Practice Essentials
Schwannomas are slow-growing, benign, encapsulated neoplasms that arise from the nerve sheath and consist of Schwann cells in a collagenous matrix. These lesions account for 6-8% of intracranial neoplasms; vestibular schwannomas are the most common cranial nerve (CN) schwannomas, followed by trigeminal and facial schwannomas and then glossopharyngeal, vagus, and spinal accessory nerve schwannomas. A study of patients undergoing MRI for indications other than the evaluation of schwannoma revealed an estimated prevalence of 0.07%. Trigeminal schwannomas are rare, accounting for only 0.07-0.3% of all intracranial tumors and only 0.8-5% of intracranial schwannomas. They mostly occur during the fourth through sixth decades of life. [1, 2, 3, 4, 5, 6, 7, 8]
Schwannomas can arise from all cranial nerves except the optic. They can also occur in spinal nerve roots, flexor surfaces of the upper and lower extremities, and the tongue. [9] In neurofibromatosis 2 (NF2), the eighth cranial nerve is affected, and the classic finding is a bilateral vestibular schwannoma. [9] CN schwannomas are usually isolated lesions, except when they are associated with NF2. [10] NF2 is also called the multiple inherited schwannomas, meningiomas, and ependymomas (MISME) syndrome. NF2 is characterized by bilateral vestibular schwannomas. Schwannomas of the other CNs occur more frequently in NF2, and the presence of one of the rare CN schwannomas should suggest the possibility of NF2. Meningiomas and intramedullary ependymomas of the spinal cord also occur in NF2. [9]
Patients with CN schwannomas can present with loss of function of the affected nerve, but they can also be asymptomatic. In these latter patients, the lesion may be incidentally discovered on computed tomography (CT) scans or MRIs obtained for reasons other than the evaluation of a schwannoma.
Before the advent of magnetic resonance imaging (MRI), imaging of the cranial nerves was difficult, and mass lesions arising from these nerves was often indirectly detected only by looking at bony changes in the skull base foramen or by using invasive techniques such as cisternography and angiography. Current imaging techniques provide noninvasive highly detailed imaging of most of the CNs and the lesions (eg, schwannomas) that affect them. [11, 12, 1, 13, 14, 15]
Varying growth patterns in schwannomas are described as Antoni type A neurilemoma and type B neurilemoma. Although type A tissue has elongated spindle cells arranged in irregular streams and is compact in nature, type B tissue has a looser organization, often with cystic spaces intermixed within the tissue. The cystic spaces can result in high signal intensity on T2-weighted MRIs. Schwannomas involving the oculomotor, trochlear, abducens, and hypoglossal nerves are rare. See the images below.
Imaging modalities
MRI with the use of gadolinium-based contrast medium is the technique of choice for imaging the CNs. [3, 16, 17, 18, 19, 20] MRI provides the highest degree of soft-tissue resolution, can provide images in multiple planes, and is not encumbered by bone artifact from the skull base. CT scanning is ideal for evaluating the secondary effects on the neural foramen. [21, 18] Aside from a patient's claustrophobia or incompatible hardware, the only significant imaging drawback of MRI is that CT scanning can be more sensitive in depicting adjacent bone destruction. [21]
On T1-weighted MRI, a schwannoma demonstrates hypointensity, and on T2-weighted MRI, hyperintensity. On MRI, signs include split fat sign (thin peripheral rim of fat on T1WI), target sign (central low signal within the lesion), and fascicular sign (multiple internal small ring-like structures). [1]
CT evaluation may be limited primarily to the assessment of bony changes in the skull base. On contrast-enhanced CT, a schwannoma displays heterogeneous enhancement [1] Artifact from the skull base limits the soft-tissue resolution of CT scans, particularly in small lesions. [21] Plain radiography has no role in the evaluation of the lesions.
Schwannomas on ultrasound are characterized by round or elliptical cross-section, with a clear border and an internal echo. Ultrasound may have greater diagnostic utility in cases in which the nerve diameter is large and the tumor is connected to the nerve. [22]
Failure to perform MRI when CN tumors are suggested is a concern. In particular, CT scans of the brain are inadequate for evaluating CNs, and the reliance on negative CT findings to exclude a CN lesion may lead to liability.
(See the images below.)
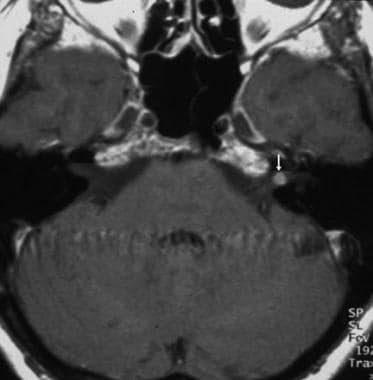
 Contrast-enhanced T1-weighted magnetic resonance image at the level of the internal auditory canal shows a strongly enhancing cisternal vestibular schwannoma (arrow) that compresses the adjacent pons and cerebellum and distorts the fourth ventricle.
Contrast-enhanced T1-weighted magnetic resonance image at the level of the internal auditory canal shows a strongly enhancing cisternal vestibular schwannoma (arrow) that compresses the adjacent pons and cerebellum and distorts the fourth ventricle.
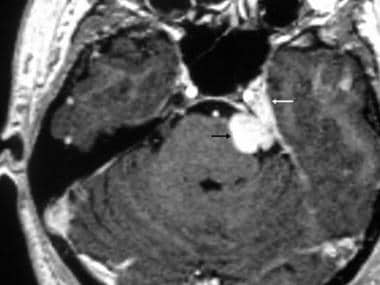
 Contrast-enhanced T1-weighted axial magnetic resonance image through the internal auditory canal shows a heterogeneously enhancing intracanalicular-cisternal vestibular schwannoma (white arrow). Anterior to the schwannoma, a tumor-related cyst is depicted (black arrow).
