Practice Essentials
The term atelectasis, which is defined as diminished lung volume, is derived from the Greek words ateles and ektasis, which mean incomplete expansion (see the image below). Atelectasis may affect all or part of a lung, and it is one of the most common radiographic abnormalities. Recognizing atelectasis on a chest radiograph is important because a sinister underlying pathology may be present. Lobar atelectasis occurs in a variety of medical conditions, such as a critical illness, a postoperative complication, a trauma, or lung cancer. The main etiology of lobar atelectasis is bronchial obstruction by mucus plugs from buildup of copious purulent secretions due to defective clearance mechanisms. Although lobar atelectasis is considered a less severe postoperative complication, in a multicenter study of noncardiothoracic surgery patients, atelectasis was associated with increased early postoperative mortality, ICU admission, and length of hospital stay. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]
Atelectasis can be categorized as obstructive or nonobstructive. Several types have been described, such as complete, adhesive, replacement, passive, rounded, and cicatrization. Atelectasis is also described by location, such as right or left upper, middle, or lower. Each has a unique radiographic pattern. [11, 12, 13, 14, 9, 10, 15]
(See the image below.)
 Gross anatomic specimen showing airless lungs, or atelectasis. Atelectasis refers to either incomplete expansion of the lungs or the collapse of previously inflated lungs, which produces areas of relatively airless pulmonary parenchyma.
Gross anatomic specimen showing airless lungs, or atelectasis. Atelectasis refers to either incomplete expansion of the lungs or the collapse of previously inflated lungs, which produces areas of relatively airless pulmonary parenchyma.
Obstructive atelectasis
An obstruction between the alveoli and trachea causes reabsorption of alveolar gas, leading to an obstructive atelectasis. The obstruction can occur at the level of the larger or smaller bronchus, and it may be secondary to a foreign body, benign or malignant tumor, mucus plug, and blood clot, as well as bronchial transection, fibrotic stenosis from granulomas or inflammation, polychondritis, post brachytherapy or radiotherapy stenosis, and other obstructive lesions. [16]
The development of atelectasis depends on several factors, including the extent of collateral ventilation and the composition of inspired gas. Obstruction of a larger bronchus is likely to produce lobar atelectasis, whereas the obstruction of a smaller bronchus causes segmental atelectasis. The pattern of atelectasis often depends on collateral ventilation, which is provided by the pores of Kohn and the canals of Lambert.
Right middle lobe (RML) syndrome, a form of chronic atelectasis, usually results from bronchial compression and obstruction by surrounding lymph nodes or bronchial scarring. Partial bronchial obstruction and recurrent infection may also lead to chronic atelectasis and acute or chronic pneumonitis.
Nonobstructive atelectasis
Loss of contact between the parietal and visceral pleurae causes nonobstructive atelectasis. The etiologies may be lung compression, the loss of surfactant, and scarring or infiltrative disease of the lung. Several types of nonobstructive atelectasis are known to occur from a variety of causes.
A pleural effusion or a pneumothorax eliminates contact between the parietal and visceral pleurae, and relaxation or passive atelectasis results. The uniform elasticity of a normal lung preserves the shape, even after atelectasis is present. The middle and lower lobes collapse more than the upper lobes in the presence of a pleural effusion, whereas the upper lobes are more affected by a pneumothorax.
Compression atelectasis occurs when any space-occupying lesion of the thorax compresses the lung and forces air out of the alveoli. The mechanism is similar to relaxation atelectasis.
Adhesive atelectasis results from surfactant deficiency. Surfactant lowers the surface tension of the alveoli and therefore plays an important role in preventing the alveoli from collapsing. Decreased production or inactivation of surfactant, as observed in acute respiratory distress syndrome (ARDS) and similar disorders, leads to alveolar instability and atelectasis.
