Practice Essentials
Tibial plateau fractures are periarticular knee fractures of the proximal tibia and account for 1% of all fractures. They may be associated with injury to nearby structures, including vasculature, nerves, ligaments, menisci, and adjacent compartments. [1, 2] Minimal tibial plateau fractures with no associated injuries can be safely managed nonoperatively, but this injury typically requires operative management. [3]
Although tibial plateau fracture was originally termed a bumper or fender fracture, only 25% of tibial plateau fractures result from impact with automobile bumpers. The most common mechanism of injury involves axial loading such as that caused by a fall. Other patterns of injury result from laterally directed forces or from a twisting injury. In all cases, force is directed from the femoral condyles onto the medial and lateral portions of the tibial plateau, resulting in fracture. In younger patients, the most common pattern of fracture is splitting, and in older, osteoporotic patients, depression fractures are more typical.
Schatzker classification
Schatzker et al proposed a classification system of condyle fractures based on the fracture pattern and fragment anatomy. This classification system, which is widely accepted and used today, divides these fractures into the following 6 types (see the first 2 images below) [4, 5] :
-
Type I - A wedge or split fracture of the lateral aspect of the plateau, usually as a result of valgus and axial forces; the wedge fragment is not compressed (depressed), because the underlying cancellous bone is strong; this pattern is usually seen in younger patients.
-
Type II - A lateral wedge or split fracture associated with compression; the mechanism of injury is similar to that of a type I fracture, but the underlying bone may be osteoporotic and unable to resist depression, or the force may have been greater.
-
Type III - A pure compression fracture of the lateral plateau; as a result of an axial force, the depression is usually located laterally or centrally, but it may involve any portion of the articular surface.
-
Type IV - A fracture that involves the medial plateau; as a result of either varus or axial compression forces, the pattern may be either split alone or split with compression; because this fracture involves the larger and stronger medial plateau, the forces causing this type are generally greater than those associated with types I, II, or III.
-
Type V - Includes split elements of both the medial and the lateral condyles and may include medial or lateral articular compression, usually as a result of a pure axial force occurring while the knee is in extension.
-
Type VI - A complex, bicondylar fracture in which the condylar components separate from the diaphysis; depression and impaction of fracture fragments are the rule; this pattern results from high-energy trauma and diverse combinations of forces.
(Examples of tibial plateau fractures are provided in the images below.)
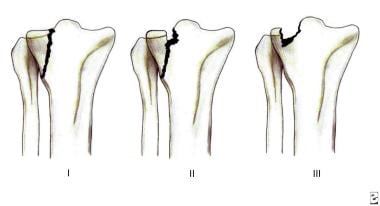 Tibial plateau fractures. Line drawings of Schatzker types I, II, and III tibial plateau fractures. Type I consists of a wedge fracture of the lateral tibial plateau, produced by low-force injuries. Type II combines the wedge fracture of the lateral plateau with depression of the lateral plateau. Type III fractures are classified as those with depression of the lateral plateau but no associated wedge fracture.
Tibial plateau fractures. Line drawings of Schatzker types I, II, and III tibial plateau fractures. Type I consists of a wedge fracture of the lateral tibial plateau, produced by low-force injuries. Type II combines the wedge fracture of the lateral plateau with depression of the lateral plateau. Type III fractures are classified as those with depression of the lateral plateau but no associated wedge fracture.
 Tibial plateau fractures. Line drawings of Schatzker types IV, V, and VI tibial plateau fractures. Type IV is similar to type I fracture, except that it involves the medial tibial plateau as opposed to the lateral plateau. Greater force is required to produce this type of injury. Type V fractures are termed bicondylar and demonstrate wedge fractures of both the medial and lateral tibial plateaus. Finally, type VI fractures consist of a type V fracture along with a fracture of the underlying diaphysis and/or metaphysis.
Tibial plateau fractures. Line drawings of Schatzker types IV, V, and VI tibial plateau fractures. Type IV is similar to type I fracture, except that it involves the medial tibial plateau as opposed to the lateral plateau. Greater force is required to produce this type of injury. Type V fractures are termed bicondylar and demonstrate wedge fractures of both the medial and lateral tibial plateaus. Finally, type VI fractures consist of a type V fracture along with a fracture of the underlying diaphysis and/or metaphysis.
