Practice Essentials
Radiography is the mainstay in idiopathic scoliosis imaging to both confirm the diagnosis and rule out any underlying conditions. Scoliosis is the presence of one or more lateral rotatory curves of the spine in the coronal plane. Although defined as a side-to-side deformity, it is a 3-dimensional (3D) rotational deformity. Many causes of scoliosis are known; however, 80% of cases are idiopathic. Idiopathic scoliosis is a diagnosis of exclusion.
(See the images below.)
Most cases of scoliosis are managed conservatively, but surgery is required in select cases to arrest further progression of the deformity, to correct the curve, and to manage severe pain. Imaging plays a crucial role in confirming the diagnosis, determining the cause, grading the severity of the curve, assessing maturity, identifying patients who need surgery, and assessing postoperative complications.
American College of Radiology guidelines and recommendations
The ACR guidelines include the following [1] :
-
Indications for radiography include alterations in normal spinal alignment on physical examination or detected on other imiaging studies, evaluation of spinal curvature progression, follow-up of treatment, and evaluation of individuals at risk for scoliosis.
-
For a scoliosis survey, the preferred method is a posteroanterior radiograph with the patient in the upright position.
-
For patients who are being assessed or are being clinically treated for scoliosis, other images include right and left lateral bending images, hyperextension and hyperflexion upright views to determine the flexibility of kyphosis and lordosis, respectively, and a posteroanterior image of the wrist and the hand for bone age.
-
Radiographic analysis should identify the presence and number of curves, curve pattern, location, curve length and measurement, and vertebral rotation.
-
Additional measurements may be obtained in special cases, such as the rib-vertebral angle in infantile idiopathic scoliosis.
-
Skeletal maturity determination is important because mild to moderate scoliotic curves do not progress after cessation of growth.
Imaging modalities
Clinical examination should include neurologic examination to assess the deformity. A scoliometer is placed over the spinous process at the apex to measure the angle of trunk rotation (ATR). The measurement is significant if it is more than 5°. A scoliometer measurement of 10° or greater requires radiologic evaluation for Cobb angle measurement. [2, 3]
Radiography is the mainstay in assessment of scoliosis (see the images below). It is used to confirm the clinical diagnosis of scoliosis, to exclude underlying causes (eg, segmentation abnormalities), to assess the curves and their severity, to monitor progression, to assess skeletal maturity, and to determine a patient's suitability for surgery. This study is also useful in diagnosing postoperative complications and in follow-up.
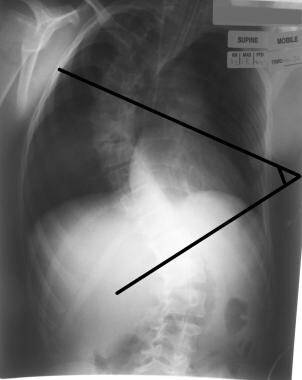
 Plain radiograph illustrates the common terms used in describing the scoliotic curve. The upper and lower end vertebrae and apical vertebra are illustrated. The vertebrae and disk spaces are smaller on the concave side and larger on the convex side. The spinous process is rotated towards the concave side. The ribs are crowded on the concave side.
Plain radiograph illustrates the common terms used in describing the scoliotic curve. The upper and lower end vertebrae and apical vertebra are illustrated. The vertebrae and disk spaces are smaller on the concave side and larger on the convex side. The spinous process is rotated towards the concave side. The ribs are crowded on the concave side.
 Radiograph shows various grades of vertebral rotation in the spine. The pedicles are normal in the bottom vertebra, but they are moving toward the center in the upper vertebra. The spinous process is in midline in the bottom vertebra, and it is displaced in the upper vertebrae.
Radiograph shows various grades of vertebral rotation in the spine. The pedicles are normal in the bottom vertebra, but they are moving toward the center in the upper vertebra. The spinous process is in midline in the bottom vertebra, and it is displaced in the upper vertebrae.
Bone scans are useful to evaluate cases of painful scoliosis and to identify tumors or infections (see the image below). They are more sensitive than plain radiography.
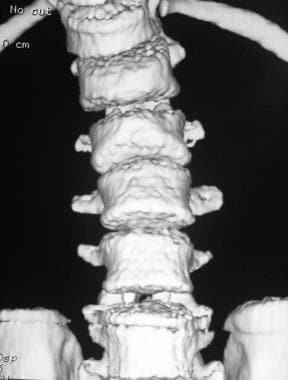
CT scanning with sagittal and coronal reconstructions can provide all the information that a plain radiograph provides (see the images below). [4] With CT, 3D reconstructions are useful in assessing segmentation abnormalities. CT can also be used to assess the true extent of rotation and rib deformities. It plays an important role in evaluating postoperative complications.
 Coronal reconstructions from multidetector-row CT show several hemivertebrae. Idiopathic scoliosis is diagnosed only after underlying structural conditions such as these are excluded.
Coronal reconstructions from multidetector-row CT show several hemivertebrae. Idiopathic scoliosis is diagnosed only after underlying structural conditions such as these are excluded.
 3-dimensional (3D) reconstructed CT scan of the same patient as in the previous image shows the hemivertebrae.
3-dimensional (3D) reconstructed CT scan of the same patient as in the previous image shows the hemivertebrae.