Cicatrization atelectasis results as a sequela of severe parenchymal scarring and is usually caused by granulomatous disease or necrotizing pneumonia. The lobar collapse from cicatrization may be either obstructive if the bronchi are involved or nonobstructive because of the fibrotic process in the lung parenchyma. Replacement atelectasis occurs when the alveoli of an entire lobe are filled by tumor (eg, bronchioalveolar cell carcinoma), resulting in a loss of volume.
Rounded atelectasis, also called folded-lung syndrome or Blesovsky syndrome, occurs as the lung collapses and folds secondary to fibrous bands and adhesions to the visceral pleura. [17] The incidence is high in asbestos workers (65-70% of cases). Patients are typically asymptomatic, and the mean age at presentation is 60 years. Rounded atelectasis is a benign disorder.
Preferred examination
Chest radiographs are generally sufficient to diagnose lobar atelectasis and to identify the collapsed lobe. [18] Chest radiographs are also useful in diagnosing platelike atelectasis, postoperative atelectasis, [19] and rounded atelectasis, as well as for following the course of the atelectasis. For example, chest radiographs can be used to determine whether an intervention, such as chest physiotherapy, has resulted in improvement. [20, 11]
A concomitant pleural effusion, pleural mass, or large lung mass may limit the usefulness of chest radiography in the diagnosis of atelectasis. In such cases, computed tomography (CT) scanning is a useful next imaging study. CT scanning should be used to assess obstructive atelectasis; this modality is also helpful in evaluating the mediastinum, chest wall, hilum, pleura, and adjacent lung. [12, 13, 21, 22, 23, 24] When a basal opacity, an opacity of the hemithorax, and other signs of atelectasis are not obvious on radiography, determining whether the opacity is a pleural effusion or a lobar collapse may be difficult. In those situations, a CT scan can be of immense help. Intravenous contrast enhancement is often required for appropriate imaging and for differentiating between various causes of atelectasis.
The limitation of CT scanning may be in differentiating between obstructive and nonobstructive causes of atelectasis. Furthermore, a CT scan may not be useful in determining whether the obstructing lesion is a tumor, mucus plug, nonopaque foreign body, or blood clot.
Magnetic resonance imaging (MRI) has no particular value in the diagnosis of lobar atelectasis, except for distinguishing obstructive from nonobstructive atelectasis. [25]
Radiography
Chest radiography has the highest sensitivity when direct signs of atelectasis can be detected. More specifically, the identification of a displaced fissure is of significant advantage in diagnosing lobar collapse. The presence of several indirect signs further corroborates the direct signs in the diagnosis of atelectasis. Modest loss of volume may occur secondary to lobar consolidation; this may lead to the erroneous diagnosis of lobar collapse.
Chest radiographs and CT scans show direct and indirect signs of lobar collapse. Direct signs include displacement of fissures and opacification of the collapsed lobe. Indirect signs include the following:
-
Displacement of the hilum
-
Mediastinal shift toward the side of collapse
-
Loss of volume in the ipsilateral hemithorax
-
Elevation of the ipsilateral diaphragm
-
Crowding of the ribs
-
Compensatory hyperlucency of the remaining lobes
-
Silhouetting of the diaphragm or heart border
A loculated pleural effusion or pleural effusion with passive collapse may be mistakenly identified as a collapse secondary to an endobronchial lesion. False-negative results may occur if the collapse does not involve the whole lobe; this situation may be secondary to an incompletely obstructive bronchial lesion or partial ventilation of the lobe.
Platelike atelectasis or postoperative atelectasis may often be missed on chest radiographs because it may be obscured by other thoracic structures. A false-negative diagnosis may also occur if the patient cannot take a full breath or if the anteroposterior or lateral chest radiograph is not available.
Complete atelectasis
Complete atelectasis of an entire lung is characterized by a complete collapse of a lung, which leads to opacification of the entire hemithorax and an ipsilateral shift of the mediastinum. The mediastinal shift separates atelectasis from a massive pleural effusion. (See the images below.)
