Practice Essentials
Abnormal development of the pulmonary veins may result in either partial or complete anomalous drainage back into the systemic venous circulation. In contrast, partial anomalous pulmonary venous return (PAPVR) is usually an acyanotic condition. In PAPVR, an anomalous pulmonary vein drains into a systemic vein rather than the right atrium and nvolves the right lung more often than the left. The most common form of PAPVR is that of an isolated right upper lobe PAPVR draining into the superior vena cava, which is often associated with a sinus venosus atrial septal defect. [1] Total anomalous pulmonary venous return (TAPVR) is a congenital disorder characterized by total mixing of systemic venous blood and pulmonary venous blood within the heart. This complete mixing of venous blood produces cyanosis. [2, 3, 4, 5]
For patients with anomalous pulmonary venous return, echocardiography is the preferred examination. [6, 7, 4] The echocardiogram demonstrates an enlarged right ventricle and a small left atrium. It may also show the pattern of abnormal pulmonary venous connections. When the pattern of Doppler venous flow of the abdominal veins is obtained, the finding of venous flow away from the heart is pathognomonic of TAPVR below the diaphragm. Shunting occurs almost exclusively from right to left at the atrial level. [8]
Electrocardiograms demonstrate right ventricular hypertrophy, usually a qR pattern in V3, R, and V1. The P waves are frequently tall and spiked.
TAPVR is a cyanotic lesion. Echocardiographic results usually confirm the diagnosis. In a study by Ali et al, echocardiography was found to have a diagnostic sensitivity of 81% for TAPVR. [9] MRI and fast CT are also useful for defining pulmonary venous drainage. [10, 11] With cardiac catheterization, the presence of anomalous pulmonary veins may be demonstrated by means of selective pulmonary arteriography. [12, 13]
Sometimes, in anomalous pulmonary venous return, echocardiographic views are limited, and MRI may be necessary.
There are 3 major clinical patterns of TAPVR:
-
Severe pulmonary venous obstruction
-
Early heart failure
-
Mildly symptomatic or asymptomatic TAPVR.
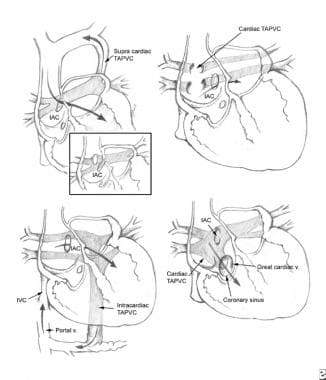
(See the image below depicting TAPVR.)
The history, physical signs, and electrocardiographic and radiographic findings of PAPVR and TAPVR are similar to those seen in patients with an isolated ostium secundum atrial septal defect (ASD). In some cases, an anomalous vein that drains into the inferior vena cava appears on chest radiography as a crescentic shadow of vascular opacity (like a scimitar) along the right border of the cardiac silhouette (scimitar syndrome). [5] In these patients, an associated ASD is not seen; rather, pulmonary sequestration and anomalous arterial supply to the affected lobe of the lung are encountered.
Fast CT is useful for defining pulmonary drainage. The degree of confidence is good for anomalous pulmonary venous return. [10] False-positive and false-negative results are rare in anomalous pulmonary venous return. [14] The use of low-dose multidetector CT angiography (MDCTA) may be useful in both the diagnosis and management of PAPVR and TAPVR. [15]
First-pass multiple gated (MUGA) scintigraphy may be useful in identifying right chamber enlargement, shunt flow, and, possibly, asymmetry of pulmonary vascularity; however, the images are harder to interpret, and MUGA scintigraphy is less reliable than other imaging modalities.
Radiography
In older children, radiographic findings indicating that the anomalous pulmonary veins enter the innominate vein and that persistent left superior vena cava is present are pathognomonic for anomalous pulmonary venous return. A large supracardiac shadow together with the normal cardiac shadow may have a "snowman" appearance.
Even in patients without obstruction, the heart is enlarged, the pulmonary artery and right ventricle are prominent, and the pulmonary vascularity is increased. In neonates with marked pulmonary venous obstruction, the chest radiograph demonstrates a perihilar pattern of pulmonary edema and a small heart.