The role of MRI is controversial. [5] Although some institutes prefer to perform routine preoperative MRI in all patients, studies have shown that such an approach does not provide clinically significant results. MRI is useful for diagnosing associated spinal and neurologic lesions. Small tumors and infections can be localized by using MRI (see the images below). [5, 6, 7, 8, 9, 3, 10]
Limitations of techniques
The main limitation of radiography is the radiation dose. The risk of carcinogenesis is increased because of the repeated examinations done to monitor curve progression. This risk can be reduced with the judicious use of radiography and proper protection techniques.
Radiography is less sensitive than bone scanning and MRI because tumors or infections are apparent only after 50% of the bone is destroyed. Radiographs cannot be used to assess abnormalities of the spinal cord.
CT scanning is not routinely indicated, but it is a good method for assessing rotation and segmentation abnormalities. Radiography can provide all of the information needed. MRI is not cost-effective, and it is not a good screening tool because its yield in depicting important clinical abnormalities that change management is minimal.
Radiography
Radiography is performed to confirm the diagnosis of scoliosis (which is made on clinical grounds), exclude underlying bony segmentation abnormalities, assess the severity of the curve, monitor progression of the curve (which is done by measuring indices), assess skeletal maturity by noting the ossification of the iliac apophysis, evaluate associated cardiac and pulmonary anomalies, assess the patient's progress, and evaluate complications during and after surgery (see the images below). [11, 12, 13]
 Radiograph shows various grades of vertebral rotation in the spine. The pedicles are normal in the bottom vertebra, but they are moving toward the center in the upper vertebra. The spinous process is in midline in the bottom vertebra, and it is displaced in the upper vertebrae.
Radiograph shows various grades of vertebral rotation in the spine. The pedicles are normal in the bottom vertebra, but they are moving toward the center in the upper vertebra. The spinous process is in midline in the bottom vertebra, and it is displaced in the upper vertebrae.
 Left lateral bending of the same patient as in the previous image shows persistence of the scoliotic curve, which indicates its structural nature.
Left lateral bending of the same patient as in the previous image shows persistence of the scoliotic curve, which indicates its structural nature.
Concave-convex biases influence the progression of scoliotic curves, and measurement may provide improved clinical assessment of the risk of progression. [14] Four patterns are seen in idiopathic scoliosis: (1) thoracic curve, (2) lumbar curve, (3) thoracolumbar curve on the same side, and (4) thoracic and lumbar curves on opposite sides. The number of vertebrae involved in the curve should be assessed. [15]
In a healthy person, a straight line can be drawn through the cervicothoracic, dorsolumbar, and lumbosacral junctions. The degree of deviation in the cervicothoracic angle from the sacral center is measured. Hypokyphosis of less than 20° or lordosis is present. The normal thoracic kyphosis is 20-45°. The apical vertebrae show increased height in the anterior aspect of vertebral body and decreased height in the posterior aspect. [16] Vertebral bodies and intervertebral disk spaces are wider on the convex side than on the concave side.
The posterior ribs are pushed posteriorly on the convex side, where they produce a hump. They are positioned anteriorly on the concave side. The ribs are closely approximated on the concave side and separated on the convex side.
At the end of the curve, the disk spaces are equal or widened on the concave side. The vertebrae and neural arches are thick on the concave side. The spinous process is shifted toward the concave side, and the pedicle and vertebral body are shifted toward the convex side.
The rotation is marked at the apex of the curve and almost neutral at the end vertebrae. Rotation can be intersegmental (between vertebrae) or intrasegmental (between elements of one vertebra); the latter is uncorrectable. The psoas shadow is absent on the concave side of the curve.
Many classification systems are used to describe the types of scoliotic curves. Classification helps surgeons determine appropriate management, because prognosis and treatment of the various curves differ.
The International Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) Classification
The SOSRT classification is divided into chronologic, angular, and topographic domains. The chronologic classification is based on age at diagnosis [17] :
-
Infantile: age 0-2 yr
-
Juvenile: age 3-9 yr
-
Adolescent: age 10-17yr
-
Adult: age 18 yr or older
Angular classification is based on Cobb degree:
-
Low: up to 20 degrees
-
Moderate: 21-35 degrees
-
Moderate to severe: 36-40 degrees
-
Severe: 41-50 degrees
-
Severe to very severe: 51-55 degrees
-
Very severe: 56 or more degrees
Topographic classification is based on the apex:
-
Cervical: C6-7
-
Cervico-thoracic: C7 to T1
-
Thoracic: T1-2 to T11-12
-
Thoraco-lumbar: T12 to L1
-
Lumbar: L1-2
Ponseti-Friedman classification
The Ponseti-Friedman classification has 5 types:
-
Type I is a single major lumbar curve at T11-L3 with an apex at L1-2 (this is the most benign type and affects 23% of patients).
-
Type II is a single major dorsolumbar curve at T6-7 to L1-2 with an apex at T11-12 (16%).
-
Type III is combined thoracic and lumbar (37%), with a dorsal curve on the right side at T5-6 or T10-11 and an apex at T7-8, and a lumbar curve on the left side at T10-11 to L3-4 with an apex at L1-2.
-
Type IV is a single major thoracic curve at T5-6 to T11-12 with an apex at T8-9 (22%).
-
Type V is cervicothoracic at C7-T1 or T4-5 with an apex at T3.
King-Moe classification
The King-Moe classification has 4 types:
-
Type I is lumbar dominant and S shaped (10%).