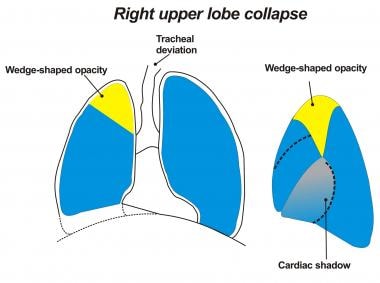
Right upper lobe collapse
The collapsed right upper lobe (RUL) shifts medially and superiorly, resulting in elevation of the right hilum and the minor fissure. The RUL may also collapse laterally, producing a pleural-based opacity that may look like a loculated pleural effusion.
The minor fissure in an RUL collapse is usually convex at its superior aspect, but it may appear concave because of an underlying mass lesion. This is called the Golden sign of S (also known as the Golden S sign and the S sign of Golden).
Tenting of the diaphragmatic pleura, called the juxtaphrenic peak sign, is another helpful sign of RUL atelectasis. [26]
(See the images below.)
 Right upper lobe collapse. This chest radiograph shows volume loss in the upper lobe, upward shifting of the horizontal fissure, and elevation of the right side of the diaphragm.
Right upper lobe collapse. This chest radiograph shows volume loss in the upper lobe, upward shifting of the horizontal fissure, and elevation of the right side of the diaphragm.
 Lateral chest radiograph demonstrating a right upper lobe collapsing anteriorly and superiorly. The opacity is seen in the anterior and superior locations.
Lateral chest radiograph demonstrating a right upper lobe collapsing anteriorly and superiorly. The opacity is seen in the anterior and superior locations.
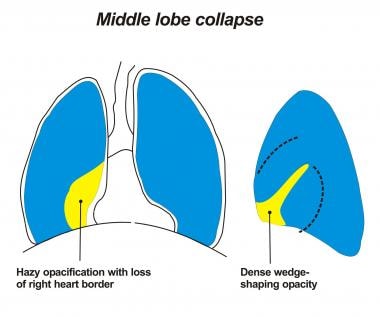
Right middle lobe collapse
RML collapse obscures the right heart border on a posteroanterior (PA) image. The lateral view shows a triangular opacity overlying the heart because the major fissure shifts upward and the minor fissure shifts downward. With worsening collapse, the opacity diminishes in size, and it may be barely perceptible.
(See the images below.)
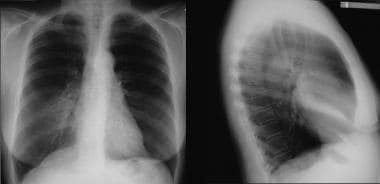 Posteroanterior (PA) (left) and lateral chest (right) radiographs. A right middle lobe collapse obliterates the right heart border on the PA image and projects as a wedge-shaped opacity on the lateral view.
Posteroanterior (PA) (left) and lateral chest (right) radiographs. A right middle lobe collapse obliterates the right heart border on the PA image and projects as a wedge-shaped opacity on the lateral view.
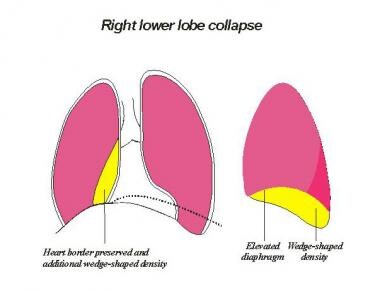
Right lower lobe collapse
The collapsed right lower lobe (RLL) shifts posteriorly and inferiorly, resulting in a triangular opacity that obscures the RLL pulmonary artery. The major fissure, normally not visible on a PA radiograph, is evident with an RLL collapse. The superior mediastinal structure shifts to the right, causing a superior triangle sign. Laterally, the collapsed RLL obliterates the posterior one third of the right hemidiaphragm and projects as an opacity over the normally lucent area.
(See the images below.)
