Practice Essentials
Thyroid nodules are common, perhaps existing in almost half the population, as determined using ultrasonography (US). Only 4-7% of thyroid nodules detected with US are palpable in the adult population in the United States, with women affected more frequently than men. Although the thyroid is the most common endocrine organ to undergo malignant degeneration, thyroid carcinoma accounts for only 1% of diagnosed neoplasms in the United States each year. [1, 2] Thyroid cancer is rare; the annual detection rate of clinically significant thyroid cancer in the general population is only 0.004%. Only 5-10% of thyroid cancers are clinically palpable. [3, 4]
In a study by Davies et al utilizing data from the National Cancer Institute's Surveillance, Epidemiology, and End Results Program and the National Vital Statistics System, the rate of thyroid cancer in US adults was found to have risen from 4.9 per 100,000 individuals to 14.3 per 100,000 between 1975 and 2009, and in women, the increase in thyroid cancer was almost 4 times that in men. [5]
Palpable nodules can be visualized as areas of increased (hot) or decreased (cold) tracer activity. However, terms such as hot nodules and cold nodules are misleading unless the nodule can be clearly delineated in several projections. A nonfunctioning (cold) nodule placed in the center of a lobe with functioning normal tissue superficial to it may appear as warm on scans because of integrated activity with depth. Unless oblique views are imaged, the presence of activity concentration cannot be definitively determined. Therefore, nodules should be identified as being functioning (hot), nonfunctioning (cold), or photon deficient. Hot nodules (which are typically adenomas) are more often benign than cold lesions are.
The classification of thyroid neoplasms has been significantly revised in the last 20 years, and the changes reflect an increased understanding of the prognosis and histologic characteristics of the tumors. Among asymptomatic patients, 7-21% have palpable nodules found on routine clinical examination. US can be used to identify many more nonpalpable nodules, and it can depict thyroid cysts as small as 2 mm and solid nodules as small as 3 mm. [6, 7]
A number of organizations have proposed and published classifications and guidelines for thyroid nodules, including the American Thyroid Association, the Society of Radiologists in Ultrasound, the National Comprehensive Cancer Network, the American College of Radiology, the Thyroid Imaging Reporting and Data System, and the British Thyroid Association. These guidelines and classifications have been compared and contrasted in numerous studies. [8, 9, 10, 11, 12, 13, 14, 15, 16, 17] Virtually all the guidelines recommend ultrasound evaluation and measurement of serum thyroid-stimulating hormone (TSH) levels to determine whether fine-needle aspiration biopsy (FNAB) is indicated.
Sonograms in 40% of the general adult population demonstrate single or multiple nodules. In an autopsy series, 49% of patients who had had clinically normal thyroid glands were found to have one or more grossly visible nodules, whereas the incidence of malignancy in the same autopsy series was 2-4%. [18, 19]
At examination, the challenge is to differentiate the few clinically significant nodules from the many benign ones. Thyroid nodules are usually clearly identified by using US. No single US criterion is reliable for differentiating all benign thyroid nodules from malignant ones, but many US features may aid in predicting the benign or malignant nature of a given nodule. [20, 21, 22, 23, 24]
Preferred examination
Ulatrasonography is usually the first modality used to investigate a palpable thyroid nodule and in searching for a primary lesion in a patient with systemic metastases. US may be the only examination required in cases of hemorrhagic cyst and multinodular goiter. Doppler US is an extension of US and provides valuable information regarding the vascularity of nodules. Most intervention in the thyroid, such as fine-needle aspiration (FNA) and guided thyroid ablation, are performed under US guidance.
Currently, scintigraphy is reserved for characterizing functioning nodules and for staging follicular and papillary carcinomas. Lymphoma of the thyroid is the only gallium-67–avid thyroid nodule.
Plain radiographs are used to detect retrosternal thyroid extension, thyroid calcification, bony or mediastinal lymph nodes, and lung metastases.
Computed tomography (CT) scanning is an effective method for detecting regional and distant metastasis from thyroid cancer.
Magnetic resonance imaging (MRI) has a limited role in characterizing thyroid nodules, although it appears to be effective in the diagnosis of cervical lymph node metastasis.
Percutaneous needle aspiration remains the key procedure in the diagnosis of thyroid lymphoma; however, thyroid lymphoma's differentiation from thyroiditis occasionally can be difficult. US helps in diagnosing thyroid lymphoma most accurately, and CT helps in staging the disease most accurately. However, MRI also can be useful in staging the lymphoma. A tissue-specific diagnosis of a lymphoma can be achieved by using US-guided FNA. [25, 26]
Limitations of techniques
In the past, radionuclide imaging was performed to differentiate malignant from benign lesions. On radionuclide imaging, 4% of hot nodules are shown to contain tumor, compared with 16% of cold nodules. [27] Thus, radionuclide imaging is unreliable in excluding or confirming the presence of cancer.
Technetium-99m pertechnetate, an inexpensive and readily available isotope, delivers a low dose of radiation because of its 6-hour half-life; it has a favorable decay scheme without particulate emission. A gamma camera using a 140-keV photon is ideal for imaging.
The disadvantages of technetium-99m pertechnetate studies are that they can delineate only the trapping function and not organification, and 3-dimensional distortion occurs with pinhole imaging and decreased sensitivity in the mediastinum.