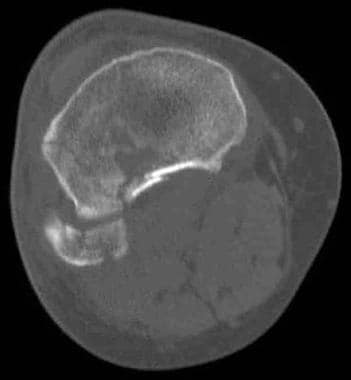
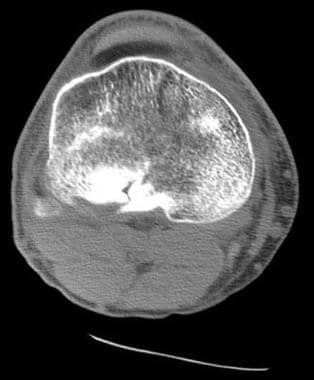 Tibial plateau fractures. CT image through the tibial plateau shows a fracture of the posterior aspect of the lateral tibial plateau, which is the source of the lipohemarthrosis.
Tibial plateau fractures. CT image through the tibial plateau shows a fracture of the posterior aspect of the lateral tibial plateau, which is the source of the lipohemarthrosis.
 Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
 Tibial plateau fractures. Radiograph of the knee shows lateral plateau splitting, a Schatzker I injury. There is no articular depression.
Tibial plateau fractures. Radiograph of the knee shows lateral plateau splitting, a Schatzker I injury. There is no articular depression.
Tibial plateau fractures are often associated with soft tissue injuries, with the lateral meniscus and the anterior cruciate ligament (ACL) being the most commonly affected structures. [6, 7] In a retrospective study of 265 patients with posterolateral tibia plateau fractures, the incidence of anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), lateral collateral ligament (LCL), medial collateral ligament (MCL), lateral meniscus, and medial meniscus injuries was assessed on magnetic resonance imaging (MRI). Anterior cruciate ligament and posterior cruciate ligament tears were present in 80% and 36%, respectively; LCL injuries were identified in 76% of patients, and 64% had MCL injuries. The incidence of lateral meniscus tears was 48%, and that of medial meniscus tears was 4%. [6]
Medial plateau injuries may result in fracture of the fibular head, which can injure the peroneal nerve or may be associated with popliteal artery occlusion. Patients may present with a knee effusion, pain, and joint stiffness. Finally, although severe fractures often are repaired surgically, both operatively and nonoperatively treated fractures are at risk of developing posttraumatic osteoarthritis as a result of ligamentous injuries with resultant instability, as well as articular discongruities, biomechanical alteration of normal compressive forces, and cartilage damage.
Imaging modalities
All imaging modalities should be analyzed for the specific pattern, shape, size, and location of different fragments of a tibial plateau fracture. The preferred examination consists of radiographs in multiple obliquities of the knee. [8] Typically, these include anteroposterior (AP), cross-table lateral, patellar (sunrise), and, possibly, oblique views. Cross-table lateral and AP may be the only views possible in the trauma suite. In this setting, the cross-table lateral radiograph may be the most important to detect occult fractures. The presence of these subtle fractures may be inferred by the presence of a lipohemarthrosis on the cross-table lateral radiograph, indicating disruption of an articular surface, most often the tibia. Nondepressed tibial plateau fractures occasionally are difficult to appreciate with standard radiographs. Plain films have a sensitivity of 85% for tibial plateau fractures. If there is a high degree of suspicion for tibial plateau fracture with negative plain radiographs, computed tomography (CT) scanning is indicated. CT assesses articular surface depression and comminution. It also delineates fracture pattern, size of fracture fragments, shapes, and locations for surgical planning. CT is typically faster and easier to obtain in an acute setting and can be used to alter fracture classification and treatment planning based on initial radiographs. Magnetic resonance imaging (MRI) is indicated to evaluate meniscal and ligamentous pathologies. [2]
If lipohemarthrosis is detected, an intra-articular fracture is present and must be located. In this situation, axial CT is an excellent tool for defining fracture anatomy using reconstructed images in the sagittal and coronal planes. The images below demonstrate the radiographic, CT, and MRI appearance of lipohemarthrosis.