 Lateral chest radiograph demonstrating a right lower lobe collapse that results in volume loss, obliteration of the right side of the diaphragm, and a posterior opacity.
Lateral chest radiograph demonstrating a right lower lobe collapse that results in volume loss, obliteration of the right side of the diaphragm, and a posterior opacity.
Concomitant RML and RLL atelectasis may appear as an elevated right hemidiaphragm or a subpulmonic effusion. An attempt to identify the fissures usually leads to the accurate diagnosis.
(See the image below.)
 Chest radiograph demonstrating a right lower lobe collapse and a right middle lobe collapse. The left lung is hyperexpanded.
Chest radiograph demonstrating a right lower lobe collapse and a right middle lobe collapse. The left lung is hyperexpanded.
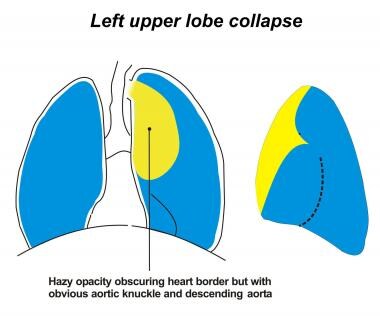
Left upper lobe collapse
An atelectatic left upper lobe (LUL) shifts anteriorly and superiorly. In one half of the cases, a hyperexpanded superior segment of the left lower lobe (LLL) is positioned between the atelectatic upper lobe and the aortic arch. This gives the appearance of a crescent of the aerated lung, called the luftsichel sign.
On PA views, an atelectatic LUL produces a faint opacity in the left upper hemithorax, obliterating the left heart border. On lateral views, the major fissure is displaced anteriorly behind the sternum.
(See the images below.)
 Left upper lobe collapse. This radiograph shows an opacity that is contiguous with the aortic knob, a smaller left hemithorax, and a mediastinal shift. The luftsichel sign involves hyperextension of the superior segment of the left lower lobe, which then occupies the left apex.
Left upper lobe collapse. This radiograph shows an opacity that is contiguous with the aortic knob, a smaller left hemithorax, and a mediastinal shift. The luftsichel sign involves hyperextension of the superior segment of the left lower lobe, which then occupies the left apex.
 Chest radiograph demonstrating a left upper lobe collapse, resulting in a veil-like opacity that extends upward and outward from the hilum. Additional signs of loss of volume in the left hemithorax and crowding of the ribs are also evident on this radiograph.
Chest radiograph demonstrating a left upper lobe collapse, resulting in a veil-like opacity that extends upward and outward from the hilum. Additional signs of loss of volume in the left hemithorax and crowding of the ribs are also evident on this radiograph.
Left lower lobe collapse
On frontal views, an increased retrocardiac opacity obliterates the LLL pulmonary artery and the left hemidiaphragm. The hilar structures shift downward, and the rotation of the heart produces flattening of the cardiac waist, which is known as the flat-waist sign. The superior mediastinum may shift and obliterate the aortic arch; this is the top-of-the-aortic-knob sign.
On the lateral radiographs, an opacity silhouettes the posterior third of the left diaphragm, and an opacity is projected over the normally lucent area. (See the images below.)
 Left lower lobe collapse. This chest radiograph shows volume loss on the left side, an elevated and silhouetted left diaphragm, and an opacity behind the heart (ie, sail sign).
Left lower lobe collapse. This chest radiograph shows volume loss on the left side, an elevated and silhouetted left diaphragm, and an opacity behind the heart (ie, sail sign).
Rounded atelectasis
In cases of rounded atelectasis, segmental or subsegmental atelectasis occurs secondary to visceral pleural thickening and entrapment of the lung tissue.