Contrast-enhanced T1-weighted axial magnetic resonance image through the internal auditory canal shows a heterogeneously enhancing intracanalicular-cisternal vestibular schwannoma (white arrow). Anterior to the schwannoma, a tumor-related cyst is depicted (black arrow).
 Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
 Vestibular schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image confirms an intracanalicular mass (arrow).
Vestibular schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image confirms an intracanalicular mass (arrow).
 Bilateral vestibular schwannomas. Axial contrast-enhanced T1-weighted magnetic resonance image reveals bilateral vestibular schwannomas (arrows), which are diagnostic of neurofibromatosis type 2.
Bilateral vestibular schwannomas. Axial contrast-enhanced T1-weighted magnetic resonance image reveals bilateral vestibular schwannomas (arrows), which are diagnostic of neurofibromatosis type 2.
Anatomy
Motor neurons of the oculomotor nerve (ie, CN III) leave the midbrain at the level of the tegmentum and emerge in the interpeduncular cistern. Here, it passes between the posterior cerebral artery (PCA) above) and the superior cerebellar artery (SCA) below, and it turns anteriorly to enter the cavernous sinus. In the cavernous sinus, the oculomotor nerve courses along the lateral wall; it is the most superior of all the nerves in the sinus. The nerve enters the orbit via the superior orbital fissure and then splits into superior and inferior divisions.
From the trochlear nucleus in the midbrain, fibers of the trochlear nerve (ie, CN IV) cross the midline dorsal to the cerebral aqueduct and exit the midbrain dorsally. From here, the fibers run around the midbrain to the ventral surface. Like the oculomotor nerve, the trochlear nerve also courses between the PCA and SCA and along the lateral wall of the cavernous sinus. It enters the orbit at the superior orbital fissure.
The trigeminal nerve (ie, CN V) exits the brainstem at the level of the mid pons, and its 3 divisions—the ophthalmic (CN V1), maxillary (CN V2), and mandibular (CN V3) branches—together proceed anteriorly toward the trigeminal ganglion in the Meckel cave, as shown in the image below. From here, the mandibular division exits inferiorly via the foramen ovale. The maxillary and ophthalmic divisions continue anteriorly along the lateral aspect of the cavernous sinus. Eventually, the ophthalmic division enters the orbit via the superior orbital fissure, while the maxillary division exits the cranial vault through the foramen rotundum.
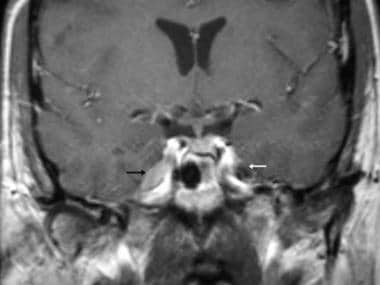 Lymphoma of the Meckel cave. Coronal contrast-enhanced T1-weighted magnetic resonance image shows an enhancing mass in the Meckel cave on the right (white arrow). The left Meckel cave is without tumor (black arrow). Lymphomatous meningitis can mimic a cranial nerve schwannoma.
Lymphoma of the Meckel cave. Coronal contrast-enhanced T1-weighted magnetic resonance image shows an enhancing mass in the Meckel cave on the right (white arrow). The left Meckel cave is without tumor (black arrow). Lymphomatous meningitis can mimic a cranial nerve schwannoma.
The abducens nerve (ie, CN VI) exits the brainstem ventrally at the level of the junction of the pons and medullary pyramid and courses anterolaterally toward the dorsum sellae, passing over the petrous apex, where it makes a sharp turn to enter the cavernous sinus. In the sinus, the abducens nerve is medial to CN IV, CN V1, and CN V2. Along with the oculomotor and trochlear nerves, the abducens nerve also enters the orbit via the superior orbital fissure, then enters the deep surface of the lateral rectus muscle.
The paths of the facial nerve (ie, CN VII) and vestibular nerve (ie, CN VIII) are intimately associated. They exit the brainstem at the pontomedullary junction, with the facial nerve slightly medial to the vestibular nerve. From there, they enter the internal auditory canal (IAC). Once in the IAC, the facial nerve courses in the superior-anterior quadrant of the canal, while the vestibular division of the vestibular nerve courses in the posterior superior and inferior quadrants, and the cochlear division courses in the inferior-posterior quadrant. CN VIII then enters the labyrinth. (The mnemonic for this arrangement is "Seven-Up and Coke [ie, cochlear] down.") [23]
The facial nerve enters the labyrinth (labyrinthine segment), courses anteriorly in the temporal bone to the geniculate ganglion, turns posteriorly to pass beneath the lateral semicircular canal (tympanic segment) and then inferiorly to course through the mastoid (vertical segment), and exits the temporal bone via the stylomastoid foramen. Finally, the facial nerve courses within the parotid gland (parotid segment) before branching.
The glossopharyngeal (ie, CN IX), vagus (ie, CN X), and accessory (ie, CN XI) nerves emerge cranial to caudal, in that order, from the ventral medulla, lateral to the medullary olive. From there, they course toward the jugular foramen and exit the skull base at the jugular foramen. The glossopharyngeal nerve is located in the pars nervosa of the jugular foramen, and the vagus and accessory nerves are located within the more posterior pars vascularis.
The hypoglossal nerve (CN XII) is formed by the fusion of multiple rootlets that emerge from the ventrolateral sulcus between the medullary olive and pyramid. The nerve exits the cranial vault via the hypoglossal canal, then lies medial to CN IX, CN X, and CN XI.
