lower pole calyx on the right. A provisional diagnosis of transitional cell carcinoma was made. Subsequent investigations and the course of events proved that the filling defect was caused by a blood clot related to the hematuria secondary to acute pyelonephritis.
An intravenous urogram in a 36-year old woman who presented with evidence of a urinary tract infection and gross hematuria. A 10-minute intravenous urogram shows a filling defect in the lower pole calyx on the right. A provisional diagnosis of transitional cell carcinoma was made. Subsequent investigations and the course of events proved that the filling defect was caused by a blood clot related to the hematuria secondary to acute pyelonephritis.
Various signs have been described in renal TCC. The stipple sign is a rare sign that occurs when contrast material is trapped within the interstices of a papillary tumor. When this is seen en face, the tumor appears to contain multiple stipples. This sign is highly suggestive of TCC. When this sign is seen, blood clots and radiolucent calculi are excluded, and further investigations are superfluous. Punctate calcification on a TCC may mimic the stipple sign.
Punctate calcification is unusual in TCC; such calcification is apparent on the scout image before the intravenous contrast material is delivered. Occasionally, contrast material may be trapped within a blood clot formed in the ureter and then extruded into the bladder as a stringy mass that may trap contrast material in an irregular fashion. However, this entrapment is coarser than that seen with neoplastic stippling.
Fungus balls or mycetoma may also occasionally entrap contrast material. The pattern of entrapment is lamellar; such entrapment is frequently associated with gas formation (frequently, patients have poorly controlled diabetes with urinary tract infections). Rarely, stippling may be observed in tubular ectasia when papillae containing dilated ducts of Bellini are seen en face. Inspection of the other papillae may make the diagnosis obvious.
Phantom calyx represents the failure of a calyx to opacify because of obstruction. Oncocalyx represents calyceal distention caused by the tumor.
In contrast to renal TCC, ureteric tumors show single or multiple filling defects in only 19% of cases. This observation is associated with hydronephrosis and hydroureter in 34% of cases; in advanced cases, it may be associated with a nonfunctioning kidney.
Bladder TCC also shows an irregular filling defect with broad base and fronds. Increased thickness of the bladder wall in the region of the tumor should indicate infiltration.
Retrograde pyelography
Retrograde pyelography in ureteric TCC may show focal expansion of ureters around and distal to the mass; such a finding is called the champagne, or goblet, sign. This finding is helpful in differentiating TCC from focal lesions of other causes, such as calculi or blood clots. Typically, calculi and blood clots do not demonstrate a goblet sign because they do not progressively stretch the ureteral wall from slow growth. Occasionally, the catheter coils below the mass during retrograde catheterization; this is called the Bergman sign.
(See the image below.)
 Left retrograde pyelogram shows marked irregularity of the infundibulum of the upper pole calyx caused by infiltration by transitional cell carcinoma. This information was unavailable on the CT scans.
Left retrograde pyelogram shows marked irregularity of the infundibulum of the upper pole calyx caused by infiltration by transitional cell carcinoma. This information was unavailable on the CT scans.
Degree of confidence
Plain radiographic findings, such as calcifications, are not specific in the diagnosis of urothelial tumors. Discernible areas of a coarse, punctate pattern of calcification with a mucosal lesion on excretory urography or retrograde pyelography may suggest TCC. An important role for plain radiography is in searching for evidence of osseous metastases that may herald renal malignancy.
Multidetector-row CT is replacing IVU in the evaluation of hematuria, although IVU is still being used. The early detection of small urothelial tumors demands a meticulous IVU technique. Accurate demonstration of the pelvocaliceal system requires abdominal compression to distend the collecting systems, and oblique imaging or tomography may also be necessary. Diuresis multidetector-row CT with contour reformatting of the axial records may be useful. This technique does not require abdominal compression. Early experience with this method has been most positive because the CT technique demonstrates not only the opacified lumen but also the surrounding soft tissue anatomy.
Filling defects with dilated calyces are easily seen and are readily diagnosed. Hydronephrosis with renal enlargement is easily confused with uncomplicated primary pelvic hydronephrosis; antegrade/retrograde pyelography is usually required for diagnosis.