Currently, iodine-123 is the radioisotope of choice. The 13.3-hour half-life, the 159-keV principal photon, and the absence of particulate emission allow for good imaging with modest patient exposure. However, this isotope is cyclotron produced and relatively expensive, and the short half-life necessitates frequent shipments from the producer. Metastatic cancer is imaged well with iodine-123 because one half of papillary carcinomas and two thirds of follicular carcinomas are sufficiently iodine avid to allow their visualization.
US is an alternative method and can be used to evaluate local tumor recurrence because, unlike iodine-123 scintigraphy, it does not require the cessation of thyroid hormone therapy for as long as 5-6 weeks.
Gallium-67 has not enabled sufficient differentiation between the degree of uptake in malignant lesions and that of benign lesions to warrant its routine use, but it appears to be useful when thyroid lymphoma is suspected. US is the most sensitive method for diagnosing intrathyroid lesions; it can depict 2-mm cystic lesions and 3-cm solid intrathyroid lesions. The challenge is to differentiate a few malignant nodules from common benign nodules, because no single US criterion can be used to reliably differentiate all benign thyroid nodules from malignant ones. However, many US features may aid in predicting the benign or malignant nature of a given nodule.
As with MRI, CT is not sensitive in the prediction of intrathyroid lesions; however, it is useful for evaluating lymphadenopathy, local tumor extension, and extension into the mediastinum or retrotracheal region. Guided FNA provides specimens for cytologic studies. The procedure is safe and inexpensive and provides direct information.
(See the images below.)
 Coned apical radiograph of the upper thorax shows curvilinear calcification in a thyroid adenoma, at the root of the neck, on the right side.
Coned apical radiograph of the upper thorax shows curvilinear calcification in a thyroid adenoma, at the root of the neck, on the right side.
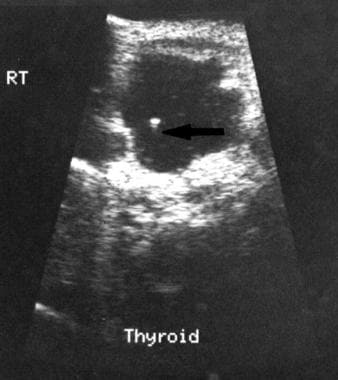
 Sonogram demonstrates a benign cystic lesion in the thyroid, with a surrounding halo and ragged walls.
Sonogram demonstrates a benign cystic lesion in the thyroid, with a surrounding halo and ragged walls.
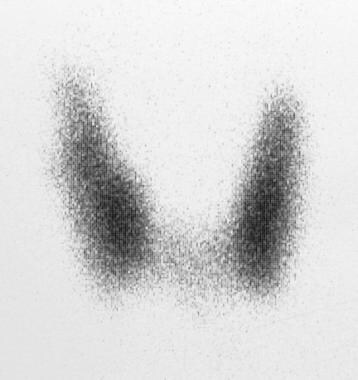
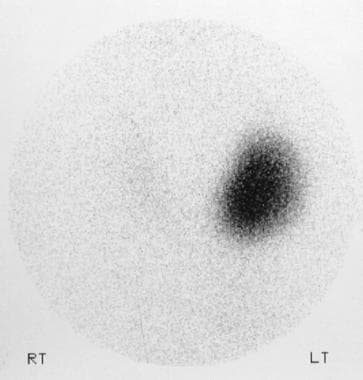
 Technetium-99m pertechnetate thyroid scan shows a large cold nodule in the left lobe of the thyroid and a further, smaller cold nodule in right lobe.
Technetium-99m pertechnetate thyroid scan shows a large cold nodule in the left lobe of the thyroid and a further, smaller cold nodule in right lobe.
 A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously. On routine follow-up examination, a mass was felt in the thyroid. Coronal, T1-weighted magnetic resonance imaging scan shows a carcinoma recurrence (R) and lymph node (L) metastases.
A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously. On routine follow-up examination, a mass was felt in the thyroid. Coronal, T1-weighted magnetic resonance imaging scan shows a carcinoma recurrence (R) and lymph node (L) metastases.
Radiography
The role of plain radiography in the evaluation of thyroid disease is limited. Plain radiographs can show soft-tissue masses and tracheal deviation. Retrosternal extension and metastatic lung disease also can be detected on a chest radiograph. (See the images below.)
 Coned apical radiograph of the upper thorax shows curvilinear calcification in a thyroid adenoma, at the root of the neck, on the right side.
Coned apical radiograph of the upper thorax shows curvilinear calcification in a thyroid adenoma, at the root of the neck, on the right side.
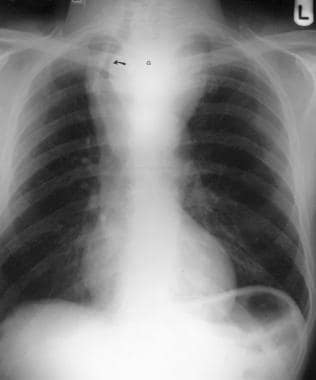 Posteroanterior chest radiograph shows a large retrosternal goiter (G) that displaces the trachea to the left (arrow).
Posteroanterior chest radiograph shows a large retrosternal goiter (G) that displaces the trachea to the left (arrow).
 Plain anteroposterior radiograph of the neck shows punctate calcification to the right of the cervical spine (straight arrow) and further multiple conglomerates of calcification at the root of the neck (curved arrow), also on the right.