-
Type II is thoracic dominant and S shaped (33%).
-
Type III is thoracic where the thoracic and lumbar curves do not cross the midline (33%).
-
Type IV is long thoracic or double thoracic, with T1 tilted into the upper curve where the upper curve is structural (10%). [18]
Lenke classification
The Lenke classification has 3 components: type of curve; lumbar modifier; and sagittal thoracic modifier.
Type of curves are as follows: I, primary thoracic; II, double thoracic scoliosis; III, double major scoliosis; IV, triple major scoliosis; and V, dorsolumbar-lumbar scoliosis.
The lumbar modifier is based on the relationship of the central sacral vertical line to the apex of the lumbar curve and is classified into A, B, and C categories.
The sagittal thoracic modifier is the sagittal curve measurement from T5-12; designations are the minus sign for less than 10°, the letter "N" for 10-40°, and the plus sign for greater than 40°. [18, 19, 20]
Radiographic views
The classic views obtained in the evaluation of scoliosis are as follows:
-
Posteroanterior (PA) erect view of the entire spine from cervical to sacral spine and including the iliac crest; this view is ideally obtained with the patient's shoulders outstretched.
-
AP recumbent view of entire spine, cervical to sacral.
-
Lateral view of dorsolumbar spine; the patient's forearm must be kept horizontal by resting it on a stand.
-
Lateral profile at the apex of scoliosis to eliminate kyphosis and show the true extent of the scoliosis.
-
Stagnara image (planed election view) perpendicular to the true coronal plane of the apical vertebra.
-
Leeds image, a true lateral view 90° perpendicular to the Stagnara view.
-
Left and right lateral bending views; these are obtained to exclude postural scoliosis; postural scoliosis disappears when bending toward the side of convexity; these views are also used to assess structural scoliosis, asymmetry and loss of normal mobility of primary curve, [21, 3] and wedging rotation of individual vertebra, as well as to dynamically assess the postural nature of secondary compensatory curves in the preoperative period and to select fusion levels.
-
AP view of the left hand to assess bone age.
-
Biplanar views with digital enhancement.
-
Ferguson view perpendicular to the L5-S1 disks to detect anomalies at this junction.
-
Coned views of focal vertebral anomalies.
In routine practice, not all these views are necessary. Full-length frontal and lateral views, as well as right and lateral bending views, are enough.
Common views obtained before surgery are PA and lateral image, which are obtained with long-cassette film to cover the whole spine, beginning from the craniocervical junction and including the pelvis to assess the Risser grade; supine, standing, or sitting images if patient is unable to stand; and lateral bending views to assess the extent of compensatory curves.
For subsequent follow-up imaging, the frontal PA view is sufficient, and lateral views are required only if a superimposed kyphotic element is present.
Terminology used to describe scoliosis
The apical vertebra is the vertebra that is displaced and rotated most. Its endplates are least tilted.
The end vertebrae are the most superior and inferior vertebrae in the curve. These bones are least displaced and rotated, with maximal tilting of the endplates toward the concavity of the curve. They are laterally wedged, longer in the convex side, and compressed on the concave side.
The neutral vertebra is not rotated on the anteroposterior (AP) image.
The stable vertebra is bisected by the central sacral line.
The primary curve is the structural curve, with wedging, angulation, rotation, and an abnormal position. The primary curve is deformed and develops structural changes simultaneously. It is not corrected spontaneously or with mechanical correction. The following characteristics are helpful in identifying the primary curve: (1) the vertebrae are deviated to the convexity of the curve; (2) if 3 curves are present, the middle one is usually the primary curve; (3) if 4 curves are present, the middle 2 are the primary ones; and (4) the primary curve may be the greatest curve.
The secondary curve is the nonstructural curve that develops in response to the primary structural curve. The structural changes in this curve occur slowly. It can be corrected spontaneously, and any mechanical correction is retained. The vertebrae are displaced to the concavity of the curve.
The compensatory curves are curves formed to balance the primary curve. If a primary curve is formed in one direction, another curve of same magnitude should be formed in the opposite direction to fully compensate for the deformity. For example, if the primary curve is 50°, 1 or 2 compensatory curves may be present and add up to equal 50° in the opposite direction.
A decompensated curve is a compensatory curve that does not fully correct the deformity. An example is when a 40° compensatory curve for a 50° primary curve results in decompensation.
An overcompensated curve is a compensatory curve that is more than the primary curve. An example is when a 60° compensatory curve or a combination of curves adding to 60° overcompensates for a 50° primary curve.
Indices used to assess scoliosis
There are a number of techniques, measures, and indices to assess scoliosis, including the Cobb-Webb technique, Lippman-Cobb technique, Ferguson technique, Greenspan method, Nash-Moe technique of measuring vertebral rotation, Cobb method of assessing vertebral rotation, and the Risser index.
Cobb-Webb technique
This is the most commonly used technique to measure the severity of scoliosis. The result determines further management and helps predict the prognosis.
The superior and inferior end vertebrae of the scoliotic curve are identified by carefully observing the rotation of vertebral bodies and the width of the intervertebral space. The intervertebral space is almost normal, and the vertebrae are in neutral position without substantial rotation in the superior and inferior end vertebra.