Differentials and other problems to be considered
The differential diagnosis varies with the location, but meningiomas can occur in similar regions and have similar imaging appearances as schwannomas. The differing growth patterns, as well as the dural tail and associated hyperostosis that can be seen with meningiomas, are often helpful differentiating factors. (See the image below.)
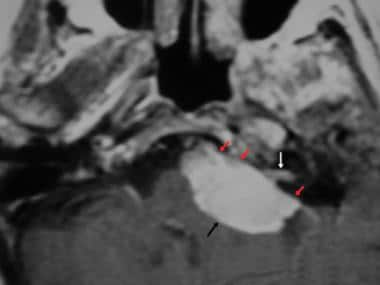 Cerebellopontine angle meningioma. Axial contrast-enhanced T1-weighted magnetic resonance image through the cerebellopontine angle shows a large cisternal mass. The intracanalicular component (white arrow) can mimic a vestibular schwannoma, although the broad-based dural attachment (red arrows) is more consistent with a meningioma.
Cerebellopontine angle meningioma. Axial contrast-enhanced T1-weighted magnetic resonance image through the cerebellopontine angle shows a large cisternal mass. The intracanalicular component (white arrow) can mimic a vestibular schwannoma, although the broad-based dural attachment (red arrows) is more consistent with a meningioma.
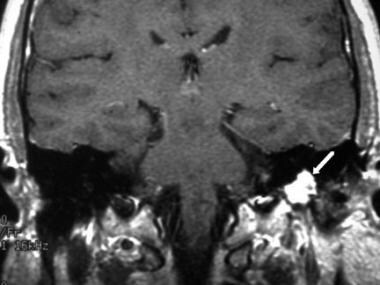
Cerebrospinal fluid (CSF) spread of metastatic disease or lymphoma can appear as a focal CN mass. In patients with carcinomatous meningitis and lymphoma, focal metastatic masses can involve the cranial nerves and mimic a schwannoma. (See the images below.)
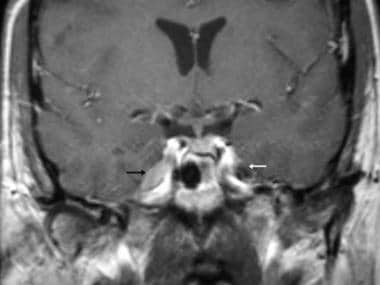 Lymphoma of the Meckel cave. Coronal contrast-enhanced T1-weighted magnetic resonance image shows an enhancing mass in the Meckel cave on the right (white arrow). The left Meckel cave is without tumor (black arrow). Lymphomatous meningitis can mimic a cranial nerve schwannoma.
Lymphoma of the Meckel cave. Coronal contrast-enhanced T1-weighted magnetic resonance image shows an enhancing mass in the Meckel cave on the right (white arrow). The left Meckel cave is without tumor (black arrow). Lymphomatous meningitis can mimic a cranial nerve schwannoma.
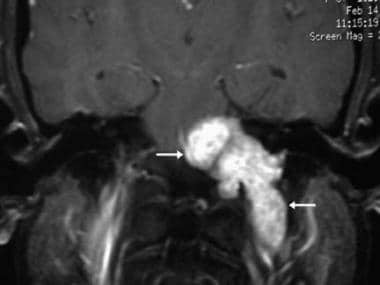
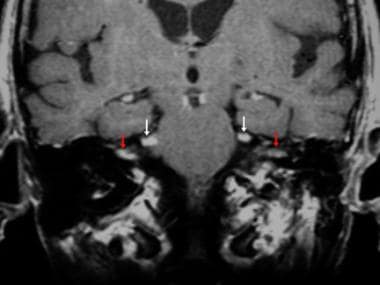 Carcinomatous meningitis. Coronal contrast-enhanced T1-weighted magnetic resonance image reveals bilateral cranial nerve V (white arrows) and cranial nerve VIII masses (red arrows). The patient had lung cancer with cerebrospinal fluid spread manifesting as multiple cranial nerve masses.
Carcinomatous meningitis. Coronal contrast-enhanced T1-weighted magnetic resonance image reveals bilateral cranial nerve V (white arrows) and cranial nerve VIII masses (red arrows). The patient had lung cancer with cerebrospinal fluid spread manifesting as multiple cranial nerve masses.
Neuritis (ie, inflammation of a nerve) can be confused with a mass. (See the images below.)
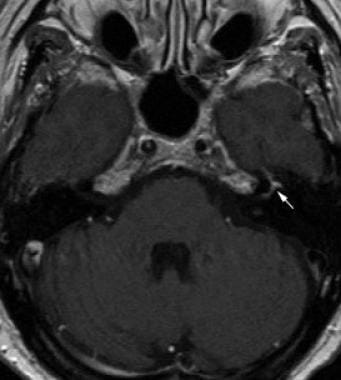 Facial neuritis. Axial contrast-enhanced T1-weighted magnetic resonance image shows enhancement of the distal intracanalicular, labyrinthine, and geniculate, segments (arrow) of cranial nerve VII.
Facial neuritis. Axial contrast-enhanced T1-weighted magnetic resonance image shows enhancement of the distal intracanalicular, labyrinthine, and geniculate, segments (arrow) of cranial nerve VII.
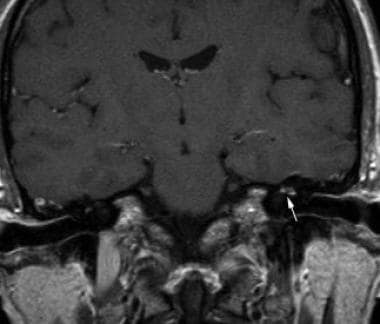 Facial neuritis. Coronal contrast-enhanced T1-weighted magnetic resonance image shows enhancement of the labyrinthine and tympanic segments of cranial nerve VII (arrow).