 Tibial plateau fractures. Cross-table lateral radiograph of the knee shows the lipohemarthrosis within the suprapatellar bursa. The fracture itself is not seen well.
Tibial plateau fractures. Cross-table lateral radiograph of the knee shows the lipohemarthrosis within the suprapatellar bursa. The fracture itself is not seen well.
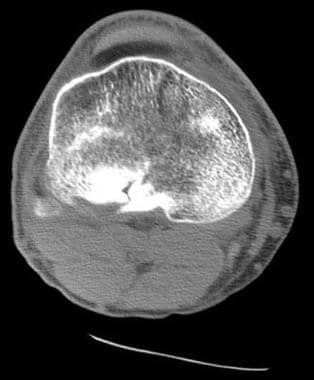 Tibial plateau fractures. CT image through the tibial plateau shows a fracture of the posterior aspect of the lateral tibial plateau, which is the source of the lipohemarthrosis.
Tibial plateau fractures. CT image through the tibial plateau shows a fracture of the posterior aspect of the lateral tibial plateau, which is the source of the lipohemarthrosis.
 Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
Computed tomography is used by most orthopedists to further characterize fractures of the tibial plateau and to assess depression of the tibia and degree of diastasis (splitting) of fractured parts to plan for surgical intervention. Generally, slice thickness should be minimized (1 mm is ideal), and a high-milliamperage-second (mAs) technique should be used. [9, 10, 11] Magnetic resonance imaging may be used as well for this determination but often is not readily available. Magnetic resonance imaging is excellent for depicting ligamentous and meniscal injuries. Arteriography (and possibly magnetic resonance angiography) may be used if popliteal artery injury is suspected. [12, 13, 14, 15, 16]
Brunner and colleagues found that CT scanning improved interobserver and intraobserver reliability of the Schatzker, Orthopaedic Trauma Association (OTA)/Arbeitsgemeinschaft für Osteosynthesefragen (AO), and Hohl and Moore classification systems for tibial plateau fractures. These 3 systems showed moderate interobserver reliability and good and moderate intraobserver reliability when evaluated only on the basis of findings on plain radiographs. Interobserver and intraobserver reliability improved significantly when CT was added. [17]
According to Mustonen and associates, although postoperative multidetector-row CT (MDCT) scanning of tibial plateau fractures is performed infrequently, in most cases it can reveal clinically significant information. In this study, the main indications for MDCT were assessment and follow-up of the joint articular surface and evaluation of fracture healing. Postoperative MDCT revealed additional clinically important information in 81% of patients, and 39% underwent reoperation. Orthopedic hardware caused no diagnostic problems with MDCT. [18]
Nuclear medicine studies are not used in the diagnosis of tibial plateau fractures unless a stress-type fracture is suspected or there is concern that osteomyelitis exists.
Type IV fractures involving the medial tibial plateau raise concern that the popliteal artery has been injured. These arterial injuries can be clinically silent or may present with decreased peripheral pulses. If clinical concern exists that a popliteal artery injury has occurred with any fracture type, an arteriogram (or possibly a magnetic resonance angiogram) can be obtained. Surgical manipulation of the tissues surrounding an injured popliteal artery can result in thrombosis with dire consequences, unless the thrombosis is addressed immediately. However, angiography is not used for the primary detection of tibial plateau fractures.
Radiography
Many methods have been developed to classify tibial plateau fractures, but all available classification systems for tibial plateau fractures are limited by their reliability and reproducibility. The Schatzker system has been found to have fair to substantial interobserver reliability. More sophisticated imaging modalities such as 2D and 3D CT typically improve reliability estimates. [19, 20, 21] Most fractures of the tibial plateau are diagnosed readily by conventional radiography. A false-negative radiograph may be encountered on the rare occasions in which a fracture is present but only a lipohemarthrosis is visualized. For these patients, CT or MRI is required to visualize the fracture.