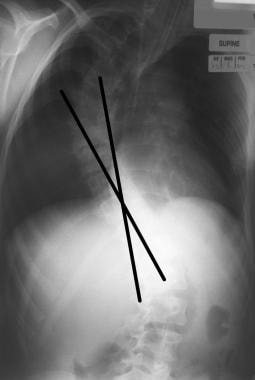
Lines are drawn tangential to superior endplate of the superior end vertebra and the inferior endplate of the inferior vertebra. The Cobb-Webb angle is the angle formed at the intersection of these lines or the angle formed at the intersection of the lines perpendicular to these lines. A Cobb angle of at least 10° is essential for diagnosing scoliosis. [3]
Limitations of Cobb-Webb angle include the following:
-
Uniplanar measurement of a 3D deformity
-
Interobserver variation
-
Diurnal variation, with angles 5° greater in the afternoon than in the morning
-
Variations that occur with changes in supine and upright positioning, rotation, body shape, and radiographic technique
-
Spinal growth of 1° per month during periods of rapid growth (frequent assessments [eg, every 3-4 mo] are needed for accurate measurements of the curve)
-
Angle of curvature determined only by the orientation of the end vertebra
-
Values higher than those obtained with other measurement techniques
A 10° measurement difference should be present to be 95% confident that the curve is progressing.
Lippman-Cobb classification
The Lippman-Cobb classification of scoliotic curvature is as follows (see the images below):
-
I = Less than 20°
-
II = 21-30°
-
III = 31-50°
-
IV = 51-75°
-
V = 76-100°
-
VI = 101-125°
-
VII = Greater than 125°
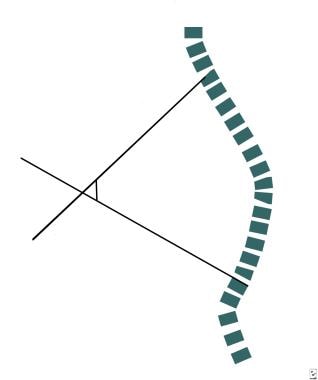
Ferguson technique
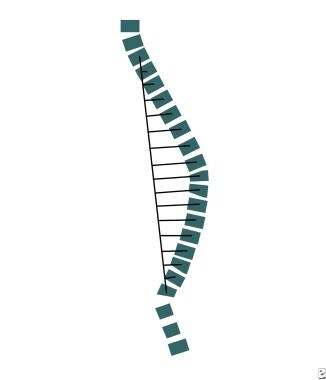
A line is drawn from the center of the apical vertebra to the center of the superior end vertebra. Another line is drawn from the center of the apical vertebra to the center of the inferior end vertebra (see the images below).
The angle between these lines is used to assess the severity of the deformity.
Greenspan index
This technique provides a measurement of the scoliotic curve more comprehensive than that obtained with other methods (see the images below). The midpoint of the vertebra above the upper end vertebra and the midpoint of the vertebra below the lower end vertebra are joined to form a vertical spinal line. Lines are drawn from the center of each vertebra in the scoliotic curve to the vertical spinal line. The value of these individual lines are added and divided by the length of the vertical spinal line. A correction factor is added for magnification.
In a healthy person, the value is zero. This method is superior to the Lippman-Cobb technique because it allows the clinician to measure the deviation at each individual vertebral level. This technique is also valuable in measuring short-segment or small curvatures.
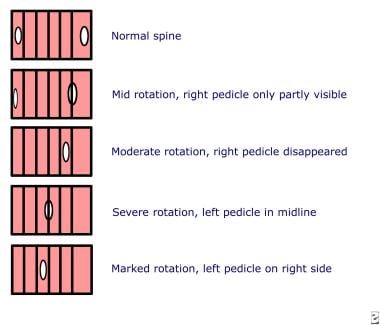
Nash-Moe technique of assessing vertebral rotation
This is a measure of rotational deformity of the vertebra.
On frontal images, the vertebra is divided into 6 segments, and the rotation is quantified on the basis of where the pedicle is located. The pedicles are normally situated in the outer segments. The rotation is graded according to the extent of migration of the pedicle toward the convex side of the curve.
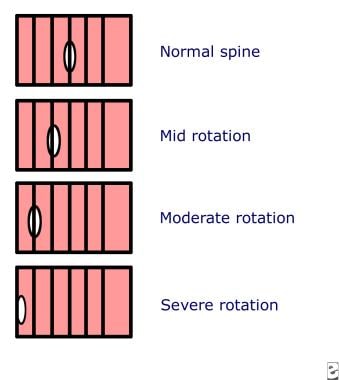
Cobb method of assessing vertebral rotation
The Cobb technique uses the position of spinous process for assessing the degree of vertebral rotation. The vertebra is divided into 6 equal segments by drawing 5 vertical lines (see the image below).
The spinous process is normally situated in the midpart of the vertebra overlying the third line. With increasing rotation, the spinous process is rotated toward the convex side of the curve.
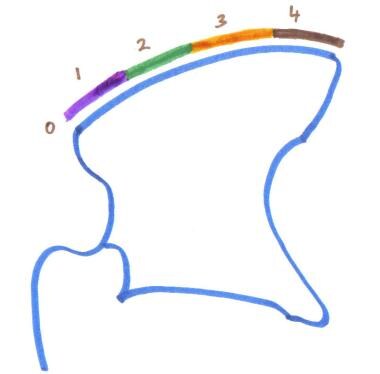
Risser index
The Risser index (see the image below) is used to measure ossification of the iliac apophysis, which is graded as follows:
-
Grade I is ossification of the lateral 25% of the iliac apophysis.
