Practice Essentials
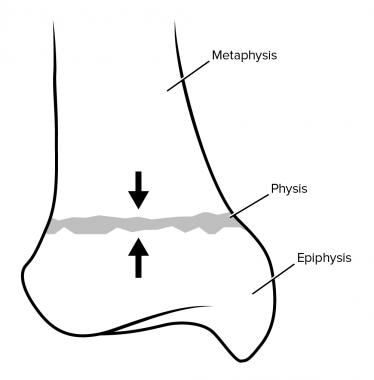
Salter-Harris fractures are fractures through a growth plate; therefore, they are unique to pediatric patients. These fractures (see the images below) are categorized according to the involvement of the physis, metaphysis, and epiphysis. The classification of the injuries is important, because it affects patient treatment and provides clues to possible long-term complications. When all types of Salter-Harris fractures are considered, the rate of growth disturbance they cause is approximately 30%. However, only 2% of Salter-Harris fractures result in a significant functional disturbance. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11]
Preferred examination
Radiography is always the preferred examination in a suspected fracture. The use of another modality should not be considered until appropriate plain film radiography has been performed. [12, 13, 14, 15, 16, 17, 18, 19]
In cases of severe injury in which the patient has acute pain, appropriate radiographic examination of the involved area may be difficult because of inadequate patient positioning. In these cases, computed tomography (CT) scanning may be beneficial in evaluating the injury after a radiologist has evaluated the plain radiographs. [18, 20] Some of the disadvantages of CT include radiation exposure, inability to evaluate the cartilaginous growth plate and epiphysis, and inability to assess osteochondral perfusion. [21] CT should be considered only when radiographic findings are insufficient.
If an additional study is performed, its purpose is to determine the appropriate management and to assist in surgical planning. Thus, the surgeon performing the operation is best suited to request the imaging study. When further definition of fractures may help in making management decisions or when the injury does not respond to conservative management, the radiologist or orthopedic surgeon can recommend an appropriate examination to perform after plain radiography.
Two radiologic examinations can be performed to further evaluate fractures: (1) CT scanning with multiplanar reconstruction and (2) magnetic resonance imaging (MRI). MRI depicts marrow edema, whereas CT shows cross-sectional bone detail and tomographic multiplanar information. MRI is not the current standard of care; CT is used more commonly. Typically, it is used for planning surgery.
The disadvantages of MRI that limit its routine use include the modality's expense, time requirement, and availability. In children, particularly very young children, sedation and even general anesthesia may be required to perform MRI scans. As techniques and software improve, the use of MRI in the acute trauma setting is likely to increase. [22, 19]
Thawrani et al published a study on interobserver agreement on classification and surgical management in complex ankle fracture with the use of CT scanning and found no increase in interobserver reliability to classify fracture or make treatment decisions. [23]
Taggart et al [24] reported that the use of point-of-care ultrasonography in the emergency department setting could correctly diagnose Salter-Harris fractures. Findings of periosteal fluid at the level of the metaphysis and widening of the physis allowed for the diagnosis of a fracture.