(The Schatzker system is depicted in the images below. [8] )
 Tibial plateau fractures. Line drawings of Schatzker types IV, V, and VI tibial plateau fractures. Type IV is similar to type I fracture, except that it involves the medial tibial plateau as opposed to the lateral plateau. Greater force is required to produce this type of injury. Type V fractures are termed bicondylar and demonstrate wedge fractures of both the medial and lateral tibial plateaus. Finally, type VI fractures consist of a type V fracture along with a fracture of the underlying diaphysis and/or metaphysis.
Tibial plateau fractures. Line drawings of Schatzker types IV, V, and VI tibial plateau fractures. Type IV is similar to type I fracture, except that it involves the medial tibial plateau as opposed to the lateral plateau. Greater force is required to produce this type of injury. Type V fractures are termed bicondylar and demonstrate wedge fractures of both the medial and lateral tibial plateaus. Finally, type VI fractures consist of a type V fracture along with a fracture of the underlying diaphysis and/or metaphysis.
Type I fractures (demonstrated in the image below) are split fractures of the lateral tibial plateau and usually are seen in younger patients. No depression is seen at the articular surface.
 Tibial plateau fractures. Radiograph of the knee shows lateral plateau splitting, a Schatzker I injury. There is no articular depression.
Tibial plateau fractures. Radiograph of the knee shows lateral plateau splitting, a Schatzker I injury. There is no articular depression.
Type II fractures (shown in the images below) are split fractures with depression of the lateral articular surface; they typically are seen in older patients with osteoporosis.
 Tibial plateau fractures. Radiograph of the knee shows a fracture through the lateral tibial plateau with extension to the lateral tibial margin and slight depression at the articular surface. This is a Schatzker II injury.
Tibial plateau fractures. Radiograph of the knee shows a fracture through the lateral tibial plateau with extension to the lateral tibial margin and slight depression at the articular surface. This is a Schatzker II injury.
 Tibial plateau fractures. A different patient illustrates a Schatzker II injury with subtle lateral articular depression.
Tibial plateau fractures. A different patient illustrates a Schatzker II injury with subtle lateral articular depression.
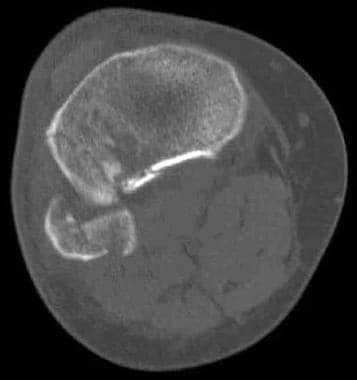 Tibial plateau fractures. Axial CT image through the tibial shows a fracture through the lateral tibial plateau with slight diastasis between the fragments. This is a Schatzker II injury.
Tibial plateau fractures. Axial CT image through the tibial shows a fracture through the lateral tibial plateau with slight diastasis between the fragments. This is a Schatzker II injury.
 Tibial plateau fractures. Axial CT image of the same patient as in the previous image shows the extent of the lateral tibial plateau fracture. In this case, it extends to the lateral tibial margin and an associated fibular head fracture is seen. This is a Schatzker II injury.
Tibial plateau fractures. Axial CT image of the same patient as in the previous image shows the extent of the lateral tibial plateau fracture. In this case, it extends to the lateral tibial margin and an associated fibular head fracture is seen. This is a Schatzker II injury.
Type III fractures (shown in the image below) are characterized by depression of the lateral tibial plateau, without splitting through the articular surface.
 Tibial plateau fractures. Oblique radiograph of the knee demonstrates a fracture of the lateral tibial plateau with slight depression. There is no associated wedge component. This is a Schatzker III injury.
Tibial plateau fractures. Oblique radiograph of the knee demonstrates a fracture of the lateral tibial plateau with slight depression. There is no associated wedge component. This is a Schatzker III injury.
Type IV fractures involve the medial tibial plateau and may be split fractures with or without depression.
Type V fractures are characterized by split fractures through both the medial and lateral tibial plateaus.
Type VI fractures (demonstrated in the images below) are caused by severe stress and result in dissociation of the tibial plateau region from the underlying diaphysis.
 Tibial plateau fractures. Radiograph of the knee reveals fractures through both the medial and the lateral tibial plateau along with a fibular head fracture and a fracture through the tibial metaphysis. This is a Schatzker VI injury.