Facial neuritis. Coronal contrast-enhanced T1-weighted magnetic resonance image shows enhancement of the labyrinthine and tympanic segments of cranial nerve VII (arrow).
NF2 is one of the phacomatoses characterized by multiple intracranial schwannomas, meningiomas, and ependymomas. Bilateral vestibular schwannomas are diagnostic of this entity, but patients can have schwannomas involving any CN (CN III-XIII). (See the image below.) Other conditions to be considered include glomus tumors of the head and Neck and NF1.
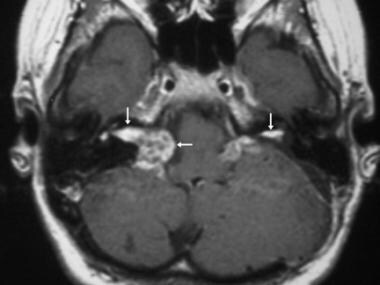 Bilateral vestibular schwannomas. Axial contrast-enhanced T1-weighted magnetic resonance image reveals bilateral vestibular schwannomas (arrows), which are diagnostic of neurofibromatosis type 2.
Bilateral vestibular schwannomas. Axial contrast-enhanced T1-weighted magnetic resonance image reveals bilateral vestibular schwannomas (arrows), which are diagnostic of neurofibromatosis type 2.
Radiologic intervention
Stereotactic radiosurgery (SRT) (ie, gamma knife radiosurgery) largely has replaced surgical resection for the treatment of vestibular schwannomas, particularly when the lesions do not compress the brainstem. Lesions should be smaller than 3 cm. Studies have demonstrated rates of tumor control (ie, lesion stabilizes or shrinks) of greater than 95% and a rate of hearing preservation of approximately 70%. Although less well studied, other CN schwannomas also can be treated with radiosurgery. [24, 25, 26, 27, 28, 29]
Nishioka et al demonstrated stereotactic radiotherapy is an effective alternative to surgical resection for patients with nonacoustic intracranial nerve schwannomas not only for long-term local tumor control but also preservation of neurofunction. [30] Following stereotactic radiotherapy, tumor size decreased in 3 patients, remained stable in 13, and increased in 1. Neurologic symptoms improved in 8 patients and remained unchanged in 9 patients. In 1 patient, an increase in tumor size necessitated microsurgical resection. No worsening of neurologic symptoms or development of new cranial nerve deficits was reported. [30]
Congress of Neurological Surgeons guidelines
The Congress of Neurological Surgeons published evidence-based guidelines on intraoperative cranial nerve monitoring in vestibular schwannoma surgery, including the following [31] :
-
It is recommended that intraoperative facial nerve monitoring be routinely utilized during vestibular schwannoma surgery to improve long-term facial nerve function.
-
Intraoperative facial nerve monitoring can be used to accurately predict favorable long-term facial nerve function after vestibular schwannoma surgery. Favorable testing results reliably portends a good long-term facial nerve outcome, but the absence of favorable testing results in the setting of an anatomically intact facial nerve does not reliably predict poor long-term function and therefore cannot be used to direct decision-making regarding the need for early reinnervation procedures.
-
Poor intraoperative EMG electrical response of the facial nerve should not be used as a reliable predictor of poor long-term facial nerve function.
-
Intraoperative eighth cranial nerve monitoring should be used during vestibular schwannoma surgery when hearing preservation is attempted.
Computed Tomography
On nonenhanced CT scans, most schwannomas are isoattenuating relative to brain parenchyma. Calcification or areas of hemorrhage are rare. On contrast-enhanced CT scans, the enhancement pattern is typically homogeneous. [21] On contrast-enhanced CT of a schwannoma, heterogeneous enhancement and cystic and fatty degeneration can be demonstrated. [1, 13]
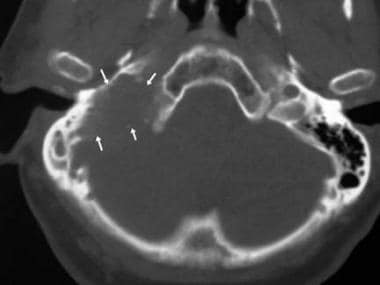
Bone-window images can demonstrate remodeling of the adjacent skull base, such as expansion of the IAC by vestibular schwannomas and expansion of the facial canal by facial schwannomas. Expansion of the jugular foramen by CN IX, CN X, or CN XI schwannomas can also be seen. (See the image below.)
 Computed tomography scan through the skull base shows soft-tissue expansion of the facial nerve canal in the petrous bone (arrow).
Computed tomography scan through the skull base shows soft-tissue expansion of the facial nerve canal in the petrous bone (arrow).
Thin-collimation CT imaging of the skull base can be helpful in evaluating bone destruction. This finding is useful in differentiating jugular foramen schwannomas from paragangliomas. (See the image below.)
 Glomus jugulare. Axial computed tomography scan obtained through the skull base shows extensive bone destruction (arrows), unlike the smooth expansion seen with schwannomas.
Glomus jugulare. Axial computed tomography scan obtained through the skull base shows extensive bone destruction (arrows), unlike the smooth expansion seen with schwannomas.
Degree of confidence
With CT scanning, large lesions can be diagnosed with a high degree of confidence. However, distinguishing a schwannoma from a meningioma may not be possible by using CT scanning. A small lesion that affects a CN cannot be confidently excluded.
CT findings can be false-negative in small lesions. Occasionally, a false-positive diagnosis occurs because a streak artifact in the cerebellopontine angle cistern mimics a lesion.
Magnetic Resonance Imaging
Similar to CT imaging, MRI tends to depict schwannomas as homogeneous masses. [9, 16, 17, 32, 9, 33, 14] Schwannomas are typically isointense or slightly hypointense relative to gray matter on T1-weighted images and slightly hypointense to CSF on T2-weighted images. Gadolinium enhancement is typically homogeneous, although larger schwannomas can show areas of cystic degeneration and heterogeneous signal intensity; these findings are based on increased numbers of areas with Antoni type B histologic features.