Adequate depiction of the ureters is difficult, and prone, oblique, or even spot images obtained during fluoroscopy may be required at urography. If an area of constant narrowing of the ureters is seen on more than 1 image and if it cannot be explained by the presence of a crossing vessel or a peristaltic wave, a tumor must be suspected. A meticulous urographic examination (radiographic or multidetector-row CT) can prevent unnecessary pyelography/ureterography in the majority of cases.
Importantly, if the demonstration of the pelvicaliceal system at excretion urography or CT is poor, an upper-tract tumor may be missed, particularly when a decoy of a bladder tumor is present. The coexistence of upper- and lower-tract tumors is not rare.
The sensitivity and specificity with regard to the upper urinary tract pathology are 67% and 91%, respectively, for IVU. Sensitivity and specificity of upper urinary tract pathology by ultrasonography are 56% and 94%, respectively. For both techniques combined, sensitivity is 79% and specificity is 88%. IVU has a 70% accuracy rate in the diagnosis of bladder TCC. The role of radiology is in demonstrating the upper urinary tract, both at the time of the initial diagnosis and during the follow-up of urothelial cancer.
Retrograde pyelography is useful when the kidney cannot be visualized with IVU or when an intravenous approach cannot be performed because of renal disease or an adverse reaction to contrast agents. Retrograde pyelography in combination with brush biopsy is a highly reliable method for making a definitive diagnosis of TCC. The results are considered diagnostic in 85% of cases.
If spot filming is the imaging technique, this should be performed in an appropriate fluoroscopic digital unit where serial images can be obtained. This may be done during diuresis urography (infusion IVU with 300 mL of 30% contrast media) or during antegrade/retrograde pyelography.
Approximately 5% of ureteric TCCs grow intramurally, resulting in a stricture rather than a filling defect. Radiologically, distinguishing this type of tumor from stricture is impossible. However, at CT, a thickened ureteric wall with stranding may be seen.
False positives/negatives
Calcification is seen in 10% of renal cell carcinomas. Extrinsic ureteric obstruction may be caused by retroperitoneal tumors, infections, or inflammation; pelvic tumors; pelvic lipomatosis; and gynecologic and gastrointestinal pathologies. Other causes of ureteric obstruction or bladder abnormalities include irradiation, surgery, trauma, or infections such as tuberculosis or schistosomiasis. These conditions may result in telltale signs on plain radiographs.
Other causes of filling defects may mimic a TCC, such as radiolucent or uric acid stones; blood clots; sloughed papilla caused by papillary necrosis; or fungal balls in patients with diabetes. Vessel crossing may cause a linear extrinsic impression; in these cases, oblique or compression images may help differentiate TCCs from urothelial tumors. Tuberculosis can cause narrowing of the infundibulum and irregular calices. With regard to imaging, tuberculosis is the major disorder in the differential diagnosis.
Other mimics include pyeloureteritis cystica, renal cell carcinoma invading the pelvicaliceal system, or choleastoma. Squamous cell carcinoma (SCC) is radiographically indistinguishable from TCC; however, SCC is less likely to be a polypoid tumor. Although a diagnosis may be made on the basis of urograms or cystograms, a small bladder tumor, especially one of the infiltrative types, may go undetected. Furthermore, a dense concentration of contrast material may obscure the intraluminal part of the urothelial tumor.
Mimics of ureteric TCC include papilloma or polyp, which commonly produces a long, smooth intraluminal filling defect. This defect may prolapse up and down the ureter on serial images, and it may even intussuscept. Avoiding the introduction of air bubbles is important because these could be mistaken for tumors.
Computed Tomography
Although the workup of patients in whom TCC is suspected includes ultrasonography and IVU, CT scanning enables the detection and staging of TCC, usually without the need for additional imaging. [3, 4, 15, 21, 22, 23] The commonly recognized presentations of TCC on CT scans include irregular filling defects of the pelvocaliceal system and ureters (which tend to be associated with obstruction and dilatation of the ureter and pelvis proximal to the lesion); ureteral wall thickening; frondlike growths projecting into the bladder from a fixed mural site; and surface calcification of bladder TCC.