Tibial plateau fractures. Radiograph of the knee reveals fractures through both the medial and the lateral tibial plateau along with a fibular head fracture and a fracture through the tibial metaphysis. This is a Schatzker VI injury.
 Tibial plateau fractures. Coronal reformatted CT. This image demonstrates a bicondylar fracture of the tibial plateau along with a fracture of the tibial diaphysis, a Schatzker VI fracture. Note the articular incongruity.
Tibial plateau fractures. Coronal reformatted CT. This image demonstrates a bicondylar fracture of the tibial plateau along with a fracture of the tibial diaphysis, a Schatzker VI fracture. Note the articular incongruity.
Computed Tomography
In most patients, computed tomography (CT) scanning mimics the findings of conventional radiography. With reconstruction of axial images into coronal and sagittal planes, precise localization of surgical landmarks and of all fracture fragments is obtained. CT is critical in formulating a surgical plan for Schatzker type IV, V, and VI fractures. [22]
Although, as previously mentioned, most fractures of the tibial plateau are diagnosed readily by conventional radiography, CT often is used with more complex fractures to confirm the anatomic relationships of fracture fragments. This is especially true at the articular surface of the tibia, where precise 3-dimensional anatomy is critical to the success of surgical repair. [23] Less-comminuted and depressed fractures may not require imaging by CT.
The value of CT lies in the speed and availability of the technique. In addition, most patients with extensive injuries undergo CT of other portions of the body in the trauma setting. With current scanners, image thickness of 1 mm or less is possible, which generally yields unequivocal depiction of fracture patterns. However, for a full depiction of soft tissue injury such as ligaments and menisci, MRI is superior. [14, 16]
False-negative errors can occur with CT when only axial imaging is used. If a fracture predominates in the axial plane, it may be overlooked by CT. However, in most instances, sagittal and coronal reconstructions of axial data, as shown in the images below, are used to avoid this problem. By reconstructing the initial data set into different planes, additional information such as articular depression and diastasis may be obtained easily. False positives are not common with CT.
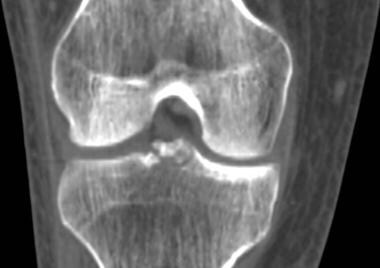 Tibial plateau fractures. Coronal reformatted CT. Initial narrow collimation axial CT data can be reconstructed into sagittal and coronal planes. This technique is useful to evaluate for fracture lines parallel to the axial imaging plane, degree of articular depression, and degree of diastasis between major fracture fragments. The best reconstructions are made when the initial data set consists of axial images of less than 2 mm thickness. In this particular case, an axial data set of 1 mm images was reconstructed into this coronal image demonstrating fractures of the tibial spines.
Tibial plateau fractures. Coronal reformatted CT. Initial narrow collimation axial CT data can be reconstructed into sagittal and coronal planes. This technique is useful to evaluate for fracture lines parallel to the axial imaging plane, degree of articular depression, and degree of diastasis between major fracture fragments. The best reconstructions are made when the initial data set consists of axial images of less than 2 mm thickness. In this particular case, an axial data set of 1 mm images was reconstructed into this coronal image demonstrating fractures of the tibial spines.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is very sensitive to the presence of osseous injury. Injuries to osseous structures manifest as areas of edema within bone marrow. However, fractures through the cortex are less well depicted because cortical bone appears as an area of low signal (generally black) on MRI sequences. Thus, fractures through cortical bone can be difficult to depict with MRI. Complex and comminuted fractures with multiple cortical fragments are exceedingly difficult to analyze via MRI.
False negatives with MRI are uncommon. MRI is used routinely for detection of occult fractures because of its superior depiction of bone marrow edema—a direct indicator of osseous injury. False-negative information may result when MRI data are analyzed for the presence of cortical fractures. False-negative and false-positive errors may occur if incorrect MRI sequences are chosen. In general, a fluid-sensitive sequence such as short tau inversion recovery, rather than a simple T2-weighted sequence, is best to detect bone marrow edema.