Rounded atelectasis manifests as a subpleural mass, and bronchovascular structures radiate out of the mass toward the hilum. An associated parietal pleural plaque may be present. The swirl appearance of the bronchovascular shadows is called the comet-tail sign and establishes the diagnosis. [27]
Computed Tomography
The common etiologies of lobar collapse include central endobronchial tumor, long-standing infection, pleural disease, and previous irradiation. CT scanning may play an important role in differentiating obstructive endobronchial lesions from other forms of collapse. By identifying the exact location of an endobronchial lesion and the presence of peribronchial spread, CT scans may be helpful in planning bronchoscopy and transbronchial biopsy. Evaluation of the mediastinum, pleura, chest wall, and adrenal glands plays a role in the staging process. [17, 21, 22, 23, 24, 28, 29]
In evaluating patients with radiographically atypical forms of collapse, CT scans further help in accurately delineating the collapse and in identifying any additional pathology. [30, 31] CT scans are particularly helpful in patients who have a pleural effusion associated with atelectasis, and these images have a significant advantage over plain radiographs in the assessment of pleural malignancy. Finally, CT scans are especially useful in evaluating patients with cicatrization atelectasis. These patients have underlying bronchiectasis and present with atypical plain radiographic findings.
Determining the cause of an endobronchial obstruction on the basis of CT scans alone may be difficult. CT scans may not be useful in distinguishing between an endobronchial malignancy, benign tumor, mucus plug, blood clot, and another nonopaque foreign body. Significant lung collapse associated with pleural effusion may not have the characteristic findings of lobar collapse; therefore, discerning whether an endobronchial lesion is present may be difficult. CT scanning is also limited in differentiating a consolidation secondary to an infectious cause from a replacement collapse in which a tumor has infiltrated the entire lobe. CT scans do not obviate bronchoscopy, which is a mandatory procedure to accurately localize an endobronchial lesion and to characterize its nature. Bronchoscopy may also serve a therapeutic role.
The primary changes of lobar collapse seen on CT scan are as follows:
-
Irregular narrowing or occlusion of a bronchus, indicating an obstructive lobar collapse
-
Lobe becoming pie shaped rather than hemispherical on cross-section.
-
Possible projection of the lobe as a V-shaped structure where the apex is situated at the origin of the affected bronchus
-
Overall increased opacity of the lobe
-
Possible bulge in the adjacent fissure (ie, the Golden sign of S), caused by a mass
-
Pattern of collapse affected by previous pleural adhesions and fluid or air in the pleural space
-
Possible infiltration of the entire lobe by the tumor, giving it a lobular, rather than wedge-shaped, appearance
Right upper lobe collapse
The RUL is bordered medially by the mediastinum, superiorly by the chest wall, inferiorly by the minor fissure, and posteroinferiorly by the superior portion of the oblique fissure.
On CT scanning, RUL collapse appears as a right paratracheal opacity, and the minor fissure appears concave laterally. The RUL collapses against the mediastinum, and this is identified as a wedge of uniform attenuation extending along the mediastinum to the anterior chest wall. There is concomitant hyperinflation of the middle and lower lobes. A bulge in the contour of the collapsed RUL occurs secondary to an endobronchial tumor and gives an S-shaped configuration. Endobronchial obstruction is readily identifiable on the CT scan.
(See the image below.)
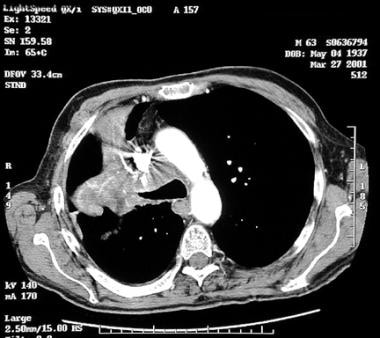 This computed tomography scan shows a right upper lobe collapse secondary to a right hilar mass. On bronchoscopy, an endobronchial lesion that occluded the right upper lobe bronchus was seen.
This computed tomography scan shows a right upper lobe collapse secondary to a right hilar mass. On bronchoscopy, an endobronchial lesion that occluded the right upper lobe bronchus was seen.