On nonenhanced CT scans, the TCC is hypoattenuated or isoattenuated relative to the normal renal parenchyma, and it is hyperattenuated relative to urine. TCCs demonstrate mild to moderate enhancement after the administration of contrast material, and they are hypoattenuated relative to opacified urine.
(See the images below).
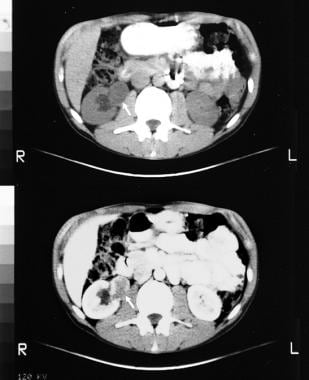 Nonenhanced (top) and enhanced (bottom) CT scans through the kidneys show a mass in the right renal pelvis. The histologic diagnosis was a right renal pelvis neurofibroma and a bladder transitional cell carcinoma.
Nonenhanced (top) and enhanced (bottom) CT scans through the kidneys show a mass in the right renal pelvis. The histologic diagnosis was a right renal pelvis neurofibroma and a bladder transitional cell carcinoma.
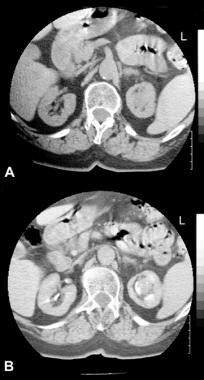 Nonenhanced (top) and enhanced (bottom) CT scans obtained through the kidneys in a 73-year-old woman show a mass in the left renal pelvis is a transitional cell carcinoma.
Nonenhanced (top) and enhanced (bottom) CT scans obtained through the kidneys in a 73-year-old woman show a mass in the left renal pelvis is a transitional cell carcinoma.
Degree of confidence
CT is of limited value in staging low-grade disease because it cannot accurately depict the depths of tumor invasion. Therefore, stages Ta-T2 cannot be distinguished. The strength of CT lies in the staging of high-grade disease, because of its ability to demonstrate peripelvic, periureteric, and local pelvic extensions, as well as distant metastases.
Inevitably, studies differ with regard to the sensitivity and specificity of preoperative CT scanning in the detection and accurate staging of TCC. The reported range for detection efficiency is 86-100%. The results of most studies suggest a range of 55-64% for correct TNM staging, as compared with surgical findings.
Understaging appears to be a limiting factor. However, results with newer scanners and adjunct techniques such as virtual cystoscopy and postmicturition scanning should improve the overall accuracy of staging with CT.
In stage I or II disease, conditions such as chronic pyelitis, tuberculosis, and xanthogranulomatous pyelonephritis may mimic TCC.
In stage III or IV disease, CT cannot be used to distinguish edema, infection, inflammatory changes, or hemorrhage from tumor. All of these processes may cause inhomogeneous peripelvic attenuation that is indistinguishable from that caused by the infiltration of fat by tumor. Superimposed pyelonephritis can cause inhomogeneous renal enhancement and thus give a false interpretation of invasion by underlying TCC. Occasionally, renal cell carcinoma may simulate TCC with renal parenchymal infiltration.
The characteristic attenuation of a TCC lesion is normally sufficiently different from renal tract filling defects of other causes, such as calculi and blood clots, to enable the correct diagnosis. However, a blood clot may be confused with a hyperattenuating TCC, particularly in the early stages of the disease. Also, in a patient with undiagnosed early-stage TCC, inhomogeneous renal fat attenuation of any cause may hinder accurate diagnosis.
Magnetic Resonance Imaging
The advantages of MRI are its high intrinsic soft tissue contrast, its direct multiplanar capability, and the availability of nontoxic renally excreted contrast agents. MRI appears to be at least as useful as CT in the evaluation of perivesical fat involvement, and it may be superior to CT in the detection of invasion of the adjacent organs. However, MRI cannot depict the superficial invasion of the upper urinary tract by TCC well. [7, 8, 9, 10, 11, 12, 13, 14]
CT and MRI have been shown to perform better than cystography in the diagnosis of tumors in the bladder diverticula that are not depicted on cystograms because of obstruction at the diverticular orifice.