In a study by Kode and colleagues investigating the usefulness of CT and MRI in visualizing fracture patterns, [24] MRI was often found to be superior to CT, unless the fracture was extremely comminuted. Meniscal injuries, as well as injuries to the collateral and cruciate ligaments, may be depicted better with MRI than with CT. [15, 16, 25]
(See the image below.)
 Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
-
Tibial plateau fractures. Line drawings of Schatzker types I, II, and III tibial plateau fractures. Type I consists of a wedge fracture of the lateral tibial plateau, produced by low-force injuries. Type II combines the wedge fracture of the lateral plateau with depression of the lateral plateau. Type III fractures are classified as those with depression of the lateral plateau but no associated wedge fracture.
-
Tibial plateau fractures. Line drawings of Schatzker types IV, V, and VI tibial plateau fractures. Type IV is similar to type I fracture, except that it involves the medial tibial plateau as opposed to the lateral plateau. Greater force is required to produce this type of injury. Type V fractures are termed bicondylar and demonstrate wedge fractures of both the medial and lateral tibial plateaus. Finally, type VI fractures consist of a type V fracture along with a fracture of the underlying diaphysis and/or metaphysis.
-
Tibial plateau fractures. Cross-table lateral radiograph of the knee shows the lipohemarthrosis within the suprapatellar bursa. The fracture itself is not seen well.
-
Tibial plateau fractures. CT image through the tibial plateau shows a fracture of the posterior aspect of the lateral tibial plateau, which is the source of the lipohemarthrosis.
-
Tibial plateau fractures. Axial CT image through the knee shows a layering lipohemarthrosis.
-
Tibial plateau fractures. MRI of the knee in a patient with tibial plateau fracture and lipohemarthrosis. Three layers of effusion are demonstrated on this proton density sequence: fat, red blood cells, and serum. Low-signal intensity in the tibial plateau corresponds to the site of fracture.
-
Tibial plateau fractures. Radiograph of the knee shows lateral plateau splitting, a Schatzker I injury. There is no articular depression.
-
Tibial plateau fractures. Radiograph of the knee shows a fracture through the lateral tibial plateau with extension to the lateral tibial margin and slight depression at the articular surface. This is a Schatzker II injury.
-
Tibial plateau fractures. A different patient illustrates a Schatzker II injury with subtle lateral articular depression.
-
Tibial plateau fractures. Axial CT image through the tibial shows a fracture through the lateral tibial plateau with slight diastasis between the fragments. This is a Schatzker II injury.
-
Tibial plateau fractures. Axial CT image of the same patient as in the previous image shows the extent of the lateral tibial plateau fracture. In this case, it extends to the lateral tibial margin and an associated fibular head fracture is seen. This is a Schatzker II injury.
-
Tibial plateau fractures. Oblique radiograph of the knee demonstrates a fracture of the lateral tibial plateau with slight depression. There is no associated wedge component. This is a Schatzker III injury.
-
Tibial plateau fractures. Coronal reformatted CT. Initial narrow collimation axial CT data can be reconstructed into sagittal and coronal planes. This technique is useful to evaluate for fracture lines parallel to the axial imaging plane, degree of articular depression, and degree of diastasis between major fracture fragments. The best reconstructions are made when the initial data set consists of axial images of less than 2 mm thickness. In this particular case, an axial data set of 1 mm images was reconstructed into this coronal image demonstrating fractures of the tibial spines.
-
Tibial plateau fractures. Radiograph of the knee reveals fractures through both the medial and the lateral tibial plateau along with a fibular head fracture and a fracture through the tibial metaphysis. This is a Schatzker VI injury.
-
Tibial plateau fractures. Radiograph of the knee shows a different Schatzker VI fracture.
-
Tibial plateau fractures. Axial CT image demonstrates the extensive fractures of both the lateral and medial aspects of the tibial plateau, a Schatzker VI injury.
-
Tibial plateau fractures. Coronal reformatted CT. This image demonstrates a bicondylar fracture of the tibial plateau along with a fracture of the tibial diaphysis, a Schatzker VI fracture. Note the articular incongruity.