-
Grade II is ossification of the lateral 50%.
-
Grade III is ossification of the lateral 75% of the apophysis.
-
Grade IV is ossification of the entire apophysis.
-
Grade V is fusion of ossified epiphysis to the iliac wing.
Scoliotic curves usually progress during periods of rapid growth, such as infancy and adolescence, and they stop growing after spinal maturation is complete. Spinal growth is completed at approximately 15 years 3 months of age in female adolescents and 15 years 10 months of age in male adolescents. This maturation coincides with the completion of ossification in the iliac apophysis, which begins at around 15 years in male adolescents and around 14 years in female adolescents. The whole process of ossification from stage I to stage IV requires 12-18 months.
After ossification, the apophysis fuses with iliac crests in 2 years in girls and slightly faster than this in boys. Progression usually does not happen after grade IV maturity of iliac apophysis is achieved. If the curve is 50-80° at the time of maturity, it tends to progress even after the apophysis fuses, especially if the curve is in the thoracic and lumbar region. However, this progression is far slower than the progression that occurs during adolescence.
Limitations of Risser index can be summarized as follows:
-
Ossification starts earlier than previous thought; hence, this index is not reliable.
-
The index is less reliable in male patients than in female patients because their ossification starts early; in male patients, growth should be considered completed when a Risser index of only 5 is achieved.
-
Data indicate that this index is not an accurate measure of completed maturity, spinal growth, or progression of the deformity.
Observation for ossification of the vertebral ring apophysis
This is an alternative method for assessing skeletal maturity (see the image below).
 Vertebral apophysis maturation. Left image shows the ossification center. Ossification is complete in the middle image. Right image shows fusion indicating vertebral maturation.
Vertebral apophysis maturation. Left image shows the ossification center. Ossification is complete in the middle image. Right image shows fusion indicating vertebral maturation.
Before skeletal maturity, the vertebral ring apophysis is absent, or it is incompletely formed or completely formed without fusing to the body. After skeletal maturity, the vertebral ring apophysis fuses to the body. This occurs by age 16 years in female adolescents and age 19 years in men.
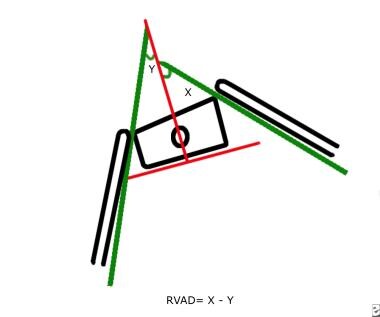
Difference in the rib-vertebral angle
This parameter is useful in predicting the progression of the curve in the idiopathic infantile type of scoliosis (see the images below).
A line is drawn along the inferior border of the apical vertebra, and another line is drawn perpendicular to the first. The midpoints of the head and neck of ribs on either side of the apical vertebra are connected by lines. These lines are extended to meet the perpendicular line drawn initially, and the angles they make are called rib-vertebral angles.
In thoracic curves, the angle is usually smaller on the convex side than the concave side because of the greater obliquity of the ribs on the convex side. In combined thoracic and lumbar curves, the angle is low at the level of the apical thoracic vertebra and can be greater on the convex side. This curve can be further negative because of the associated drooped 12th rib on the concave side of the curve.
In resolving curves, the angle is less than 20°, and it is more than 20° in progressive curves. Subsequent images obtained after 2-3 months show a decreased angle in resolving curves and the same or increased angle in progressive curves.
Perdriolle method
The Perdriolle method is used to measure apical vertebral rotation.
Lytilt method
The Lytilt method is used to measure the angle between the L4 vertebra and a line connecting the iliac crests.
Other methods of assessing skeletal maturity
Ossification and maturation of the epiphysis of the left hand and wrist are compared with standards. Two main methods are used. The first is the Greulich-Pyle method, in which the radiograph of the hand and wrist is compared with standard radiographs in the atlas. The second is the Tanner-Whitehouse method, in which the epiphyses of the hand and wrist are compared with those of the atlas. A score is assigned to each of them, and the sum is compared with values on standard tables. Thus, bone age is assessed.
Surgery for scoliosis
The Cobb angle based on an anteroposterior radiograph is a necessary prerequisite to plan the surgery, and corrective surgery is always required when a Cobb angle is greater than 50°. [22] The immediate preoperative assessment should include chest radiographs for cardiovascular assessment, supine and recumbent AP views of the spine, right and left lateral bending images, and traction views. The bending and traction views are helpful in assessing the site of fusion, the degree of correction required, and the placement of spinal devices.
Surgery for scoliosis includes the following techniques:
-
A single rod can be used to fix the upper and lower end of the curves with a posterior approach; disadvantages are prolonged immobilization or use of braces and suboptimal results. [23]
-
Two Harrington or Luque rods can be used to accomplish segmental stabilization at each level of the spine using sublaminar wires.
-
Use of the Cotrel-Dubousset system with multiple hooks with rods may improve 3D results.
-
An anterior approach can be used with thoracotomy or thoracoscopy in which single or double rods with screws are attached to each vertebral body; results are better than with other methods, and this approach treats the rib bump at the same time.