Plain anteroposterior radiograph of the neck shows punctate calcification to the right of the cervical spine (straight arrow) and further multiple conglomerates of calcification at the root of the neck (curved arrow), also on the right.
 Standard posteroanterior chest radiograph in the same patient as in the previous image shows widening of the superior mediastinum on the right in a lobulated fashion.
Standard posteroanterior chest radiograph in the same patient as in the previous image shows widening of the superior mediastinum on the right in a lobulated fashion.
 Plain radiograph of the upper abdomen in the same patient as in the previous 2 images shows multiple conglomerates of punctate calcification in the right hypochondrium encroaching on the left hypochondrium. The final diagnosis was a medullary carcinoma of the thyroid (calcified), lymph node metastases at the root of the neck (calcified), right superior mediastinal metastases, and gross hepatomegaly with multiple calcified hepatic metastases.
Plain radiograph of the upper abdomen in the same patient as in the previous 2 images shows multiple conglomerates of punctate calcification in the right hypochondrium encroaching on the left hypochondrium. The final diagnosis was a medullary carcinoma of the thyroid (calcified), lymph node metastases at the root of the neck (calcified), right superior mediastinal metastases, and gross hepatomegaly with multiple calcified hepatic metastases.
 Posteroanterior chest radiograph shows a large, lytic, expanding metastasis in the anterior aspects of the right fifth and sixth ribs, secondary to an anaplastic thyroid carcinoma in an 85-year-old woman. Note displacement of the trachea to the left by a mass lesion at the root of the neck.
Posteroanterior chest radiograph shows a large, lytic, expanding metastasis in the anterior aspects of the right fifth and sixth ribs, secondary to an anaplastic thyroid carcinoma in an 85-year-old woman. Note displacement of the trachea to the left by a mass lesion at the root of the neck.
 Anteroposterior chest radiograph of an 86-year-old woman who had been unwell for a few months and was losing weight. The radiograph shows a right superior mediastinal mass.
Anteroposterior chest radiograph of an 86-year-old woman who had been unwell for a few months and was losing weight. The radiograph shows a right superior mediastinal mass.
Calcifications in thyroid tumors can be seen on plain radiographs. Stippled calcification in the thyroid is suggestive of carcinoma, whereas peripheral rim calcification suggests a benign lesion. However, because of the overlap in findings, the sensitivity is reduced. Medullary carcinomas and their metastases can become calcified. Plain radiographs can show metastases in bone; these are vascular and can cause expansion of the bone.
Degree of confidence
Plain radiograph findings are neither sensitive nor specific. Retrosternal goiters caused by tracheal stenosis that are large enough to cause symptoms may be shown on plain radiographs, but CT is more sensitive and specific. Findings of calcification in thyroid cancers overlap with those of benign disease. Similarly, lung and bone metastases can be derived from several primary sites.
False positives/negatives
Tracheal stenosis or deviation can result from causes other than retrosternal goiters. Similarly, calcification in the neck can have several causes other than thyroid cancer.
Computed Tomography
Similarly to MRI, CT is not a sensitive technique for demonstrating intrathyroid lesions. However, CT is useful in evaluating lymphadenopathy, local tumor extension, and extension into the mediastinum or retrotracheal region. Therefore, US is used for primary detection of intrathyroid lesions, and CT or MRI is used for staging. [28, 29] Attempts to differentiate benign from malignant nodules by measuring the iodine content and enhancement characteristics of the nodules on CT scans have been unsuccessful. CT scans of thryoid nodules are depicted in the images below.
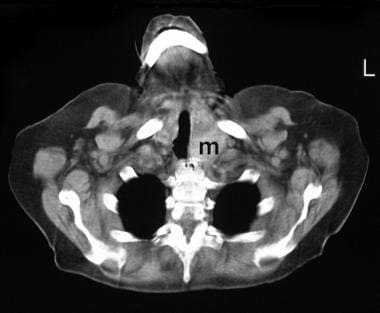 Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass (m) at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta.
Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass (m) at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta.
 Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass (m) at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta (same patient as in the previous image).
Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass (m) at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta (same patient as in the previous image).
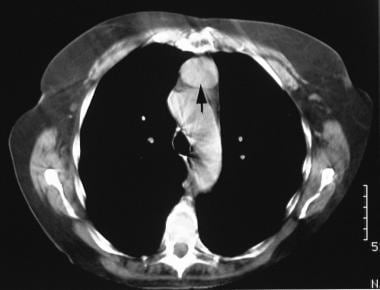 Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta (arrow) (same patient as in the previous 2 images).
Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta (arrow) (same patient as in the previous 2 images).
 Computed tomography scan shows a mass in the posterior mediastinum (P), which displaces the air-filled esophagus to the right (arrow) (same patient as in the previous 3 images).
Computed tomography scan shows a mass in the posterior mediastinum (P), which displaces the air-filled esophagus to the right (arrow) (same patient as in the previous 3 images).
Degree of confidence
CT of the thyroid is neither sensitive enough nor specific enough to allow the characterization of thyroid nodules. Thyroid cancer is suggested when certain patterns of calcification are seen in a thyroid mass and when extension to the surrounding soft tissues is visualized. Regional lymphadenopathy in association with a thyroid mass also is suggestive of thyroid malignancy.