False-positive diagnoses have been reported. In staging bladder TCC, tumor extension is overstaged according to the TNM classification in 7.5% of patients and is understaged in 32.5% of patients.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with troublemoving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
The most common sonographic appearance of TCC is that of a hypoechoic mass in the renal collecting system that splits the central echocomplex with varying degrees of infundibular dilatation. Focal hypoechogenicity of adjacent renal cortex reflects local invasion. Occasionally, the central echocomplex may be only segmentally amputated. [16, 17, 18]
Ultrasonography is inaccurate for diagnosing early TCC; it is useful in the diagnosis of obstructive uropathy. Ureteric lesions are particularly difficult to visualize unless they cause hydronephrosis and hydroureter. The other limitation of ultrasonography is that it is inaccurate in the staging of bladder TCC, particularly Ta and T1 tumors, and also in the detecton of pelvic lymph node involvement.
On sonograms, calculi may be confused with high-grade TCCs, which can be densely echogenic. No sonographic features are specific for TCC, and many filling defects within the renal collecting system and bladder may have a nonspecific appearance. In addition, ultrasonography is limited in its capacity to depict nondilated ureters.
(See the images below.)
 Longitudinal sonogram obtained through the right kidney shows a hypoechoic mass bisecting the renal sinus fat. The mass is a transitional cell carcinoma.
Longitudinal sonogram obtained through the right kidney shows a hypoechoic mass bisecting the renal sinus fat. The mass is a transitional cell carcinoma.
 Top, Longitudinal sonogram obtained thorough the left kidney in a 58-year-old man presenting with hematuria shows a normal left kidney. Bottom, More medial section through the same kidney shows a vague isoechoic mass in the upper of the kidney. Whether this finding represented an artifact or a genuine lesion was unclear. Technetium-99m dimercaptosuccinate (99mTc DMSA) scanning is good modality for differentiating a renal pseudomass from a genuine mass.
Top, Longitudinal sonogram obtained thorough the left kidney in a 58-year-old man presenting with hematuria shows a normal left kidney. Bottom, More medial section through the same kidney shows a vague isoechoic mass in the upper of the kidney. Whether this finding represented an artifact or a genuine lesion was unclear. Technetium-99m dimercaptosuccinate (99mTc DMSA) scanning is good modality for differentiating a renal pseudomass from a genuine mass.
 Longitudinal sonogram through left kidney shows that the filling defects are due to calculi. Ultrasonography is an efficient means for differentiating between radiolucent calculi and uroepithelial tumors.
Longitudinal sonogram through left kidney shows that the filling defects are due to calculi. Ultrasonography is an efficient means for differentiating between radiolucent calculi and uroepithelial tumors.
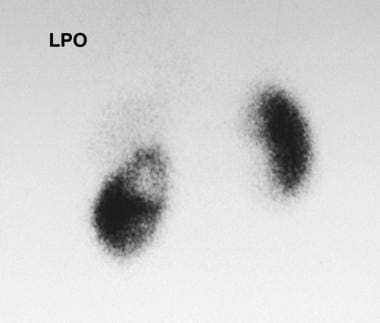
Nuclear Imaging
Isotope renography is an extremely sensitive means of assessing relative renal function and obstructive uropathy before surgery. Isotope bone scanning is a useful technique in the investigation of skeletal metastases. [19, 24, 25]
(See the image below.)
Questions & Answers
Overview
What are transitional cell carcinomas (TCCs)?
What is the role of imaging in the workup of transitional cell carcinoma (TCC)?
How are transitional cell carcinomas (TCCs) staged?
What are the limitations of transitional cell carcinoma (TCC) imaging techniques?
Which retrograde pyelography findings are characteristic of transitional cell carcinomas (TCCs)?