Right middle lobe collapse
The RML is bounded medially by the right heart border; anteriorly and laterally by the chest wall; posteriorly by the major fissure; and superiorly by the minor fissure.
As the RML collapses, the minor fissure shifts downward and the oblique fissure is displaced forward. With a progressive loss of volume, the middle lobe collapses medially against the right heart border. The collapsed middle lobe is a wedge-shaped opacity that extends laterally from the hilum toward the lateral chest wall. It is bounded posteriorly by the RLL and anteriorly by the hyperinflated RUL.
On CT scans, a triangular opacity along the right heart border, with the apex pointing laterally, is a characteristic finding. This appearance resembles a tilted ice-cream cone.
Right lower lobe collapse
The RLL is bordered inferiorly by the hemidiaphragm, posteriorly and laterally by the chest wall, medially by the heart and mediastinum, and anteriorly by the major fissure.
The RLL generally collapses in a posteromedial direction against the posterior mediastinum and spine. An endobronchial lesion may result in a convex lateral contour of the collapsed RLL. The major fissure is displaced posteromedially.
Left upper lobe collapse
The LUL is bounded medially by the mediastinum, inferiorly by the left heart border, superiorly and laterally by the chest wall, and posteriorly by the major fissure.
CT scanning shows the inferior location of the collapsed lobe and the shift of the RUL across the midline. LUL collapse occurs anterosuperiorly. As opposed to the RUL, the collapsed LUL maintains more contact with the anterior and lateral chest wall. Hyperaeration of the superior segment of the LLL may cause displacement and superior movement; these changes may account for periaortic lucency or the luftsichel sign on PA images. The LUL maintains its contact with the mediastinum and remains attached to the left hilum by a wedge of collapsed tissue. The anterosuperior direction of the collapse projects a wedge-shaped triangular opacity, with the apex pointing posteriorly. Endobronchial obstruction is easily identified on CT scans.
Left lower lobe collapse
The LLL is bordered inferiorly by the hemidiaphragm, posteriorly and laterally by the chest wall, medially by the heart and mediastinum, and anteriorly by the major fissure. The LLL collapses medially toward the mediastinum and maintains contact with the hemidiaphragms. The major fissure moves posteriorly. The LLL has an opacity situated against the posterior mediastinum. CT scanning shows the atelectatic LLL in the inferior posterior location. (See the image below.)
Passive atelectasis
Passive atelectasis is likely the most common form of atelectasis. It occurs secondary to the presence of air or fluid in the pleural space. The CT scan easily depicts pleural effusion and the underlying collapsed lung. Differentiation may be made easier with the use of contrast medium. The pattern of collapse secondary to an endobronchial lesion is distorted in the presence of pleural fluid. CT scanning may be of some help in distinguishing benign causes from malignant causes of pleural effusion. An irregular or nodular pleural surface may indicate an underlying malignancy.
Cicatrization atelectasis
Scarring or fibrosis from an inflammatory disease may lead to cicatrization collapse, the most common example being previous tuberculosis.
In cicatrization atelectasis, an endobronchial lesion is not seen and the bronchial tree in the collapsed lobe is hidden. Marked volume loss is present, and bronchiectatic changes frequently occur in the involved lobe.
Chronic middle-lobe syndrome results in a patent bronchus. Significant bronchiectasis and scarring may be observed in the collapsed lobe.
Adhesive atelectasis
Adhesive atelectasis occurs secondary to the loss of surfactant. A common cause is lung collapse due to radiation pneumonitis. The CT scan appearance is a sharp line demarcating the normal pulmonary parenchyma from the irradiated lung, which is generally paramediastinal.
Replacement atelectasis
Replacement atelectasis is a form of volume loss in which the pulmonary parenchyma is replaced by tumor infiltration. In this situation, the CT scan shows uniform attenuation throughout the involved lobe. This finding generally mimics consolidation. The tumor may grow into the edges and structures, such as the chest wall or mediastinum.