False positives/negatives
Thyroid cancers may be missed on CT scans in the presence of a multinodular goiter. An intrathyroidal parathyroid gland and/or adenoma may lead to a false-positive diagnosis of thyroid cancer.
Magnetic Resonance Imaging
MRI is not as sensitive as US in depicting intrathyroid lesions. Early optimism regarding the use of MRI in the diagnosis of intrathyroid lesions is fading. However, MRI is helpful in the evaluation of local extension of thyroid neoplasms or the spread of disease into the mediastinum or retrotracheal region (see the images below). In addition, MRI is useful in assessing lymphadenopathy. High–field-strength and specially configured coils have improved the resolution of MRI.
 A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously. On routine follow-up examination, a mass was felt in the thyroid. Coronal, T1-weighted magnetic resonance imaging scan shows a carcinoma recurrence (R) and lymph node (L) metastases.
A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously. On routine follow-up examination, a mass was felt in the thyroid. Coronal, T1-weighted magnetic resonance imaging scan shows a carcinoma recurrence (R) and lymph node (L) metastases.
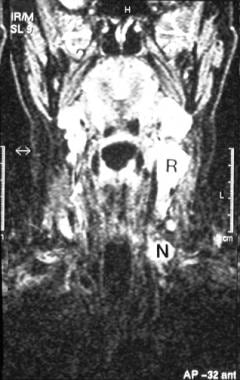 A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously (same patient as in the previous image). On routine follow-up examination, a mass was felt in the thyroid. Coronal, short-tau inversion recovery magnetic resonance imaging scan shows carcinoma recurrence (R) and lymph node (L) metastases.
A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously (same patient as in the previous image). On routine follow-up examination, a mass was felt in the thyroid. Coronal, short-tau inversion recovery magnetic resonance imaging scan shows carcinoma recurrence (R) and lymph node (L) metastases.
Thyroid lymphoma
Once the diagnosis is made, MRI is suggested for staging the cancer, including the assessment of adenopathy and esophageal involvement. On T2-weighted MRIs, the lesions tend to be homogeneous and isointense to hyperintense as compared with normal tissue. (Typically, however, the lesions are isointense to normal thyroid tissue, with more T1 weighting in approximately one third of the patients.) Tracheal compression, extrathyroidal extension, and the presence of a pseudocapsule are described.
Lymph node involvement is depicted equally well by MRI and CT, and both are superior to US. Tumor invasion of the esophagus is demonstrated well on MRIs and CT scans but not on sonograms.
Gallium-67 scintigraphy is a useful adjunct to imaging because thyroid lymphoma is the only thyroid malignancy in which the uptake of the radionuclide is reported.
Magnetic resonance spectroscopy
Magnetic resonance spectroscopy has been tried with FNA and surgical specimens. Performing hydrogen spectroscopy at 360 MHz has demonstrated a ratio of the peaks at 1.7 and 0.9 ppm, and it can be used to differentiate benign from malignant lesions. Values higher than a ratio of 1.1 are normal, and ratios lower than 1.1 indicate malignancy. In addition, normal tissue can be distinguished from papillary and medullary carcinoma, with a sensitivity of approximately 95%. The employment of this technique may be useful in differentiating malignant from benign follicular lesions when cytologic analysis is difficult.
Degree of confidence
The specificity of MRI is not adequate to preclude further imaging or FNA. Once the diagnosis has been achieved by using alternative methods, MRI is particularly good for the detection of tumoral extension into the surrounding tissues, particularly the trachea and esophagus.
False positives/negatives
The differentiation of the various thyroid nodules localized to the thyroid gland can be difficult with MRI. A thyroid carcinoma in a multinodular goiter may be missed.
Ultrasonography
According to the American Thyroid Association, ultrasound is the most important imaging modality in evaluating thyroid cancer, and ultrasound-guided fine-needle aspiration of suspicious lymph nodes may be useful in guiding the extent of surgery. [30, 31] US is the most sensitive method for diagnosing intrathyroid lesions (see the images below). It can depict 2-mm cystic lesions and 3-mm solid intrathyroid lesions. The challenge is differentiating a few malignant nodules from common benign nodules. Despite US's ability to clearly identify nodules, no single US criterion is reliable in differentiating benign ones from malignant thyroid nodules. Even so, many US features may aid in predicting the benign or malignant nature of a given nodule. [32, 33, 34, 35, 36, 37]
 Repeat 3-month follow-up sonogram in a 53-year-old woman with a sudden onset of pain in the anterior part of the neck shows that the septa have resolved. However, debris and strands are noted at the bottom of the cyst (same patient as in the previous image).
Repeat 3-month follow-up sonogram in a 53-year-old woman with a sudden onset of pain in the anterior part of the neck shows that the septa have resolved. However, debris and strands are noted at the bottom of the cyst (same patient as in the previous image).
 Further 3-month follow-up sonogram shows a considerable reduction in the size of the cyst, with a tiny debris level at the base of the cyst, in a 53-year-old woman with a sudden onset of pain in the anterior part of the neck. The final diagnosis was hemorrhage in a benign cyst (same patient as in the previous 2 images).
Further 3-month follow-up sonogram shows a considerable reduction in the size of the cyst, with a tiny debris level at the base of the cyst, in a 53-year-old woman with a sudden onset of pain in the anterior part of the neck. The final diagnosis was hemorrhage in a benign cyst (same patient as in the previous 2 images).