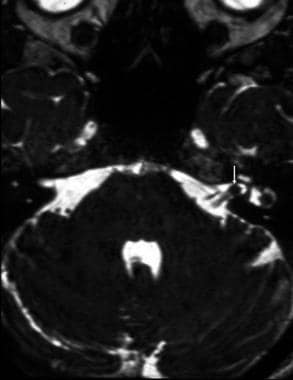
High-resolution, thin-section, heavily T2-weighted, 3-dimensional (3-D) sequences have been used to look for acoustic neuromas. On images obtained with these sequences, individual nerves in the cistern and internal auditory canal (IAC) can be visualized as linear filling defects in the bright CSF. Small masses can be identified without the use of an intravenously administered contrast agent. (See the image below.)
 Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
Vestibular schwannomas are the most common CN schwannomas. Typically, the masses are located in the cerebellopontine angle (CPA) and centered at the porus, with extension into the IAC. Their appearance has been described as that of a comet tail or ice cream cone, with the cone as the intracanalicular extension and the ice cream as the cisternal component. The long axis of the tumors is parallel to the petrous surface. [10, 18, 34, 9, 33, 14]
Although schwannomas of the eighth cranial nerve characteristically occur in the IAC, these tumors can rarely originate within the vestibule, cochlea, or semicircular canals and are termed intralabyrinthine schwannomas. With MRI, small (< 2mm) intracochlear schwannomas (ICS) have been detected and localized. On gadolinium-enhanced T1-weighted imaging, an ICS shows sharply delineated edges, and on spin-echo T2-weighted images, signal loss in the high-intensity intralabyrinthine fluid is shown. [23]
NF2 is characterized by bilateral vestibular schwannomas. [9]
(See the images below.)
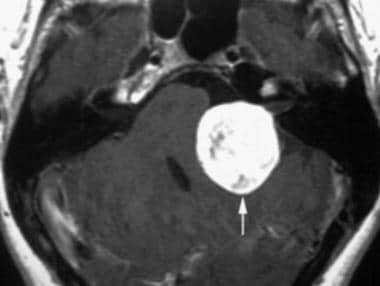
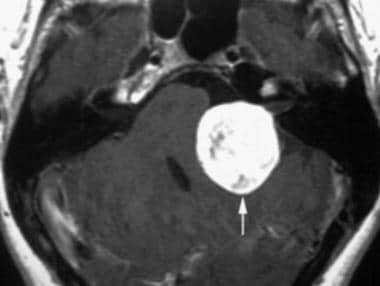 Contrast-enhanced T1-weighted magnetic resonance image at the level of the internal auditory canal shows a strongly enhancing cisternal vestibular schwannoma (arrow) that compresses the adjacent pons and cerebellum and distorts the fourth ventricle.
Contrast-enhanced T1-weighted magnetic resonance image at the level of the internal auditory canal shows a strongly enhancing cisternal vestibular schwannoma (arrow) that compresses the adjacent pons and cerebellum and distorts the fourth ventricle.
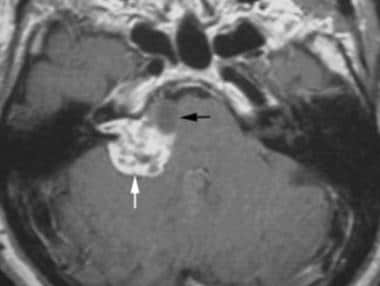
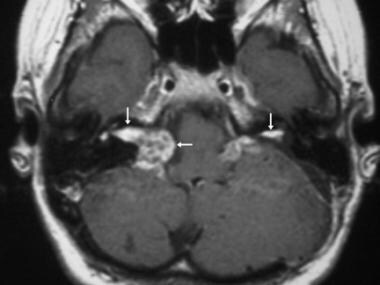
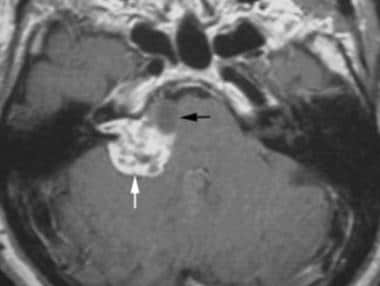 Contrast-enhanced T1-weighted axial magnetic resonance image through the internal auditory canal shows a heterogeneously enhancing intracanalicular-cisternal vestibular schwannoma (white arrow). Anterior to the schwannoma, a tumor-related cyst is depicted (black arrow).
Contrast-enhanced T1-weighted axial magnetic resonance image through the internal auditory canal shows a heterogeneously enhancing intracanalicular-cisternal vestibular schwannoma (white arrow). Anterior to the schwannoma, a tumor-related cyst is depicted (black arrow).
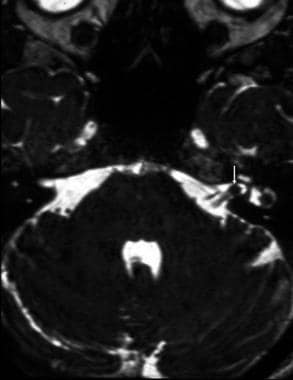 Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
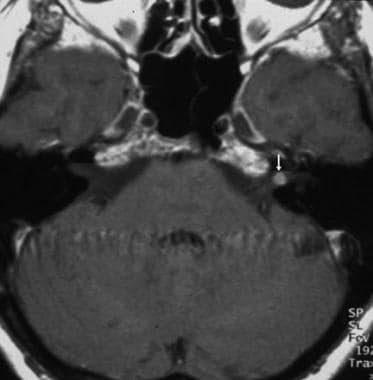 Vestibular schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image confirms an intracanalicular mass (arrow).
