Practice Essentials
Sternal fractures are often seen in association with deceleration injuries and/or direct blows to the chest, as in blunt chest trauma during motor vehicle accidents. [1] The introduction of seat-belt legislation has resulted in an increased frequency of these types of injuries. [2, 3, 4] Fractures are also a common complication of the repeated sternal compressions administered during cardiopulmonary resuscitation (CPR). The reported rates of CPR-related sternal fracture has ranged widely, from 16.1% to 72% of patients with nontraumatic cardiac arrest. [5, 6] In one series, the risk of fracture was found to be significantly higher in those receiving CPR for more than 10 minutes. [5]
Most sternal fractures occur in the midbody, and they are typically transverse. Manubrial fractures are the next most common. Stress fractures are occasionally seen in athletes such as wrestlers, but they can also occur in women with osteoporosis and kyphotic thoracic spines.
Patients should be carefully assessed for other potentially associated injuries such as rib fractures, flail chest, pneumothorax, hemothorax, pulmonary contusion, blunt cardiac injury (manifested by dysrhythmias or murmurs), pericardial tamponade, or vascular injury, as well as head, neck, abdominal, or extremity trauma. Sternal fracture–associated mortality can result from cardiac contusion, aortic rupture, pulmonary contusion, and thoracic spine compression fractures.
Sternal and rib fractures are common concomitant injuries. In a retrospective study by Choi et al, of 475,710 adults admitted with rib fractures, 24,594 (5%) also had sternal fractures. Additionally, patients with sternal fractures had a 70% higher risk of undergoing tracheostomy, 40% higher risk of undergoing intubation, 10-30% higher risk of respiratory failure, and 10-40% higher risk of mortality. [7]
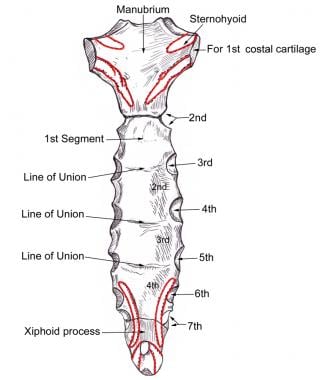
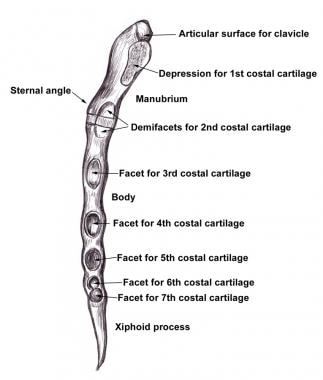
The sternum has 3 parts: the manubrium, the body (corpus), and the xiphoid process (tip) (see the images below).
The manubrium lies at the level of the third (T3) and fourth thoracic (T4) vertebrae. Along the superior margin of the manubrium is the suprasternal or jugular notch. Both the clavicle and the first rib articulate with the manubrium, and the sternal head of the sternocleidomastoid muscle inserts onto this portion of the sternum.
The joint between the manubrium and the body, the manubriosternal joint, forms the sternal angle, which is at the level of the second rib. In older people, this joint tends to be fused.
The xiphoid process is cartilaginous in younger people and ossified in older people.