What is the role of plain radiography in transitional cell carcinoma (TCC) imaging?
Which findings on IV urography (IVU) are characteristic of transitional cell carcinomas (TCCs)?
What is the accuracy of radiography for transitional cell carcinomas (TCCs) imaging?
What is the role of CT scanning in transitional cell carcinoma (TCC) imaging?
What is the accuracy of CT scanning for transitional cell carcinomas (TCCs) imaging?
What is the role of MRI in transitional cell carcinoma (TCC) imaging?
What is the accuracy of MRI for transitional cell carcinomas (TCCs) imaging?
Which ultrasonography findings are characteristic of transitional cell carcinoma (TCC)?
What is the accuracy of ultrasonography for transitional cell carcinomas (TCCs) imaging?
Which nuclear imaging findings are characteristic of transitional cell carcinoma (TCC)?
-
A 21-year old man presented with a history of intermittent hematuria of 1-month duration. Three months previously, he had been assaulted and kicked in the right loin. A 30-minute intravenous urogram shows a moderate right hydronephrosis without filling of the renal pelvis, although some contrast material has passed into the upper ureter. Note also a polypoid intraluminal filling defect within the left side of the bladder (arrow).
-
Left, transverse sonogram of the right kidney in the same patient as in the previous image shows a centrally placed solid mass within the renal pelvis with low-level echoes and with proximal hydronephrosis. Right, transverse sonogram through the bladder shows a polypoid filling defect in the bladder.
-
Nonenhanced (top) and enhanced (bottom) CT scans through the kidneys show a mass in the right renal pelvis. The histologic diagnosis was a right renal pelvis neurofibroma and a bladder transitional cell carcinoma.
-
An intravenous urogram in a 36-year old woman who presented with evidence of a urinary tract infection and gross hematuria. A 10-minute intravenous urogram shows a filling defect in the lower pole calyx on the right. A provisional diagnosis of transitional cell carcinoma was made. Subsequent investigations and the course of events proved that the filling defect was caused by a blood clot related to the hematuria secondary to acute pyelonephritis.
-
Localized views of the right vesicoureteric junction obtained after intravenous urography shows a polypoid filling defect in the lower right ureter due to a transitional cell carcinoma.
-
A 10-minute intravenous urogram in a 56-year-old man presenting with hematuria. The image shows a mass lesion in the right renal pelvis that bisects the renal sinus and splays the adjacent calyces.
-
Longitudinal sonogram obtained through the right kidney shows a hypoechoic mass bisecting the renal sinus fat. The mass is a transitional cell carcinoma.
-
Nonenhanced (top) and enhanced (bottom) CT scans obtained through the kidneys in a 73-year-old woman show a mass in the left renal pelvis is a transitional cell carcinoma.
-
Left retrograde pyelogram shows marked irregularity of the infundibulum of the upper pole calyx caused by infiltration by transitional cell carcinoma. This information was unavailable on the CT scans.
-
Top, Longitudinal sonogram obtained thorough the left kidney in a 58-year-old man presenting with hematuria shows a normal left kidney. Bottom, More medial section through the same kidney shows a vague isoechoic mass in the upper of the kidney. Whether this finding represented an artifact or a genuine lesion was unclear. Technetium-99m dimercaptosuccinate (99mTc DMSA) scanning is good modality for differentiating a renal pseudomass from a genuine mass.
-
Left posterior view of a technetium-99m dimercaptosuccinate (99mTc DMSA) scan shows a photon-deficient mass in the upper pole of the left kidney; this finding indicates a genuine mass in this region. At partial nephrectomy, transitional cell carcinoma was confirmed.
-
Scout radiograph in a 53-year-old man presenting with hematuria shows a few small vague opacities in the left renal area; these are suggestive of renal calculi.
-
Intravenous urogram shows 2 filling defects: 1 in the upper pole and 1 in the lower-pole calyces. Conventional tomographic results (bottom) confirm the findings.
-
Longitudinal sonogram through left kidney shows that the filling defects are due to calculi. Ultrasonography is an efficient means for differentiating between radiolucent calculi and uroepithelial tumors.