Vestibular schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image confirms an intracanalicular mass (arrow).
Occasionally, tumors can be entirely intracanicular, in which case the primary differential diagnosis is a meningioma of the CPA. Unlike vestibular schwannomas, meningiomas tend to form obtuse angles with the adjacent petrous bone, are typically hemispheric, and often extend into the middle fossa as a result of herniation. Meningiomas can be differentiated by their broad base of attachment along the petrous bone and by the presence of a dural tail. Meningiomas uncommonly extend into the IAC. [17] (See the image below.)
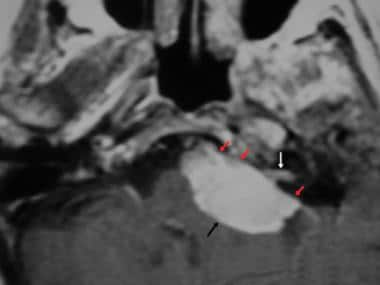 Cerebellopontine angle meningioma. Axial contrast-enhanced T1-weighted magnetic resonance image through the cerebellopontine angle shows a large cisternal mass. The intracanalicular component (white arrow) can mimic a vestibular schwannoma, although the broad-based dural attachment (red arrows) is more consistent with a meningioma.
Cerebellopontine angle meningioma. Axial contrast-enhanced T1-weighted magnetic resonance image through the cerebellopontine angle shows a large cisternal mass. The intracanalicular component (white arrow) can mimic a vestibular schwannoma, although the broad-based dural attachment (red arrows) is more consistent with a meningioma.
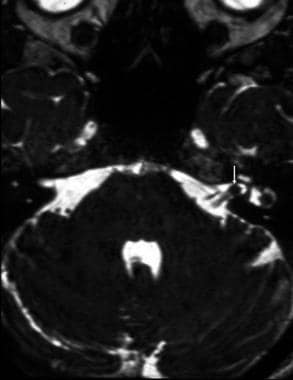
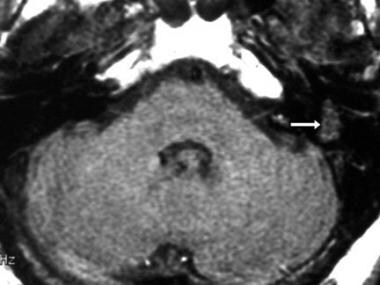
Schwannomas of the facial nerve can occur along any segment, but they frequently involve the geniculate ganglion and extend proximally or distally from there. MRI and CT imaging characteristics are similar to those of vestibular schwannomas. The location of the mass results in variable growth patterns. In the IAC, facial schwannomas are indistinguishable from vestibular lesions. When facial schwannomas cross the petrous bone to involve both the middle and posterior fossa, they cross in the mid portion of the petrous bone. In contrast, trigeminal schwannomas cross near the petrous apex. Lesions in the geniculate ganglion can be mistaken for temporal lobe lesions, and imaging in the coronal plane is useful in evaluating the lesions.( See the images below.)
 Facial schwannoma. Axial T1-weighted magnetic resonance image at the level of the internal auditory canal shows a soft-tissue mass (arrow) along the course of the tympanic segment of the facial nerve.
Facial schwannoma. Axial T1-weighted magnetic resonance image at the level of the internal auditory canal shows a soft-tissue mass (arrow) along the course of the tympanic segment of the facial nerve.
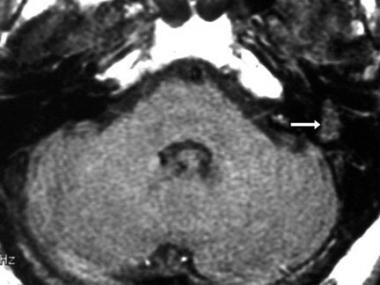
 Facial schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows a schwannoma (arrow) involving the mastoid segment of cranial nerve VII.
Facial schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows a schwannoma (arrow) involving the mastoid segment of cranial nerve VII.
Thompson et al elucidated the appearance of the schwannoma on MRIs and demonstrated that enhanced MRI is the imaging modality of choice for facial nerve schwannomas. [12] All lesions in their study involved 2 or more contiguous segments of the facial nerve, with 28 (93%) involving 3 or more segments. The median number of segments involved per lesion was 4, with a mean of 3.83. Geniculate involvement was most common, present in 29 patients (97%). CPA and IAC involvement was significantly related to sensorineural hearing loss (SNHL). [12] Seventeen patients (57%) presented with facial nerve dysfunction, which manifested in 12 patients as facial nerve weakness or paralysis and in 8 patients as involuntary movements of the facial musculature. [12]
Trigeminal schwannomas can arise in the Meckel cave or in the cistern along the course of the nerve. [35] Extension and expansion of the foramen rotundum or ovale is common, and the masses can have a bilobed appearance. Tumors can also grow posteriorly to involve the posterior fossa, or they can grow anteriorly into the cavernous sinus. Trigeminal schwannomas tend to have a more cystic component than other schwannomas. (See the images below.)
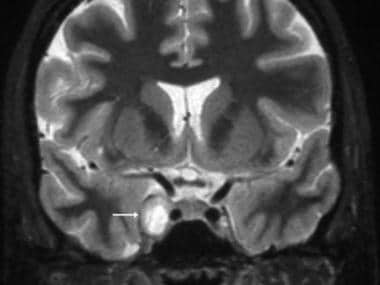 Trigeminal schwannoma. Coronal T2-weighted magnetic resonance image shows a hyperintense mass in the right cavernous sinus (arrow).
Trigeminal schwannoma. Coronal T2-weighted magnetic resonance image shows a hyperintense mass in the right cavernous sinus (arrow).
