Practice Essentials
Testicular trauma is uncommon because of its anatomic location and the mobility of testes within the scrotum. Most testicular trauma occurrences are related to sports injuries. Other causes include direct trauma, motor vehicle accidents, and straddle injuries. Patients present with an acute scrotum and history of trauma. The most common age range is 10 to 30 years. Rupture or fracture of the testis can result in the release of spermatic antigens, followed by production of anti-sperm antibodies, which can lead to infertility. Diagnosis is made in combination with clinical history and physical and ultrasound (US) findings. [1, 2, 3, 4, 5, 6, 7, 8, 9]
Blunt scrotal trauma may lead to rupture of the tunica albuginea of the testicle in 50% of cases presenting for evaluation. Ultrasound may confirm or imply testicular rupture, which should prompt exploration and attempt at repair. Penetrating injuries to the scrotum should undergo surgical exploration, as over 50% of cases will have testicular rupture. [10] Testicular rupture is a urologic emergency, and more than 80% of ruptured testes can be saved if surgery is performed within 72 hours. [11, 12, 13]
(See the images below.)
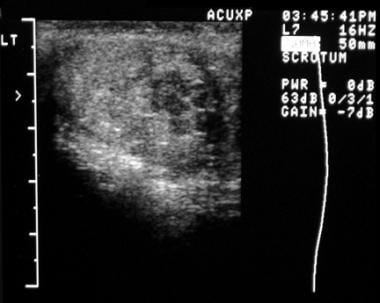 Longitudinal ultrasonogram of the left testis reveals multiple hypoechoic areas in the inferior pole, consistent with a contusion injury, secondary to gunshot wound.
Longitudinal ultrasonogram of the left testis reveals multiple hypoechoic areas in the inferior pole, consistent with a contusion injury, secondary to gunshot wound.
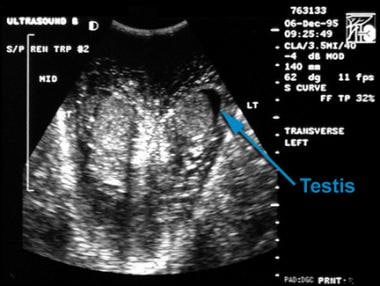 Transverse ultrasonogram of both testes demonstrates variable echo texture in the scrotal wall secondary to hemorrhage resulting from a motor vehicle accident.
Transverse ultrasonogram of both testes demonstrates variable echo texture in the scrotal wall secondary to hemorrhage resulting from a motor vehicle accident.
Preferred examination
According to all major guidelines, ultrasonography (US) is the imaging modality of choice for the diagnosis of testicular trauma. [10, 14, 15, 16] Doppler studies give an indication of the perfusion within the testicle and the integrity of the vascular hilum. Areas with impaired blood flow indicate either an intra‐testicular haematoma or nonviable testicular tissue. [14, 7]
If US fails to reveal contusion, hematoma, or testicular rupture, then surgical exploration should be performed. [5, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27] US is 80% specific for detecting tunica albuginea fracture.
The American Institute of Ultrasound in Medicine has published guidelines (in association with the American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound) on the evaluation of testicular and extratesticular structures. [15]
In a retrospective study of 298 boys with acute scrotum suggesting testicular torsion, color Doppler ultrasonography had a 96.8% sensitivity, 97.9% specificity, 92.1% positive predictive value, and 99.1% negative predictive value for testicular torsion. According to Waldert et al, approximately 20% of boys who present with acute scrotum have testicular torsion, and color Doppler is a reliable modality for making the diagnosis. [28]
Magnetic Resonance Imaging
According to Parenti et al, color Doppler ultrasound is irreplaceable as the initial approach for scrotal disease and trauma, but MRI is an ideal second-line modality. The authors followed 801 patients with scrotal disease or trauma who underwent color Doppler ultrasound, followed by MRI in 46 of the patients. [29] In the study, Doppler ultrasound revealed an inflammatory process in 277 patients, testicular trauma in 112, funicular torsion or torsion of the vestigial remnant in 44, and testicular neoplasm findings in 35. MRI identified 3 intraparenchymal hematomas, 1 intrascrotal cavernous body rupture, 1 testicular abscess with intrascrotal fistula, 2 testicular infarctions, and 15 neoplasms. MRI excluded focal abnormalities in 10 patients with testicular microlithiasis, in 3 with chronic orchitis, and in 4 with atrophic involution. MRI confirmed the finding of inguinal hernia in 3 cases. The authors concluded that MRI offers useful, occasionally decisive, information because of its ability to identify unexpected findings.