 Sonogram demonstrates a benign cystic lesion in the thyroid, with a surrounding halo and ragged walls.
Sonogram demonstrates a benign cystic lesion in the thyroid, with a surrounding halo and ragged walls.
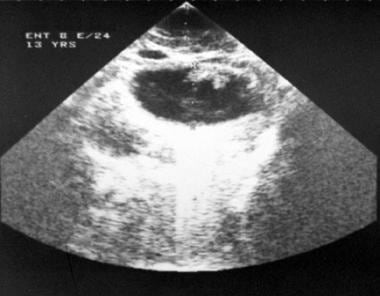 Sonogram demonstrates thyroid cystic lesions in a 13-year-old female adolescent with cystic papillary thyroid carcinoma.
Sonogram demonstrates thyroid cystic lesions in a 13-year-old female adolescent with cystic papillary thyroid carcinoma.
Most cystic lesions are benign masses that contain internal debris with a solid component that is hyperechoic relative to the adjacent thyroid tissue. Typically, benign nodules are well defined (96% benign). Lesions demonstrating eggshell calcification and a thin echolucent halo around the entire lesion are most often benign. Some authors have found that the halo sign is present in 21-33% of thyroid cancers.
Typically, malignant nodules are mostly solid and hypoechoic, with irregular margins and, at times, fine punctate calcification in the nodule, particularly in papillary carcinomas. Thyroid cancer has a hypoechoic texture, as compared with that of a normal thyroid gland, because a malignancy contains many cells that lack colloid. Carcinoma is hypoechoic in 68-100% of patients; however, a hypoechoic nodule is more likely to be benign than malignant, because benign nodules are highly prevalent in the general population. Recent research has revealed a correlation between osteopontin messenger RNA expression and the formation of microcalcification seen on US in papillary thyroid carcinomas. [38]
Considerable overlap may exist between benign nodules and malignant nodules. Some malignant nodules can have a cystic component. Cystic degeneration is reported in 4-33% of thyroid cancers.
A retrospective review of 624 patients examined the usefulness of surgeon-performed US to predict benign thyroid nodules. About 10% of patients were found to have benign nodules (classified as 1-4 cm, isoechoic, with regular borders, a cystic component, and no microcalcifications) through this procedure, leading the authors to conclude that patients without clinical risk factors and significant features of benignity can forego further fine needle aspiration and thyroid lobectomy and can be monitored through follow-up US examinations. [39]
Solid subcentimeter nodules that are taller than wide, are hypoechoic or markedly hypoechoic, and have coarse microcalcifications and macrocalcifications are associated with a risk of malignancy, indicating the need for further assessment. [40]
Caution should be taken in relying on US features alone.
Thyroid cyst
On sonograms, thyroid cysts are anechoic, fluid-filled, smooth-walled structures. Most cysts are colloid-filled, dilated macrofollicles, which represent colloid accumulation in goiter. Simple cysts of the thyroid are rare. Cysts with irregular walls and particulate fluid content usually represent hemorrhagic colloid cysts; hemorrhagic adenoma (30% of cases); necrotic papillary carcinoma (15% of cases); liquefaction necrosis in adenoma or goiter; thyroid abscess; and, occasionally, a cystic parathyroid tumor. Some colloid cysts have a characteristic US appearance; in addition to the well-defined cyst, several echogenic foci with comet tails are visualized in the cyst. [41, 42]
Thyroid lymphoma
On US, a thyroid lymphoma has the appearance of a hypoechoic mass, often a large one with lobulated margins and large, anechoic necrotic areas. Doppler US findings are unremarkable and are comparable to those of an undifferentiated carcinoma. Signs of cervical invasion in the late stages also are similar to those of an undifferentiated thyroid carcinoma; however, thyroid tissue surrounding undifferentiated tumors is a normal finding, whereas tissue surrounding lymphomas shows evidence of chronic thyroiditis.
Thyroid metastases
Involvement can be diffuse or focal. In diffuse disease, a heterogeneous hypoechoic pattern resembles that of thyroid lymphoma. Focal disease is usually confined to the lower pole, which is typically large and appears solid, well defined, noncalcified, and hypoechoic. Color Doppler images may occasionally show hypervascularity.
Color Doppler imaging
Color Doppler US has been applied to the evaluation of thyroid nodules, but again, many similarities are noted between the appearance of benign nodules and that of malignant nodules. No consistent correlation has been found between the pathologic findings and either the presence of internal flow or its amount. Color Doppler findings depend more on lesion size than on the histologic features. In fact, papillary carcinomas are usually less vascular than benign lesions. Cold nodules demonstrated with scintigraphy are usually hypervascular at the periphery and internally hypovascular. Most nodules with this pattern of vascularity are benign. [43]
Warm nodules demonstrated on scintigraphy are always internally and peripherally hypervascular, with a significant increase in blood velocity in the vessels that supply them compared with that of vessels in the normal parenchyma. When a cold nodule is internally hypervascular, the likelihood of malignancy increases. Papillary carcinoma can be hypovascular. If associated with Hashimoto thyroiditis, the tumor can be seen as a hypovascular area surrounded by an intensely hypervascular parenchyma.