Postoperative radiographic assessment
In the immediate postoperative period, chest radiographs are used to assess for complications. Frontal and lateral spinal images are required to assess the postoperative spine. The degree of correction of the curve can also be evaluated. [26]
Recognized complications are damage to the rods or wires, dislocation or migration of the rods, loosening of a device, spondylolysis, pseudoarthrosis, aortic aneurysm, retroperitoneal fibrosis, gastric volvulus, and progression of the deformity (crankshaft phenomenon). This last complication occurs when surgery is performed before maturity (Risser index < 1 and age < 10 yr). The unfused vertebrae and portions of the vertebrae not included in the fusion continue to grow, producing progressive deformity. This effect is marked in posterior fusion, in which the anterior portions of vertebrae continue to grow and produce a new curve.
Follow-up assessment should be routinely performed until the patient reaches maturity.
Radiation protection
The radiation dose is an important factor in evaluation of scoliosis. Techniques for radiation protection include the use of the following: PA view to reduce exposure to the breast; lead-acrylic filters; increased beam filtration; low-dose imaging systems; and breast, gonad, and thyroid shields. [1]
Computed Tomography
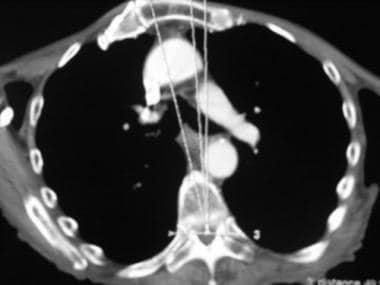
The scoliotic deformity can be visualized on CT scans of the thorax and abdomen (see the images below). Associated lesions, such as osteoid osteoma, osteoblastoma, infection, tumors, disk prolapse, and costovertebral dislocation, can be found. CT can also be used to create a 3D image of associated chest deformities. [27]
 Coronal reconstructions from multidetector-row CT show several hemivertebrae. Idiopathic scoliosis is diagnosed only after underlying structural conditions such as these are excluded.
Coronal reconstructions from multidetector-row CT show several hemivertebrae. Idiopathic scoliosis is diagnosed only after underlying structural conditions such as these are excluded.
 3-dimensional (3D) reconstructed CT scan of the same patient as in the previous image shows the hemivertebrae.
3-dimensional (3D) reconstructed CT scan of the same patient as in the previous image shows the hemivertebrae.
With modern multidetector-row CT scanners, thin sections of the whole body can be obtained within a few seconds and reconstructed in any plane: sagittal, coronal, oblique, or axial. Even 3D reconstruction with shaded-surface display or volume rendering is possible.
CT myelography is not routinely done, and it is not needed in idiopathic scoliosis. This is useful for evaluating intraspinal lesions, such as diastematomyelia, a tethered cord, or intraspinal tumors. Compression of the spinal cord can also be assessed.
Role of CT in evaluating scoliosis
CT is performed for an evaluation of segmentation abnormalities with 3D reconstructions, though MRIs have largely replaced these scans. CT is also used to evaluate postoperative complications because MRIs may show metallic artifacts. In addition, CT helps in evaluating intrinsic rotational deformity. Scoliotic deformity can be visualized on CT scans of the thorax and abdomen. Associated lesions, such as osteoid osteoma, osteoblastoma, infection, tumors, disk prolapse, and costovertebral dislocation, can be found. Finally, associated rib-cage deformity is best assessed with CT scans. The rib-cage deformity is well correlated with the longitudinal deformity at the level of the apical vertebra.
CT myelography is done to assess suspected radiculopathy, intraspinal lesions, or cord compression.
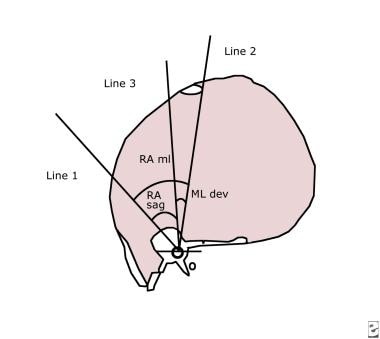
Indices used to assess rib-cage deformity
The apical vertebra of the primary curve is identified by using plain radiography. CT scans are then acquired at this level to help assess the longitudinal deformity. Several lines are used.
Line 1 is drawn from the center of the posterior aspect of the vertebral foramen to the center of the vertebral body and extended to the anterior chest wall. Line 2 extends from the center of the posterior aspect of vertebral foramen to the anterior midline of the body. Line 3 is a horizontal line extending through the center of the posterior aspect of the vertebral foramen. A perpendicular is then drawn from the center of the posterior aspect of the vertebral foramen to meet the anterior chest wall (see the images below).
The rotation of apical vertebra from the anterior midline of the body (RAML) is the angle between line 1 and line 2. The rotation of the apical vertebra from the sagittal plane (RASag) is the angle between line 1 and line 3. This is the most definitive method for assessing the severity of scoliosis with CT scans. The results are significantly correlated with the Cobb-Webb angles on plain radiographs. The angle of lateral deviation of the apical vertebra from the midline of body (Mldev) is the angle between line 2 and line 3.
RAML is the sum of RASag and Mldev.