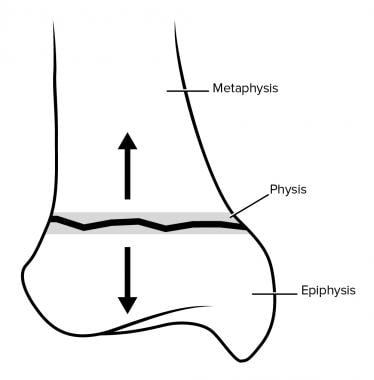
Type I
A type I fracture (see the images below) is a transverse fracture through the hypertrophic zone of the physis. In this injury, the width of the physis is increased. The growing zone of the physis usually is not injured, and growth disturbance is uncommon. On clinical examination, the child has point tenderness at the epiphyseal plate, which is suggestive of a type I fracture. [25, 22, 26, 27]
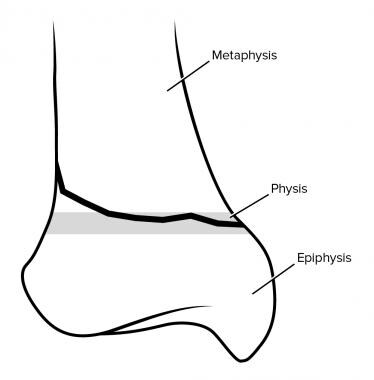
Type II
Type II represents up to 75% of cases. [21] A type II fracture (see the images below) occurs through the physis and metaphysis; the epiphysis is not involved in the injury. These fractures may cause minimal shortening; however, the injuries rarely result in functional limitations. [12, 28] Conservative nonoperative treatment is effective for most patients, although surgery may be necessary in some selected patients. [29, 30]
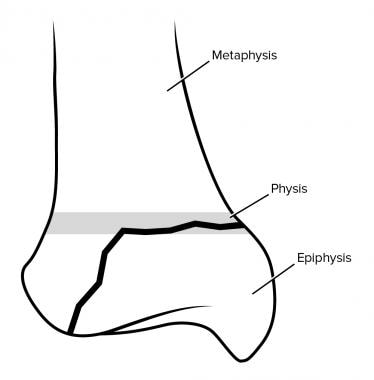
Type III
A type III fracture (see the images below) is a fracture through the physis and epiphysis. This fracture passes through the hypertrophic layer of the physis and extends to split the epiphysis, inevitably damaging the reproductive layer of the physis. This type of fracture is prone to chronic disability, because by crossing the physis, the fracture extends into the articular surface of the bone. However, type III fractures rarely result in significant deformity; therefore, they have a relatively favorable prognosis. [8, 9, 31]
An ankle fracture termed a Tillaux fracture is a Salter-Harris type III fracture that is prone to disability. About 15% of juvenile long bone injuries involve the epiphyseal growth plate, with 2.9% of these being Tillaux fractures. In juvenile Tillaux fracture, the avulsed fragment is quadrangular, but in adults it is triangular. [32, 33]
The treatment for type III fractures is often surgical.
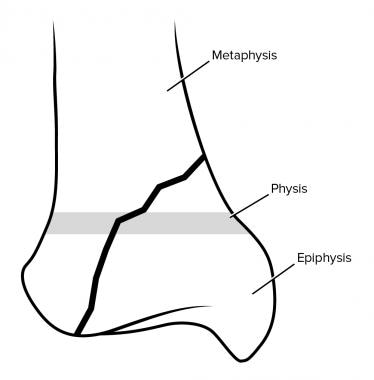
Type IV
A type IV fracture is the second most common Salter-Harris fracture and occurs in about 10-12% of cases (see the images below). [21] It involves all 3 elements of the bone, passing through the epiphysis, physis, and metaphysis. [7, 31] Similar to a type III fracture, a type IV fracture is an intra-articular fracture; thus, it can result in chronic disability. By interfering with the growing layer of cartilage cells, these fractures can cause premature focal fusion of the involved bone. Therefore, these injuries can cause deformity of the joint. Surgical restoration of the joint surface realignment is often required. [21]
Type V
A type V injury (see the images below) is a compression or crush injury of the epiphyseal plate, with no associated epiphyseal or metaphyseal fracture. Type V fractures are rare and account for less than 1% of growth plate fractures. This fracture is associated with growth disturbances at the physis. Initially, diagnosis may be difficult, and it is often made retrospectively after premature closure of the physis is observed. In older teenagers, the diagnosis is particularly difficult. The clinical history is paramount in the diagnosis of this fracture. A typical history is that of an axial load injury. Type V injuries have a poor functional prognosis. [11, 21]
Types VI-IX
Rare types of Salter-Harris fractures include the following:
-
Type VI - Injury to the perichondral structures
-
Type VII - Isolated injury to the epiphyseal plate
-
Type VIII - Isolated injury to the metaphysis, with a potential injury related to endochondral ossification
-
Type IX - Injury to the periosteum that may interfere with membranous growth
See Common Pediatric Sports and Recreational Injuries, a Critical Images slideshow, to help recognize some of the more common injuries and conditions associated with pediatric recreational activities.
Radiography
Radiographic findings vary according to the type of Salter-Harris fracture.
With a type I fracture, initial radiographs may suggest separation of the physis, but this separation may not be apparent. However, soft-tissue swelling is present, and its center typically overlies the physis. Follow-up radiographs obtained 7-10 days after injury help establish the diagnosis. New bone growth (ie, adjacent sclerosis and periosteal reaction) along the epiphyseal plate confirms the diagnosis of a Salter-Harris type I fracture.