Rounded atelectasis
Rounded atelectasis is a form of chronic atelectasis that may appear as a mass lesion on chest radiographs. Although this form is most commonly associated with asbestos exposure, other benign conditions may also be present. These conditions include tuberculosis, uremic pleuritis, pulmonary infarction, and other causes of pleuritis. Because of adhesions between the visceral pleura and parietal pleura, the atelectatic lung becomes trapped and folds onto itself. [14, 28]
In cases of rounded atelectasis, the CT scan results are diagnostic and definitive; therefore, further investigations to exclude lung cancer are not required. The CT scan findings are a peripheral oval or wedge-shaped attenuating area with smooth lateral edges and a medial irregular or ill-defined border that points to the hilum. Distortion and displacement of the blood vessels and bronchi appear in a characteristic curvilinear configuration that leads to the rounded atelectasis (ie, comet-tail sign). In most cases, bronchograms are seen on the CT scan, and calcification is also common. (See the image below.) Crowded and converging bronchovascular bundles enter the mass from all sides, termed the crow's-feet sign. [15]
 Computed tomography scan demonstrating rounded atelectasis in a patient exposed to asbestos. This image shows a peripheral pleural-based opacity with crowding of the bronchovascular structures in the comet-tail sign.
Computed tomography scan demonstrating rounded atelectasis in a patient exposed to asbestos. This image shows a peripheral pleural-based opacity with crowding of the bronchovascular structures in the comet-tail sign.
Magnetic Resonance Imaging
The role of MRI in differentiating a central obstructing tumor from a peripheral collapsed lung has been evaluated. T2-weighted sequences are useful in identifying an endobronchial lesion. [25, 32] Because lipid-laden macrophages accumulate in the subacute phase of lobar collapse, progressive lymphocytic infiltration and collagen deposition occur within the pulmonary interstitium. In these situations in which the ratio of lung to fat in the collapsed lung is greater than 1, T2-weighted MRIs are most useful in differentiating a tumor from lung collapse.
MRI may have a role in the evaluation of adhesive atelectasis. T2-weighted sequences may help in differentiating fibrosis secondary to an endobronchial obstruction from radiation-induced pneumonitis. Furthermore, MRI may have a role in diagnosing rounded atelectasis, because MRIs may more accurately depict curvilinear vessels in the folded lung. [33]
MRI is an excellent imaging modality in situations in which intravenous contrast material cannot be administered. MRIs may delineate the extent and the location of a tumor; this modality may also have a role when CT scans are not helpful in differentiating between a tumor and a collapsed lung.
Ultrasonography
Ultrasonography has a limited role in the evaluation of atelectasis. The only potential role for this modality is in differentiating a basal lung collapse from a loculated pleural effusion. However, there are data to support the use of bedside ultrasonography in cases in which the clinical history and findings, as well as the radiologic studies of critically ill patients, are inconclusive. [34, 35, 36]
In addition, studies evaluating the usefulness of routine ultrasonography in neonatal lung disease have found US to be reliable and accurate for the diagnosis of pulmonary atelectasis. The advantages of ultrasound include avoiding transport, easy to control body position, no radiation exposure, and availability at bedside. [37, 38]
CT scanning is preferred tover ultrasonography because CT scanning is more accurate, delineates the surrounding structures better, and is more useful in identifying the cause of atelectasis.
-
Gross anatomic specimen showing airless lungs, or atelectasis. Atelectasis refers to either incomplete expansion of the lungs or the collapse of previously inflated lungs, which produces areas of relatively airless pulmonary parenchyma.
-
Image depicting a right upper lobe collapsing posteriorly and inferiorly.
-
Image depicting a right middle lobe collapsing medially.
-
Image depicting a right lower lobe collapsing anteriorly and superiorly.