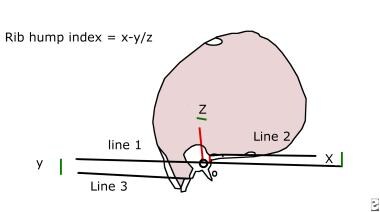
Rib-hump index
The rib-hump index is measured at the level of the rib hump by using several lines. Line 1 is a horizontal line drawn through the center of the posterior aspect of the vertebral foramen to the lateral chest wall on both sides. Line 2 is a horizontal line parallel to the first; this line passes through the peak of the inner rib cage on the hump side. Line 3 is parallel to the first and passes through the peak of the inner rib cage on the side opposite the hump. Line 4 is a perpendicular line drawn from the peak of the inner rib cage on the hump side to meet the first line at point 0.
The rib-hump index is defined as (X - Y)/Z, where X is the distance between line 1 and line 2, Y is the distance between lines 1 and 3, and Z is the distance between point 0 and the center of posterior aspect of the vertebral foramen.
The rib-hump index is directly correlated with RASag.
Postoperative CT
Postoperative CT scanning can be done to assess for the development of complications such as hemorrhage, fracture, or pseudoarthrosis.
Magnetic Resonance Imaging
MRI is performed in the sagittal, axial, and coronal planes by using T1- and T2-weighted sequences. Proper technique is difficult, especially if the patient has more than one curve. MRI is indicated if the patient develops neurologic deficits after the procedure. If MRI is being done for the first time, occult spinal cord lesions cannot be detected. Imaging might be difficult because of the presence of spinal instruments. Hemorrhage, pseudoarthrosis, and tumors can be detected. [9, 3, 10]
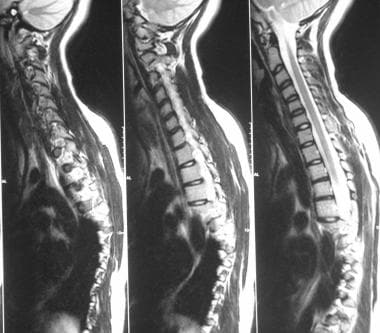
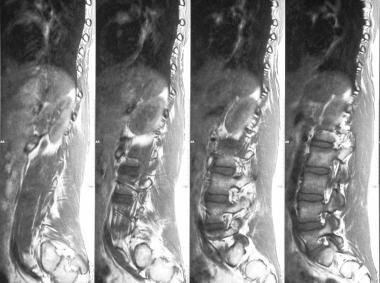
MRI is not used for diagnosing scoliosis. It is useful for assessing other etiologic factors, especially spinal cord anomalies, that can change the diagnosis. Such anomalies are most common in the infantile and juvenile types and include syringomyelia, hydromyelia, spinal cord tumors, dysraphism, a tethered cord, diastematomyelia, lipomas, neurofibromas, and Chiari malformations (see the images below). [6, 7, 8]
Idiopathic scoliosis is diagnosed only after its differential diagnoses are excluded. In one study, 50% of all cases previously designated as being idiopathic involved some spinal lesion. Untreated syringomyelia contributes to paraplegia after surgery.
MRI is also used to investigate occult intraspinal tumors, which can occur with scoliosis but without any neurologic symptoms or signs; to exclude other underlying abnormalities, such as tumors, infections, and disk prolapse; to evaluate atypical scoliosis or an atypical curve in a child with normal neurologic findings; to evaluate the patient before surgery because assessment of the spinal cord in patients with postoperative neurologic symptoms can be difficult because surgical devices produce artifacts; to evaluate rotational deformity and distinguish intervertebral from intravertebral rotation (standard derotational surgery is suboptimal in those with predominant intravertebral rotation.); and to ascertain the severity of the curve.
Atypical features for which MRI is warranted include the following:
-
Abnormal neurologic finding
-
Painful scoliosis
-
Signs of dysraphism
-
Neck pain, headache
-
Weakness, pes cavus, ataxia
-
Back pain
-
Atypical curves (left-sided thoracic curve, juvenile onset)
-
Rapid progression
-
Associated lower limb deformity
-
Increased kyphosis
-
Thoracic deformity
-
Wide spinal canal
-
Thin pedicles
-
Abnormal somatosensory evoked potentials
Do et al found that only 7 of 327 patients with diagnosed idiopathic scoliosis had other abnormalities on routine MRI. [5] None of the newly diagnosed pathologies were clinically important in terms of future management.
Degree of confidence
Important considerations are intraspinal tumors. Intraspinal tumors occasionally cause scoliosis and no other symptoms. In such cases, idiopathic scoliosis might be diagnosed. Only MRI can depict intraspinal tumors. The identification of notable neurologic and other diseases alters management.
If the patient develops neurologic symptoms postoperatively, assessment of the spinal cord is difficult because of the surgical devices, which produce artifacts. Hence, a routine preoperative MRI is considered useful.
Although MRI has been advocated in patients with atypical scoliosis, data confirming the benefit of this approach are lacking.
MRI can depict a number of findings; however, onestudy revealed no significant difference in the incidence of anomalies between those with atypical findings and patients without atypical findings. Even if anomalies such as syringomyelia and Chiari malformation are found, they do not affect management. Therefore, the effectiveness of MRI as a diagnostic tool is questioned.
Some centers still routinely use MRI, and others use it only if surgery is contemplated or if atypical signs are present.