In a type II fracture (see the image below), the fracture line passes through the metaphysis into the epiphyseal plate, but no fracture is observed in the epiphysis. The metaphyseal fragment is sometimes called the Thurston-Holland fragment.
A type III fracture (see the image below) passes through the hypertrophic layer of the physis and extends to split the epiphysis. The fracture crosses the physis and extends into the articular surface of the bone.
A Type IV fracture (see below) passes through the epiphysis, physis, and metaphysis. Similar to a type III fracture, a type IV fracture is an intra-articular injury.
In a type V injury, initial plain radiographs may not show a fracture line, similar to images of type I fractures. However, soft-tissue swelling at the physis is present. A compression or crush injury of the epiphyseal plate is present without associated epiphyseal or metaphyseal fracture.
In a study that compared radiography with subsequent CT for diagnosis of Salter-Harris type III fractures, Salter-Harris type IV fractures, Tillaux fractures, and triplane fractures in 64 patients, CT was found to be essential in patients with transitional distal tibial fractures, as well as in patients with displaced Salter-Harris type III and type IV fractures, to make an accurate diagnosis and select appropriate treatment. In patients who received initial radiographic examination, surgical treatment was chosen for 18 patients and nonsurgical for 46. For patients who underwent CT scanning, 42 patients were found to require surgical treatment and only 22 nonsurgical. [20]
Computed Tomography
CT scanning has an important role in the evaluation of epiphyseal injuries. Rogers and Poznanski [34] discussed the role of CT along with the use of a bone algorithm and multiplanar reconstruction of multiplanar initial images. With CT, a considerable amount of information regarding the nature of the fracture can be gathered. CT techniques typically are used in patients before surgery after a fracture diagnosis has been made on the basis of plain radiographic findings. [20, 23]
Multiplanar CT findings are similar to plain radiographic findings.
The computer program is able to compensate for imprecise patient positioning. True lateral and true anteroposterior (AP) views of the bone in question can be obtained. As with any study, physicians who request these costly studies should have the knowledge and experience needed to interpret the images. Orthopedic surgeons may be the ones to request CT examinations; however, any physician can order them in consultation with a radiologist.
The advantages of CT scanning over MRI are its greater availability and the faster speed in obtaining images. The disadvantage of CT scanning is that the modality requires a relatively large dose of radiation for diagnostic imaging. Raw-data images typically are obtained with 1-mm sections and a high milliampere technique; however, the high collimation reduces the total amount of exposure.
In the future, multi–detector row technology is likely to affect the utility of CT in the detailed evaluation of fractures.
Magnetic Resonance Imaging
On MRIs, the typical findings of Salter-Harris fractures include a signal void on T1-weighted images. On T2-weighted images, increased signal intensity, which is consistent with edema, is depicted around the fracture site. MRI can be used in surgical planning. [13, 15, 18]
Craig et al [35] discussed the use of MRI in evaluating partial closure of the growth plates. Patients with functional or growth abnormalities were examined with MRI, and the exact nature of the defects were well described. These findings helped orthopedic surgeons plan appropriate surgery. On the basis of their research, Craig et al suggested that a sagittal 3-dimensional (3D) spoiled gradient-recalled (SPGR) sequence is the best sequence for the evaluation of the physeal plate. In addition to using the SPGR sequence, the study's authors examined patients using 2-dimensional (2D) sagittal and coronal fast spin-echo sequences (with an echo train length of 3) and 3-mm-thick sections with a 1-mm gap. The field of view was 14 cm. They also used 2D axial and coronal fast spin-echo imaging with fat saturation (with an echo train length of 8) and 5-mm-thick sections with a 1.5-cm gap. The field of view was 18 cm.