Kim et al explained that because of its high soft-tissue contrast and its multiplanar capability, MRI can be a useful alternative diagnostic modality for blunt scrotal trauma, especially when ultrasonography results in an inconclusive diagnosis. In 7 patients with blunt scrotal trauma, the diagnostic accuracy of MRI was 100%. Three cases with testicular rupture were diagnosed accurately, with interruption of the dark signal intensity line of the tunica albuginea being pathognomonic for the diagnosis of testicular rupture. In 2 cases in which there was an inconclusive diagnosis by ultrasonography, diagnoses of epididymal hematomas were correctly made by MRI. The remaining 2 cases showed concordant results with the surgical findings. [30]
Ultrasonography
Ultrasonography is the modality of choice for imaging of scrotal trauma. [12] US has a 100% sensitivity and an 80% specificity for testicular trauma. However, hemorrhage from an underlying tumor or incarcerated hernia may cause a false-positive diagnosis. [5, 17, 18, 19, 20, 21, 22, 23, 24]
Direct visualization of a testicular fracture line in US is rare, being observed only in approximately 17% of patients. [11] Demonstration of disruption of the tunica vasculosa is diagnostic of testicular rupture. Other US findings include scrotal wall thickening, hematocele, and testicular hematoma. US appearance of a hematocele varies depending on the length of time since trauma occurred.
Acute hematoceles are echogenic, and subacute and chronic hematoceles appear as fluid collections and may have fluid-fluid levels or low-level internal echoes. Hematocele is the most common finding.
In one study of 19 patients that evaluated US features of scrotal injuries caused by gunshot wounds, testicular rupture was detected sonographically in 6 patients. [24, 11] US in patients with surgically confirmed testicular rupture revealed heterogeneous echogenicity and loss of smooth oval contour.
(See the images below.)
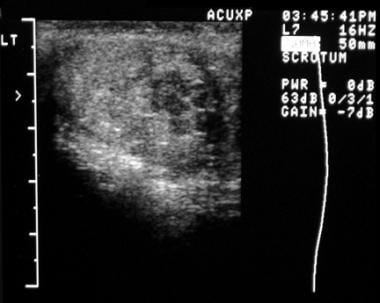 Longitudinal ultrasonogram of the left testis reveals multiple hypoechoic areas in the inferior pole, consistent with a contusion injury, secondary to gunshot wound.
Longitudinal ultrasonogram of the left testis reveals multiple hypoechoic areas in the inferior pole, consistent with a contusion injury, secondary to gunshot wound.
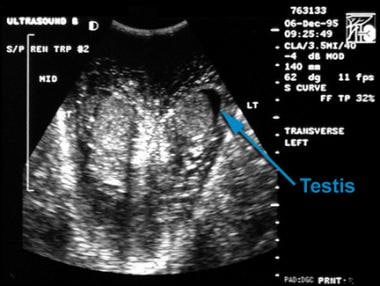 Transverse ultrasonogram of both testes demonstrates variable echo texture in the scrotal wall secondary to hemorrhage resulting from a motor vehicle accident.
Transverse ultrasonogram of both testes demonstrates variable echo texture in the scrotal wall secondary to hemorrhage resulting from a motor vehicle accident.
-
Longitudinal ultrasonogram of the left testis reveals multiple hypoechoic areas in the inferior pole, consistent with a contusion injury, secondary to gunshot wound.
-
Transverse ultrasonogram of both testes demonstrates variable echo texture in the scrotal wall secondary to hemorrhage resulting from a motor vehicle accident.