Ultrasonography
Ultrasonography has only limited application in scoliosis (see the image below). It can be useful to assess soft tissue complications, such as hematomas and abscesses, after surgery. If scoliosis is seen in a neonate or child with spina bifida, a sonogram of the spine can be obtained to assess the spinal cord. The position of the cord, including tethering, can be evaluated. Associated lesions, such as myelomeningocele, lipomas, epidermoids, and those due to diastematomyelia, are also seen. [28]
Nuclear Imaging
Bone scanning is not routinely performed in idiopathic scoliosis. Bone scans are obtained to evaluate atypical or painful scoliosis and to exclude infection. Focal hot spots can be seen in osteoid osteomas, osteoblastomas, infections, and other primary tumors that can cause painful scoliosis. Bone scans may also help assess surgical complications, including infection. A WBC scan may be required to differentiate infection from postoperative changes in the spine. Focal hot spots are also seen in stress fractures, spondylosis, and pseudoarthrosis in the fused segments.
Bone scanning is highly sensitive in the diagnosis of bone lesions. Osteoid osteoma is the most common cause of painful scoliosis. Bone scanning is helpful in assessing this condition and for showing increased uptake.
-
Mild juvenile scoliosis.
-
Anteroposterior (AP) radiograph shows mild adolescent scoliosis.
-
Lateral view of mild adolescent scoliosis.
-
Moderate scoliosis.
-
Severe infantile scoliosis.
-
Severe typical scoliosis.
-
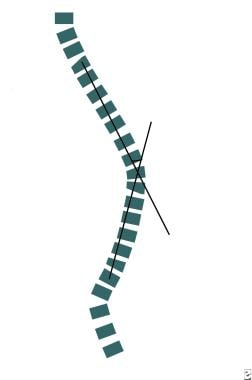
Line diagram illustrates the common terms used in describing scoliosis.
-
Plain radiograph illustrates the common terms used in describing the scoliotic curve. The upper and lower end vertebrae and apical vertebra are illustrated. The vertebrae and disk spaces are smaller on the concave side and larger on the convex side. The spinous process is rotated towards the concave side. The ribs are crowded on the concave side.
-
Line diagram illustrates measurement of the Lippman-Cobb angle.
-
Radiograph shows measurement of Lippman-Cobb angle.
-
Line diagram shows the Risser-Ferguson technique.
-
Radiograph shows measurement by using the Ferguson technique.
-
Line diagram illustrates the Greenspan technique.
-
Radiograph shows measurement of the Greenspan index of scoliosis.
-
Line diagram shows the Nash-Moe method of measuring vertebral rotation.
-
Line diagram illustrates the Cobb method of measuring vertebral rotation.
-
Radiograph shows various grades of vertebral rotation in the spine. The pedicles are normal in the bottom vertebra, but they are moving toward the center in the upper vertebra. The spinous process is in midline in the bottom vertebra, and it is displaced in the upper vertebrae.
-
Line diagram shows rib–vertebral angle difference (RVAD) (Mehta, 1976).
-
Radiograph shows measurement of difference in the rib-vertebral angle.
-
Line diagram illustrates the Risser index.
-
Vertebral apophysis maturation. Left image shows the ossification center. Ossification is complete in the middle image. Right image shows fusion indicating vertebral maturation.
-
Right lateral bending view of a patient with scoliosis.
-
Left lateral bending of the same patient as in the previous image shows persistence of the scoliotic curve, which indicates its structural nature.
-
MRIs show cervical scoliosis.
-
Sagittal MRIs show lumbar scoliosis.
-
Axial MRI shows apical vertebra.
-
Sagittal MRI shows an Arnold-Chiari I malformation and syringomyelia.
-
3-dimensional (3D) reconstruction of mild scoliotic curve without segmentation anomaly.
-
Coronal reconstructions from multidetector-row CT show several hemivertebrae. Idiopathic scoliosis is diagnosed only after underlying structural conditions such as these are excluded.
-
3-dimensional (3D) reconstructed CT scan of the same patient as in the previous image shows the hemivertebrae.
-
CT is good for assessing rotation of the vertebra.
-
Line diagram illustrates measurement of the CT index.
-
Line diagram illustrates measurement of the CT rib-hump index.
-
CT scan illustrates the indices useful for assessing the extent of rotation.
-
Bone scans in a patient with painful atypical scoliosis are normal.
-
Intraoperative image shows screw fixation.
-
Intraoperative image shows screw fixation.
-
Harrington rods with wires, hooks, and screws.
-
Harrington rods with wires, hooks, and screws as shown on a lateral radiograph.
-
Anteroposterior (AP) view of fixation by using pedicle screws.
-
Lateral view of pedicle screws.
-
Coronal CT appearance of pedicle screws.
-
Axial CT appearance of a normal pedicular screw after surgery.
-
Anteroposterior (AP) radiograph of body screws.
-
Normal appearance of body screws on a lateral view.
-
Axial CT appearance of a screw in a vertebral body.
-
Displaced pedicular screw indenting the descending thoracic aorta.
-
Anteriorly displaced screw in the parenchyma of the right lower lobe of the lung.
-
Postoperative focal hot spot in the spine due to infection.
-
CT scan shows right rib destruction and underlying pulmonary infection. Left-sided pleural effusion is also shown.
-
Sonogram shows a small collection adjacent to the rib, which was drained.
-
Cardiomyopathy with bilateral pleural effusion after surgery.