The evaluation of Salter-Harris injuries in children is a new use for MRI technology. Salter-Harris type I fractures of the distal fibula have been found to be rare in children with radiographic fracture-negative lateral ankle injuries. In a prospective cohort study of 135 children (age range, 5-12 yr) in pediatric EDs who underwent ankle MRI for Salter-Harris type I fracture of the distal fibula, only 4 patients were found to have Salter-Harris type I fractures, and 2 of these were partial growth plate injuries. [36]
MRI is limited in the assessment of acute injuries because of the length of time involved in the examination. Another limitation is the relative isolation of the patient within the machine. Therefore, it is most efficiently applied by specialists with specific treatment questions. Orthopedic surgeons are the most appropriate physicians to request MRI; however, in consultation, a radiologist and a clinician may determine a specific need for MRI findings in a given case. Consultation with an orthopedic surgeon is likely to be helpful in complicated injuries that require treatment. [22, 19]
In a study of 31 pediatric patients (mean age 10±2.86 yr) seen in an ED with a clinical suspicion of Salter-Harris type I fracture of the distal fibula who underwent MRI, none of the patients turned out to have Salter-Harris fracture. The majority of the injuries were ligamentous lesions, bone contusions, or joint effusions. [13]
Close and Strouse found evidence that MRI can reveal fractures not seen on plain radiographs. [13] The authors retrospectively evaluated 315 consecutive knee MRIs in children with a history of trauma. They reported that MRI revealed 8 additional fractures that were not fully identified on plain radiographs, and of the 8 fractures found with MRI, 7 had MRI findings that changed the clinical management. This study was limited because of its retrospective nature and selection bias; however, the authors indicated that MRI is better than plain radiography in delineating the exact nature of an injury. In complex cases, this advantage may be of clinical importance.
(The ability of MRI to reveal Salter-Harris fractures that were not seen on radiographs is demonstrated in the image below.)
 Coronal MRI obtained several weeks after an initial radiograph was obtained to assess ligamentous injury shows an unexpected finding of a Salter-Harris type III fracture.
Coronal MRI obtained several weeks after an initial radiograph was obtained to assess ligamentous injury shows an unexpected finding of a Salter-Harris type III fracture.
Carey et al [14] reviewed the correlation between MRI results and plain radiographic findings in Salter-Harris fractures and found a trend similar to that of Close and Strouse. [13] A Finnish study revealed no misclassification in patients with minor ankle fractures; MRI was helpful in evaluating complex injuries in the ankle. [15]
A study performed by Petite et al [16] revealed a small benefit in the use of MRI versus plain radiography They found a misclassification rate of only 3% in patients with acute trauma. This study was limited because only gradient-echo imaging was used. (Carey et al [14] and Close and Strouse [13] used multiple MRI techniques.) The conclusion of Petite et al [16] is similar to that of the other studies: MRI can be helpful in complex cases or when plain radiographic findings are normal and the clinical findings are highly suggestive of fracture.
Ultrasonography
Ultrasonography (US) has a limited role in the diagnosis of fractures. Hubner et al found that Salter-Harris type I fractures and nondisplaced fractures with less than 1 mm of separation were reliably detected with US. [17] However, complex fractures were more difficult to assess with the modality. The study compared primary US diagnosis of fractures with diagnosis using plain radiography.
Salter-Harris type I fracture of the distal humerus is a rare but important diagnosis in the neonatal population. This injury can be easily mistaken for a posterior elbow dislocation, but it can require different management. Therefore, it is important to consider a transphyseal (Salter-Harris type I) humeral fracture in any neonate presenting with a posteriorly displaced elbow injury on radiographs. On ultrasound, a complete absence of the distal left humerus epiphysis from its expected position at the distal end of the humerus metadiaphysis may be seen. [37]
-
Salter-Harris type II fracture of the distal tibia.
-
Salter-Harris type III fracture of the distal tibia.
-
Salter-Harris type IV fracture of the distal tibia.
-
Illustration of uninjured bone.
-
Salter-Harris fracture type I.
-
Salter-Harris fracture type II.
-
Salter-Harris fracture type III.
-
Salter-Harris fracture type IV.
-
Salter-Harris fracture type V.
-
Anteroposterior (AP) plain radiograph of the knee in a child with persistent knee pain after trauma. The radiographic findings appear normal.
-
Lateral view obtained in the same patient as in the previous image shows only a joint effusion.
-
Sagittal MRI in the same patient as in the previous 2 images.
-
Coronal MRI obtained several weeks after an initial radiograph was obtained to assess ligamentous injury shows an unexpected finding of a Salter-Harris type III fracture.