 Trigeminal schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image at the level of the mid pons shows a strongly enhancing mass involving the left cranial nerve V in the cistern (black arrow) and Meckel cave (white arrow).
Trigeminal schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image at the level of the mid pons shows a strongly enhancing mass involving the left cranial nerve V in the cistern (black arrow) and Meckel cave (white arrow).
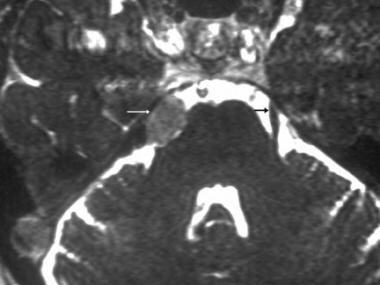 Trigeminal schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a mass in the region of the cisternal segment of the right cranial nerve V (white arrow). The left cranial nerve V without tumor (black arrow) is also depicted.
Trigeminal schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a mass in the region of the cisternal segment of the right cranial nerve V (white arrow). The left cranial nerve V without tumor (black arrow) is also depicted.
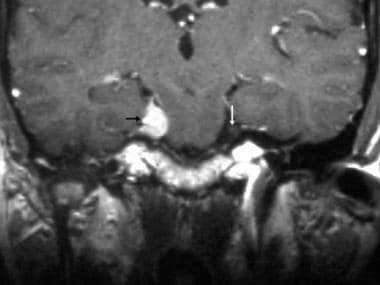 Trigeminal schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows the mass arising from the cisternal segment of the right cranial nerve V. The left cranial nerve V (without tumor) is also shown (arrow).
Trigeminal schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows the mass arising from the cisternal segment of the right cranial nerve V. The left cranial nerve V (without tumor) is also shown (arrow).
Glossopharyngeal, vagus, or accessory nerve schwannomas are rare and difficult to distinguish from one another. The tumors are classified on the basis of their growth patterns: Type A lesions grow predominantly intracranially, type B lesions grow predominantly at the jugular foramen, and type C lesions grow predominantly extracranially. CT scan and MRI characteristics are similar to those of other schwannomas. In contrast to the more common paragangliomas in this region, schwannomas expand but do not infiltrate the adjacent bone. Unlike paragangliomas, which infiltrate and erode adjacent bone, schwannomas smoothly expand the bone and leave an intact cortical margin. (See the images below.)
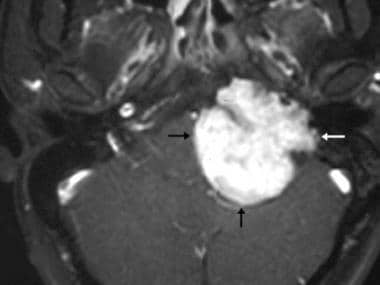 Glossopharyngeal schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image shows a large extra-axial mass that compresses the brainstem (black arrows) and extends into the skull base (white arrows).
Glossopharyngeal schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image shows a large extra-axial mass that compresses the brainstem (black arrows) and extends into the skull base (white arrows).
 Glossopharyngeal schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows a mass (arrows) extending through the skull base via the jugular foramen.
Glossopharyngeal schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows a mass (arrows) extending through the skull base via the jugular foramen.
Hypoglossal schwannomas have growth patterns and imaging characteristics similar to those of jugular foramen schwannomas. When large enough, the tumors can erode the hypoglossal canal to such an extent that their differentiation from jugular foramen schwannomas can be difficult. [36]
Schwannomas of the abducens nerve (ie, CN VI) are rare. They are reported to occur in the prepontine cistern, with a heterogeneous appearance on CT scans and MRIs and extension into the adjacent cavernous sinus. As with other schwannomas, meningioma is the primary differential diagnosis, and the presence of areas of cystic change (which have high signal intensity on T2-weighted images) can suggest the likelihood of schwannoma instead of meningioma. Similarly, CN IV schwannomas are rare. (See the image below.)
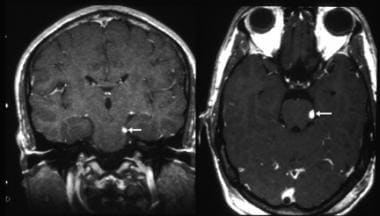 Cranial nerve IV schwannoma. Axial and coronal contrast-enhanced T1-weighted magnetic resonance images demonstrate a small mass (arrows) involving the cisternal segment of cranial nerve IV adjacent to the midbrain. Courtesy of Glenn A Tung, MD, Brown Medical School.
Cranial nerve IV schwannoma. Axial and coronal contrast-enhanced T1-weighted magnetic resonance images demonstrate a small mass (arrows) involving the cisternal segment of cranial nerve IV adjacent to the midbrain. Courtesy of Glenn A Tung, MD, Brown Medical School.
Schwannomas of the oculomotor nerve are reported in the literature, but they are exceedingly rare. The tumors can present as masses in the suprasellar cistern, and they can be difficult to distinguish from meningiomas in this region.
Gadolinium warning
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Degree of confidence
A diagnosis of a CN mass can be made with a high degree of confidence by using MRI.
False-positive findings occur primarily in the jugular fossa, where slow flow in the jugular bulb can mimic a mass. A false-negative diagnosis can occur if imaging is inadequate—for example, if the image sections are too thick or if fat suppression is not used in evaluating the skull base.
Angiography
Angiography is not used as a diagnostic modality for schwannomas. However, when studied with angiography, schwannomas typically appear hypovascular; this finding distinguishes them from paragangliomas when the lesion is in the jugular fossa. (See the images below.)