Degree of confidence
Typical benign nodules are well defined, mostly cystic, and hyperechoic relative to adjacent parenchyma (96% benign). These nodules have eggshell calcification and a thin, echolucent halo around the entire lesion (in many benign nodules), and they always contain internal debris.
Typical malignant nodules have irregular margins at times and are solid (most nodules) and mostly hypoechoic. Fine punctate calcification may be present within the nodule, particularly in papillary carcinoma.
False positives/negatives
Significant overlap exists between benign and malignant thyroid nodules; therefore, FNA biopsy is necessary in many cases with equivocal findings.
Nuclear Imaging
In the past, radionuclide imaging was performed to differentiate malignant from benign lesions. With radionuclide imaging, 4% of hot nodules are shown to contain tumor, compared with 16% of cold nodules. Thus, radionuclide imaging is unreliable in excluding or confirming the presence of cancer. Currently, several radionuclides are used in thyroid scintigraphy. (See the images below.) [44, 45]
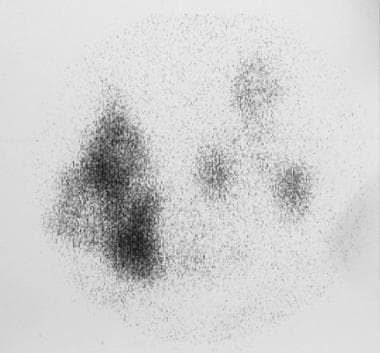
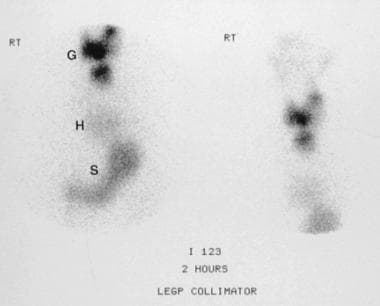 Iodine-123 thyroid scan shows that a mass is a multinodular goiter (G). The posterior mediastinal mass is a hiatus hernia (H); the stomach (S) is shown. Further investigation revealed that thyrotoxicosis was the cause of the patient's symptoms.
Iodine-123 thyroid scan shows that a mass is a multinodular goiter (G). The posterior mediastinal mass is a hiatus hernia (H); the stomach (S) is shown. Further investigation revealed that thyrotoxicosis was the cause of the patient's symptoms.
 Technetium-99m pertechnetate thyroid scan demonstrates an autonomous nodule with increased activity. Uptake in the remainder of the thyroid is suppressed.
Technetium-99m pertechnetate thyroid scan demonstrates an autonomous nodule with increased activity. Uptake in the remainder of the thyroid is suppressed.
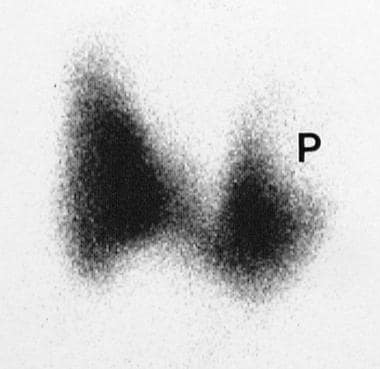
 Technetium-99m pertechnetate thyroid scan demonstrates intense activity in a large thyroid gland in a patient who was hypothyroid. The patient had Pendred syndrome. Note the pyramidal lobe (P).
Technetium-99m pertechnetate thyroid scan demonstrates intense activity in a large thyroid gland in a patient who was hypothyroid. The patient had Pendred syndrome. Note the pyramidal lobe (P).
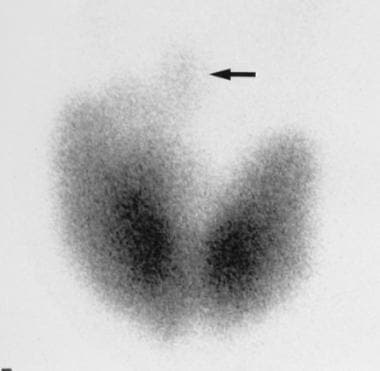 Technetium-99m pertechnetate thyroid scan demonstrates a thyrotoxic goiter. Note the pyramidal lobe (arrow).
Technetium-99m pertechnetate thyroid scan demonstrates a thyrotoxic goiter. Note the pyramidal lobe (arrow).
 Technetium-99m pertechnetate thyroid scan demonstrates a cold nodule in the left lobe of the thyroid (C).
Technetium-99m pertechnetate thyroid scan demonstrates a cold nodule in the left lobe of the thyroid (C).
 Technetium-99m pertechnetate thyroid scan shows a photon-deficient mass in the upper pole of the left lobe in a 53-year-old woman with a sudden onset of pain in the anterior aspect of the neck.
Technetium-99m pertechnetate thyroid scan shows a photon-deficient mass in the upper pole of the left lobe in a 53-year-old woman with a sudden onset of pain in the anterior aspect of the neck.
Technetium-99m pertechnetate study
This radionuclide delivers a low dose of radiation because of its 6-hour half-life and favorable decay scheme without particulate emission. The 140-keV photon is ideal for imaging with the gamma camera. The isotope is inexpensive and readily available. The disadvantages are that the technique can delineate only the trapping function and not organification. With pinhole imaging, 3-dimensional distortion of the image occurs and sensitivity is decreased in the mediastinum.