In cases of partial anomalous pulmonary venous return (PAPVR) in which more than 2 pulmonary veins have anomalous drainage, right ventricular dilation, pulmonary hypertension, and increased pulmonary blood flow in the lung fields are characteristically seen. Occasionally, the superior vena cava is dilated or an azygous vein or a left vertical vein is present.
The most interesting finding is encountered in cases in which there is anomalous drainage of the right pulmonary veins into the inferior vena cava. In such cases, the pulmonary venous pattern exhibits a crescent-shaped or scimitar-shaped curve along the right heart border in the right lower lung field (scimitar syndrome). [5]
The degree of confidence with radiography is moderate. The "snowman" appearance is not helpful for diagnosis in early infancy because of the thymus. False-positive and false-negative results are rare. In patients with pulmonary obstruction, findings of pulmonary congestion and a small heart may be misinterpreted as indicating primary pulmonary disease.
Computed Tomography
In a retrospective study of 41 patients with TAPVR (10 patients) or PAPVR (31 patients), anomalous pulmonary venous drains and associated cardiac and extracardiac anomalies were reliably and quickly detected with high-pitch, low-dose CT without sedation in pediatric patients (age range, 6 mo to 15 yr; mean, 3 yr), according to Gozgec et al. Of the 10 patients with TAPVR, 6 had the supracardiac type, 2 had the cardiac type, and 2 had the mixed type, and all 10 patients had a large atrial septal defect (ASD). In the 31 patients with PAPVR, 40 cases of PAPVR were identified, with 27 of the cases being right sided and 13 left sided. Twenty of the PAPVR patients also had atrial septal defect (12), persistent superior vena cava (4), patent ductus arteriosus (3), or aortic coarctation (2). [10]
Magnetic Resonance Imaging
MRI is useful for defining pulmonary venous drainage. On MRI, anomalous pulmonary venous return is evidenced by a lack of pulmonary veins to the left atrium; the presence of anomalously routed pulmonary veins; a large right atrium; a large right ventricle; a right-to-left interatrial shunt; and, possibly, asymmetry of the pulmonary vasculature. Gradient-refocused gradient echo imaging (eg, FIESTA) in a short-axis stack covering the entire atria is particularly helpful for identifying pulmonary venous return. Two-dimensional cine phase contrast is particularly helpful for identifying and quantifying shunt flow. [11, 16, 17, 18, 19]
The degree of confidence is high with MRI for anomalous pulmonary venous return. False-positive and false-negative results are rare in anomalous pulmonary venous return.
Ultrasonography
In cases of anomalous pulmonary venous return, the echocardiogram demonstrates a large right ventricle; in addition, a pattern of abnormal pulmonary venous connections is usually seen. The demonstration of a vessel in the abdomen with Doppler venous flow away from the heart is pathognomonic of total anomalous pulmonary venous return (TAPVR) below the diaphragm. Shunting occurs almost exclusively from right to left at the atrial level. [20, 21, 22, 23]
The degree of confidence is high with ultrasonography for anomalous pulmonary venous return. False-positive and false-negative results are rare in anomalous pulmonary venous return.
Angiography
For patients with anomalous pulmonary venous return, cardiac catheterization shows that the levels of oxygen saturation of blood in both atria, in both ventricles, and in the aorta are more or less similar; such results are indicative of a total mixing lesion. An increase in systemic venous saturation occurs at the site of entry of the abnormal pulmonary venous channel. Oxygen saturation sampling may help identify a step-up at the sites of pulmonary venous return.
In older patients, the pulmonary arterial and right ventricular pressures may be only moderately elevated. In infants who present with pulmonary venous obstruction, pulmonary hypertension is usual.
The anatomy of the pulmonary veins, as well as their point of entry into the systemic venous circulation, may be seen on selective pulmonary arteriography or venography.
The degree of confidence with angiography is case-dependent, and findings are not always definitive for anomalous pulmonary venous return. False-positive and false-negative results are rare in anomalous pulmonary venous return.
-
Anomalous pulmonary venous return (APVR). Types of total anomalous pulmonary venous connection.