Imaging modalities
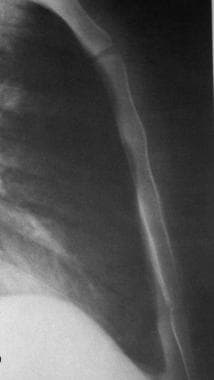
The routine radiologic study of the sternum consists of a lateral projection and frontal views, which are obtained with the patient prone and rotated slightly off the midline in each direction (see the images below). Normal anatomic variants, such as nonunited ossification centers, may sometimes cause a diagnostic dilemma. The lateral radiograph is usually the most valuable view for detecting sternal fractures and for determining the degree of displacement (see the images below). [8] Almost all patients with sternal fractures complain of localized sternal pain. Therefore, correlation with the clinical presentation is important. Nonunited ossification centers and failure of bony fusion of the sternomanubrial and sternoxiphoid articulations can simulate fractures; the angulation is variable at both of these sites. [3, 9, 10, 11]
Initially, computed tomography (CT) scan studies were less sensitive than plain radiographs. However, multidetector-row CT (MDCT) scanning units now allow for multiplanar and 3-dimensional (3-D) reconstruction, which greatly improve accuracy. CT scanning provides superior sensitivity and specificity but at greater cost and with increased radiation exposure. CT scanning is particularly useful to assess patients with sternal fractures for associated injuries such as pulmonary contusion, pneumothorax, or retrosternal hematoma. [3, 12, 10, 11, 13, 14]
In a study of 292 patients with sternal fracture by Terry et al, 94% of fractures were visible only on chest CT, and cardiac contusion was identified in 7 of the patients. [15]
Ultrasonography has been proven to be as accurate as radiography in diagnosing sternal fractures, but conventional radiography remains the standard means of documenting a sternal fracture. [16, 17, 18, 19] In children, subtle sternal fractures may be missed with CT and radiography, and ionizing radiation is a concern. Some studies have shown that ultrasound may be of particular benefit in diagnosing sternal fractures in these patients. However, ultrasonography is operator-dependent and has a smaller scanning area than imaging modalities such as radiography, CT, or MRI. [20, 21, 22, 23]
Nuclear bone scanning may be needed if the initial radiographic findings are not definitive. Total-body bone scans are sensitive for acute sternal trauma. However, the anatomic detail is limited, and correlation with the results of radiography or CT scanning is often necessary.
(See the images below.)
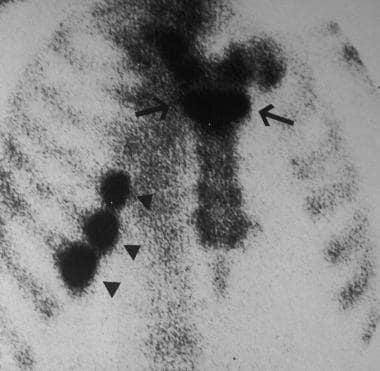 Nuclear bone scan of fractures of the sternum (arrow) and of the ribs on the right side (arrowheads).
Nuclear bone scan of fractures of the sternum (arrow) and of the ribs on the right side (arrowheads).
 Upright frontal radiograph in the same patient as in the previous image shows mild widening of the superior mediastinum after blunt trauma to the chest.
Upright frontal radiograph in the same patient as in the previous image shows mild widening of the superior mediastinum after blunt trauma to the chest.
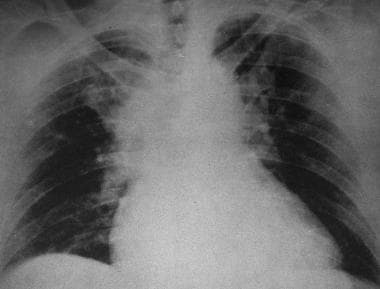 Supine frontal radiograph after significant blunt trauma to the anterior chest wall shows marked mediastinal widening. (Also see next image.)
Supine frontal radiograph after significant blunt trauma to the anterior chest wall shows marked mediastinal widening. (Also see next image.)
 Lateral radiograph shows a complete displaced fracture of the sternum (arrow) (same patient as in the previous image above).
Lateral radiograph shows a complete displaced fracture of the sternum (arrow) (same patient as in the previous image above).
According to the American College of Radiology (ACR), clinical judgement should be used to determine which patients should receive whole-body CT following a blunt trauma with suspected chest injury. Indications for WBCT include the following [24] :
-
Motor vehicle accidents: high-velocity (>35 mph), rollover, or ejection from the vehicle
-
Motorcycle accident
-
Bicycle accident
-
Pedestrian hit by a motor vehicle
-
Fall from greater than 15 ft
Trauma to the aorta and cardiac and/or pulmonary contusions are part of the differential diagnosis.
Ultrasonography
-
Lateral radiograph of the normal sternum.
-
Frontal radiograph of the normal sternum.
-
(Click Image to enlarge.) Posterior surface of the sternum.
-
(Click Image to enlarge.) Lateral border of the sternum.
-
Nuclear bone scan of fractures of the sternum (arrow) and of the ribs on the right side (arrowheads).
-
Lateral radiograph demonstrates complete dislocation at the sternal angle. (Also see next image.)
-
Upright frontal radiograph in the same patient as in the previous image shows mild widening of the superior mediastinum after blunt trauma to the chest.
-
Supine frontal radiograph after significant blunt trauma to the anterior chest wall shows marked mediastinal widening. (Also see next image.)
-
Lateral radiograph shows a complete displaced fracture of the sternum (arrow) (same patient as in the previous image above).