Iodine-123 study
Currently, iodine-123 is the radioisotope of choice. The 13.3-hour half-life, 159-keV principal photon, and absence of particulate emission allow for good imaging with modest patient exposure. However, this isotope is cyclotron produced and relatively expensive, and the short half-life necessitates frequent shipments from the producer. Scintigraphy with iodine-123 is the preferred modality for functional evaluation of the thyroid. Palpable nodules can be visualized as areas of increased (hot) or decreased (cold) tracer activity.
Terms such as hot nodules and cold nodules are misleading unless the nodule can be clearly delineated in several projections. A nonfunctioning (cold) nodule placed in the center of a lobe with functioning normal tissue superficial to it may appear as warm on scans because of integrated activity with depth. Unless oblique views are obtained, the presence of activity concentration cannot be determined with certainty. Therefore, nodules should be identified as being functioning (hot), nonfunctioning (cold), or photon deficient.
Most nodules are cold; hot nodules account for only about 10% of the lesions. A hot nodule is usually a benign lesion; typically, it is an adenoma. Hot nodules have a risk of malignancy of approximately 1-4%.
All thyroid carcinomas are likely to be cold, as are lymphoma, metastases, and many benign thyroid abnormalities, such as adenomas, nodular goiter, focal thyroiditis, and cysts. As a result of the relative frequencies of these benign abnormalities, most cold nodules are benign. Approximately 80% of cold lesions are benign.
Low iodine-123 uptake in a single palpable nodule indicates that it has a risk of malignancy of approximately 10-25%, but this percentage decreases to only 1-3% if multiple nodules are demonstrated at scintigraphy. The risk of cancer in nodules with increased technetium-99m pertechnetate uptake is approximately 29%, whereas the risk of cancer in nodules with increased iodine-123 uptake is only 4%.
A thyroid nodule may have decreased or absent iodine organification. In this case, pertechnetate uptake (which is not organified) may still be present, but the nodule may lack radioiodine uptake (which is organified). Therefore, the nodule may be cold on radioiodine images but hot on pertechnetate images. Therefore, hot nodules on pertechnetate images are usually rescanned by using iodine-123 for further characterization. Technetium-99m pertechnetate study is not sensitive for nodules smaller than 5 mm, but its sensitivity increases to 100% in nodules larger than 2 cm.
Metastatic cancer is imaged well by using iodine-123 because one half of papillary and two thirds of follicular carcinomas are sufficiently iodine avid to allow their visualization. US is an alternative method that can be used to evaluate local tumor recurrence because, unlike iodine-123 scintigraphy, it does not require the cessation of thyroid hormone use for as long as 5-6 weeks.
Gallium-67 study
Scans performed by using this radionuclide have not demonstrated sufficient differentiation between the uptake in malignant nodules and the uptake in benign lesions to warrant its routine use. However, gallium-67 is useful when lymphoma of the thyroid is suspected.
Thallium-201 study
Thallium uptake is better visualized than gallium-67 uptake in the evaluation of cold nodules. Imaging at 3-5 hours after the administration of the agent demonstrates washout of activity from benign lesions, with intensely persisting activity in cancers.
Iodine fluorescence imaging
This technique is used only in a few centers in which dedicated equipment is available. An external beam of monoenergy gamma rays irradiates the thyroid, and the fluorescence of the intrinsic stores of stable iodine in the thyroid is studied. This technique provides a slightly different metabolic marker of thyroid function. The radiation dose used in this technique is low.
Degree of confidence
Radionuclide imaging is not reliable in excluding or confirming the presence of cancer. However, metastatic cancer is imaged well by using iodine-123, because one half of papillary and two thirds of follicular carcinomas are sufficiently iodine avid to allow their visualization. Scintigraphy provides a specific imaging tool for functional thyroid studies and for demonstrating aberrant thyroid tissue and nodules. Gallium-67 studies can be useful in assessing thyroid lymphoma, but their employment does not preclude the use of FNA.
False positives/negatives
The diagnosis of thyroid nodules is based on activity patterns of the radionuclide. Most malignant thyroid nodules are photon deficient, but so are thyroid cysts, some adenomas, and inflammatory nodules. Conversely, most benign thyroid nodules are hot, but 4% of thyroid cancers also can be hot.
-
Coned apical radiograph of the upper thorax shows curvilinear calcification in a thyroid adenoma, at the root of the neck, on the right side.
-
Posteroanterior chest radiograph shows a large retrosternal goiter (G) that displaces the trachea to the left (arrow).
-
Plain anteroposterior radiograph of the neck shows punctate calcification to the right of the cervical spine (straight arrow) and further multiple conglomerates of calcification at the root of the neck (curved arrow), also on the right.
-
Standard posteroanterior chest radiograph in the same patient as in the previous image shows widening of the superior mediastinum on the right in a lobulated fashion.
-
Plain radiograph of the upper abdomen in the same patient as in the previous 2 images shows multiple conglomerates of punctate calcification in the right hypochondrium encroaching on the left hypochondrium. The final diagnosis was a medullary carcinoma of the thyroid (calcified), lymph node metastases at the root of the neck (calcified), right superior mediastinal metastases, and gross hepatomegaly with multiple calcified hepatic metastases.
-
Posteroanterior chest radiograph shows a large, lytic, expanding metastasis in the anterior aspects of the right fifth and sixth ribs, secondary to an anaplastic thyroid carcinoma in an 85-year-old woman. Note displacement of the trachea to the left by a mass lesion at the root of the neck.