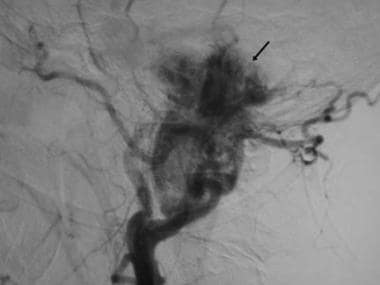
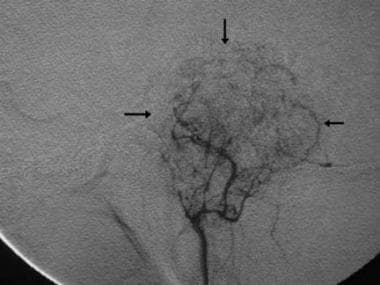 Glossopharyngeal schwannoma. Digital subtraction angiogram obtained with an ascending pharyngeal arterial injection reveals a moderately hypervascular schwannoma (arrows), which is atypical for schwannomas.
Glossopharyngeal schwannoma. Digital subtraction angiogram obtained with an ascending pharyngeal arterial injection reveals a moderately hypervascular schwannoma (arrows), which is atypical for schwannomas.
-
Contrast-enhanced T1-weighted magnetic resonance image at the level of the internal auditory canal shows a strongly enhancing cisternal vestibular schwannoma (arrow) that compresses the adjacent pons and cerebellum and distorts the fourth ventricle.
-
Contrast-enhanced T1-weighted axial magnetic resonance image through the internal auditory canal shows a heterogeneously enhancing intracanalicular-cisternal vestibular schwannoma (white arrow). Anterior to the schwannoma, a tumor-related cyst is depicted (black arrow).
-
Intracanalicular vestibular schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a 3-mm mass (arrow) in the internal auditory canal as a filling defect in the bright cerebrospinal fluid.
-
Vestibular schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image confirms an intracanalicular mass (arrow).
-
Cerebellopontine angle meningioma. Axial contrast-enhanced T1-weighted magnetic resonance image through the cerebellopontine angle shows a large cisternal mass. The intracanalicular component (white arrow) can mimic a vestibular schwannoma, although the broad-based dural attachment (red arrows) is more consistent with a meningioma.
-
Bilateral vestibular schwannomas. Axial contrast-enhanced T1-weighted magnetic resonance image reveals bilateral vestibular schwannomas (arrows), which are diagnostic of neurofibromatosis type 2.
-
Computed tomography scan through the skull base shows soft-tissue expansion of the facial nerve canal in the petrous bone (arrow).
-
Facial schwannoma. Axial T1-weighted magnetic resonance image at the level of the internal auditory canal shows a soft-tissue mass (arrow) along the course of the tympanic segment of the facial nerve.
-
Facial schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows a schwannoma (arrow) involving the mastoid segment of cranial nerve VII.
-
Facial neuritis. Axial contrast-enhanced T1-weighted magnetic resonance image shows enhancement of the distal intracanalicular, labyrinthine, and geniculate, segments (arrow) of cranial nerve VII.
-
Facial neuritis. Coronal contrast-enhanced T1-weighted magnetic resonance image shows enhancement of the labyrinthine and tympanic segments of cranial nerve VII (arrow).
-
Trigeminal schwannoma. Coronal T2-weighted magnetic resonance image shows a hyperintense mass in the right cavernous sinus (arrow).
-
Trigeminal schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image at the level of the mid pons shows a strongly enhancing mass involving the left cranial nerve V in the cistern (black arrow) and Meckel cave (white arrow).
-
Trigeminal schwannoma. Axial constructive interference in the steady state (CISS) magnetic resonance image shows a mass in the region of the cisternal segment of the right cranial nerve V (white arrow). The left cranial nerve V without tumor (black arrow) is also depicted.
-
Trigeminal schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows the mass arising from the cisternal segment of the right cranial nerve V. The left cranial nerve V (without tumor) is also shown (arrow).
-
Lymphoma of the Meckel cave. Coronal contrast-enhanced T1-weighted magnetic resonance image shows an enhancing mass in the Meckel cave on the right (white arrow). The left Meckel cave is without tumor (black arrow). Lymphomatous meningitis can mimic a cranial nerve schwannoma.
-
Cranial nerve IV schwannoma. Axial and coronal contrast-enhanced T1-weighted magnetic resonance images demonstrate a small mass (arrows) involving the cisternal segment of cranial nerve IV adjacent to the midbrain. Courtesy of Glenn A Tung, MD, Brown Medical School.
-
Carcinomatous meningitis. Coronal contrast-enhanced T1-weighted magnetic resonance image reveals bilateral cranial nerve V (white arrows) and cranial nerve VIII masses (red arrows). The patient had lung cancer with cerebrospinal fluid spread manifesting as multiple cranial nerve masses.
-
Glossopharyngeal schwannoma. Axial contrast-enhanced T1-weighted magnetic resonance image shows a large extra-axial mass that compresses the brainstem (black arrows) and extends into the skull base (white arrows).
-
Glossopharyngeal schwannoma. Coronal contrast-enhanced T1-weighted magnetic resonance image shows a mass (arrows) extending through the skull base via the jugular foramen.
-
Extracranial vagal schwannoma. Axial contrast-enhanced computed tomography scan shows a heterogeneous mass (arrow) in the neck posterior to the carotid vessels.
-
Glomus jugulare. Axial computed tomography scan obtained through the skull base shows extensive bone destruction (arrows), unlike the smooth expansion seen with schwannomas.
-
Glossopharyngeal schwannoma. Digital subtraction angiogram obtained with an ascending pharyngeal arterial injection reveals a moderately hypervascular schwannoma (arrows), which is atypical for schwannomas.
-
Glomus jugulare. Digital subtraction angiogram shows a markedly hypervascular mass (arrow).