-
Image depicting a left upper lobe collapsing superiorly and anteriorly.
-
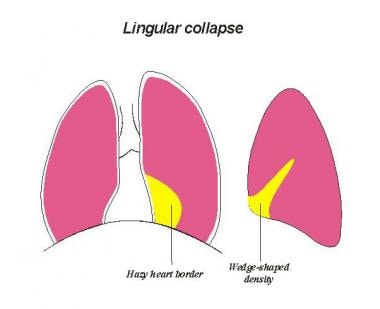
Image depicting the lingula collapsing medially.
-
Image depicting a left lower lobe collapsing posteriorly and inferiorly.
-
Chest radiograph demonstrating complete atelectasis of the left lung.
-
Left upper lobe collapse. This radiograph shows an opacity that is contiguous with the aortic knob, a smaller left hemithorax, and a mediastinal shift. The luftsichel sign involves hyperextension of the superior segment of the left lower lobe, which then occupies the left apex.
-
Chest radiograph demonstrating a left upper lobe collapse, resulting in a veil-like opacity that extends upward and outward from the hilum. Additional signs of loss of volume in the left hemithorax and crowding of the ribs are also evident on this radiograph.
-
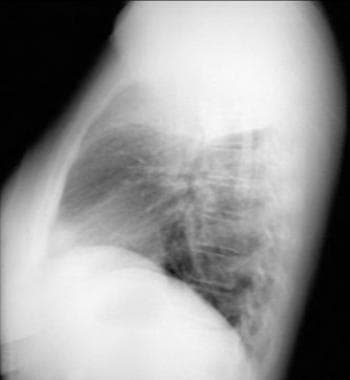
Lateral chest radiograph demonstrating a left upper lobe collapsing anteriorly.
-
Computed tomography scan shows a left lower lobe collapse with a small pleural effusion.
-
Chest radiograph depicting complete right lung atelectasis.
-
Left lower lobe collapse. This chest radiograph shows volume loss on the left side, an elevated and silhouetted left diaphragm, and an opacity behind the heart (ie, sail sign).
-
Right upper lobe collapse. This chest radiograph shows volume loss in the upper lobe, upward shifting of the horizontal fissure, and elevation of the right side of the diaphragm.
-
Lateral chest radiograph depicting left a lower lobe collapse. The opacity is in a posteroinferior location.
-
Lateral chest radiograph demonstrating a right upper lobe collapsing anteriorly and superiorly. The opacity is seen in the anterior and superior locations.
-
This computed tomography scan shows a right upper lobe collapse secondary to a right hilar mass. On bronchoscopy, an endobronchial lesion that occluded the right upper lobe bronchus was seen.
-
Chest radiograph demonstrating a right lower lobe collapse and a right middle lobe collapse. The left lung is hyperexpanded.
-
Posteroanterior (PA) (left) and lateral chest (right) radiographs. A right middle lobe collapse obliterates the right heart border on the PA image and projects as a wedge-shaped opacity on the lateral view.
-
Lateral chest radiograph demonstrating a right lower lobe collapse that results in volume loss, obliteration of the right side of the diaphragm, and a posterior opacity.
-
Computed tomography scan demonstrating rounded atelectasis in a patient exposed to asbestos. This image shows a peripheral pleural-based opacity with crowding of the bronchovascular structures in the comet-tail sign.
-
Posteroanterior (PA) (left) and lateral chest (right) radiographs from a patient with collapse of the right middle lobe. The PA view shows the right middle lobe collapse obscuring the right heart border. The lateral view shows a triangular opacity that overlies the heart because the major fissure shifts upward and the minor fissure shifts downward. With worsening collapse, the opacity diminishes in size, and it may be barely perceptible.
-
Chest radiograph showing collapse of the left lower lobe toward the posterior and inferior aspect of the thoracic cavity. The atelectatic left lower lobe is present as a sail sign behind the cardiac shadow.