-
Anteroposterior chest radiograph of an 86-year-old woman who had been unwell for a few months and was losing weight. The radiograph shows a right superior mediastinal mass.
-
Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass (m) at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta.
-
Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass (m) at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta (same patient as in the previous image).
-
Ten-millimeter computed tomography section through the thorax shows a heterogeneous mass at the root of the neck, on the left, that displaces the trachea to the right. The mass appears to be growing in the caudal direction and is reaching the arch of the aorta (arrow) (same patient as in the previous 2 images).
-
Computed tomography scan shows a mass in the posterior mediastinum (P), which displaces the air-filled esophagus to the right (arrow) (same patient as in the previous 3 images).
-
Iodine-123 thyroid scan shows that a mass is a multinodular goiter (G). The posterior mediastinal mass is a hiatus hernia (H); the stomach (S) is shown. Further investigation revealed that thyrotoxicosis was the cause of the patient's symptoms.
-
Technetium-99m pertechnetate thyroid scan demonstrates normal findings in a thyroid gland.
-
Technetium-99m pertechnetate thyroid scan demonstrates an autonomous nodule with increased activity. Uptake in the remainder of the thyroid is suppressed.
-
Technetium-99m pertechnetate thyroid scan demonstrates intense activity in a large thyroid gland in a patient who was hypothyroid. The patient had Pendred syndrome. Note the pyramidal lobe (P).
-
Technetium-99m pertechnetate thyroid scan demonstrates a thyrotoxic goiter. Note the pyramidal lobe (arrow).
-
Technetium-99m pertechnetate thyroid scan demonstrates a multinodular goiter.
-
Technetium-99m pertechnetate thyroid scan demonstrates a cold nodule in the left lobe of the thyroid (C).
-
Technetium-99m pertechnetate thyroid scan shows a photon-deficient mass in the upper pole of the left lobe in a 53-year-old woman with a sudden onset of pain in the anterior aspect of the neck.
-
Sonogram demonstrates a multilocular benign cyst.
-
Repeat 3-month follow-up sonogram in a 53-year-old woman with a sudden onset of pain in the anterior part of the neck shows that the septa have resolved. However, debris and strands are noted at the bottom of the cyst (same patient as in the previous image).
-
Further 3-month follow-up sonogram shows a considerable reduction in the size of the cyst, with a tiny debris level at the base of the cyst, in a 53-year-old woman with a sudden onset of pain in the anterior part of the neck. The final diagnosis was hemorrhage in a benign cyst (same patient as in the previous 2 images).
-
Sonogram demonstrates a cystic colloid cyst with a comet tail artifact, in the thyroid.
-
Sonogram demonstrates a benign cystic lesion in the thyroid, with a surrounding halo and ragged walls.
-
Sonogram demonstrates a multilocular benign cyst in the thyroid.
-
Sonogram demonstrates thyroid cystic lesions in a 13-year-old female adolescent with cystic papillary thyroid carcinoma.
-
Technetium-99m pertechnetate thyroid scan shows a large cold nodule in the left lobe of the thyroid and a further, smaller cold nodule in right lobe.
-
Sonogram shows a 4-cm, hypoechoic, left-lobe thyroid mass.
-
Sonogram displaying a palpable, asymptomatic thyroid nodule (same patient as in the previous image) shows a solid mass in the thyroid, with a completely surrounding halo. The final diagnosis was a follicular carcinoma of the left lobe and a benign adenoma of the right lobe.
-
Image in a patient with a palpable, asymptomatic thyroid nodule shows a solid mass in the left lobe, with a complete surrounding halo (thyroid adenoma).
-
Power Doppler sonogram shows peripheral vascularity but no detectable flow in the tumor. The final diagnosis was benign thyroid adenoma (same patient as in the previous image).
-
A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously. On routine follow-up examination, a mass was felt in the thyroid. Coronal, T1-weighted magnetic resonance imaging scan shows a carcinoma recurrence (R) and lymph node (L) metastases.
-
A 56-year-old man underwent subtotal thyroidectomy for a familial medullary carcinoma 2 years previously (same patient as in the previous image). On routine follow-up examination, a mass was felt in the thyroid. Coronal, short-tau inversion recovery magnetic resonance imaging scan shows carcinoma recurrence (R) and lymph node (L) metastases.
-
Acute thyroiditis planar and power Doppler images. Courtesy of Shlomo Gobi, Sonographer.
-
Planar ultrasound images, color Doppler and resected papillary carcinoma of the thyroid. Courtesy Ravi Kadasne.
-
Planar and color Doppler images showing a cystic papillary thyroid carcinoma with a hypervascular intramural nodule. Courtesy Ravi Kadasne.
-
(1) Ultrasound planar images show a large solid but partially necrotic mass with microcalcification within. (2) Associated cervical lymphadenopathy. The patient presented with a mass on the right side of the neck. A biopsy revealed a papillary thyroid carcinoma.
-
CT images of the same patient as in previous images, showing a partially necrotic but enhancing mass in the left thyroid lobe and superior mediastinal lymphadenopathy.
-
Scanogram of the same patient as in previous images showing extensive miliary lung metastases and mediastinal lymphadenopathy.
-
Axial CT scans showing extensive miliary metastases.