Practice Essentials
Reflux nephropathy occurs in approximately 1-3% of children and is associated with 7-17% of children developing end-stage renal disease (ESRD) around the world, and it may account for up to 10% of ESRD cases in adults. Reflux nephropathy is a direct result of vesicoureteral reflux (VUR) or another urologic condition that causes chronic high-pressure reflux of sterile urine and often leads to recurrent urinary tract infections. However, not all patients with urinary tract infections and vesicoureteral reflux develop reflux nephropathy. [1, 2, 3, 4, 5]
Renal ultrasonography (RUS) and voiding cystourethrography (VCUG) are the preferred radiologic examination methods for reflux nephropathy. [6, 7, 8] The 2 procedures provide complementary information. RUS helps evaluate the upper urinary tract (kidneys and proximal portion of the collecting system) for anomalies, masses, calcification, hydronephrosis, and size and can identify renal scarring if moderate to severe in degree. VCUG helps evaluate for vesicoureteral reflux (VUR) and the anatomy of the lower urinary tract (bladder and urethra).
Contrast-enhanced voiding urosonography has been found to be a sensitive, radiation-free imaging method for the diagnosis of VUR, [9] though it may overestimate the incidence of reflux. [10]
Nuclear medicine renal scanning with a cortical imaging agent (eg, technetium-99m [99mTc] dimercaptosuccinic acid) is a better means of detecting and identifying renal scarring than is ultrasonography.
Imaging with renal scanning may require sedation in younger children. Sedation is increasingly requested, although rarely necessary, for children undergoing VCUG.
Magnetic resonance imaging (MRI) is not routinely indicated in the evaluation of reflux nephropathy because of the procedure's cost and the potential need for patient sedation. As with CT scanning, MRI can demonstrate renal scarring and hydronephrosis, but not VUR. [11]
Computed tomography (CT) scanning is not indicated in the evaluation of reflux nephropathy because of radiation dose, the need for intravenously administered contrast material, and the potential need for patient sedation. Although CT scans can demonstrate renal scarring and hydronephrosis, they cannot demonstrate VUR.
(See the images below.)
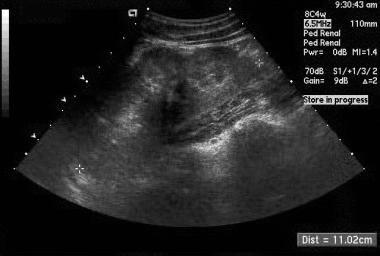 Sonogram in a child with recurrent urinary tract infections and vesicoureteral reflux. Focal contour indentation along the lower lateral margin of the left kidney (longitudinal view) reflects a focal pyelonephritic scar, which is an appearance distinct from the more global parenchymal scarring seen in the next image.
Sonogram in a child with recurrent urinary tract infections and vesicoureteral reflux. Focal contour indentation along the lower lateral margin of the left kidney (longitudinal view) reflects a focal pyelonephritic scar, which is an appearance distinct from the more global parenchymal scarring seen in the next image.
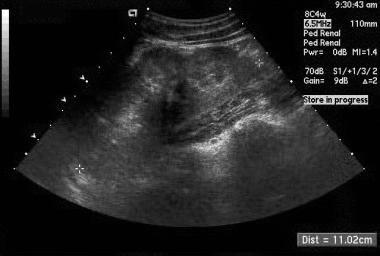
 Longitudinal sonogram of the left kidney in an 18-year-old woman with a history of recurrent urinary tract infections demonstrates normal parenchymal thickness in the upper portion of the kidney and generalized marked parenchymal thinning in the lower portion. The latter reflects chronic pyelonephritic scarring secondary to urinary tract infection and vesicoureteral reflux that occurred in childhood.
Longitudinal sonogram of the left kidney in an 18-year-old woman with a history of recurrent urinary tract infections demonstrates normal parenchymal thickness in the upper portion of the kidney and generalized marked parenchymal thinning in the lower portion. The latter reflects chronic pyelonephritic scarring secondary to urinary tract infection and vesicoureteral reflux that occurred in childhood.
Radiography
Plain images offer no diagnostic information regarding vesicoureteral reflux (VUR) and reflux nephropathy, although they can be used to evaluate spinal anomalies and potential urinary tract calculi, which rarely occur in this population. VCUG is essential in evaluating lower urinary tract anatomy and in identifying or excluding VUR.
With voiding cystourethrography, contrast material is instilled in the urinary bladder via a transurethral catheter and demonstrates increased opacity in the ureters and pelvicaliceal systems when VUR is present. VUR grading (grades 0-5) is based on the distribution and degree of associated upper urinary tract dilatation demonstrated on VCUG.
Intravenous urography (IVU), used to produce the image below, can demonstrate changes reflecting reflux nephropathy and renal scarring, including the following:
-
Dilatation and deformity of one or more renal calyces
-
Loss of parenchymal thickness of a region of the kidney (especially upper and lower poles)
-
Focal contour indentation typically adjacent to a calyx, representing renal scarring
(See the image below.)
 A 15-minute postinjection anteroposterior view of the kidneys in a 9-year-old boy with a history of multiple urinary tract infections who presented with hypertension demonstrates bilateral diffuse calyceal clubbing (arrows) and deformity accompanied by thinning of the adjacent renal parenchyma (arrowheads). These findings reflect chronic pyelonephritis and demonstrate the characteristic appearance of reflux nephropathy on intravenous urography.
A 15-minute postinjection anteroposterior view of the kidneys in a 9-year-old boy with a history of multiple urinary tract infections who presented with hypertension demonstrates bilateral diffuse calyceal clubbing (arrows) and deformity accompanied by thinning of the adjacent renal parenchyma (arrowheads). These findings reflect chronic pyelonephritis and demonstrate the characteristic appearance of reflux nephropathy on intravenous urography.
With VCUG, the degree of confidence is high for detecting VUR and low for detecting chronic pyelonephritic scarring. With IVU, the degree of confidence is moderate for detecting chronic pyelonephritic scarring. [12, 13]
False findings occur infrequently; however, the soft tissue of the bowel wall can simulate contrast enhancement in a ureter, and overlying stool and intestinal gas can sufficiently obscure the kidney to prevent identification of lesser degrees of VUR.
Scarring from reflux nephropathy can usually be differentiated from scarring from other etiologies (such as parenchymal infarction) by the fact the calyx underlying the scar will be deformed in reflux nephropathy.
Ultrasonography
Alteration of renal contour and reduced thickness of the renal parenchyma (seen in the images below) are the primary findings of reflux nephropathy. Ultrasonography is excellent for demonstrating upper urinary tract dilatation. [14, 15, 16, 17]
 Sonogram in a child with recurrent urinary tract infections and vesicoureteral reflux. Focal contour indentation along the lower lateral margin of the left kidney (longitudinal view) reflects a focal pyelonephritic scar, which is an appearance distinct from the more global parenchymal scarring seen in the next image.
Sonogram in a child with recurrent urinary tract infections and vesicoureteral reflux. Focal contour indentation along the lower lateral margin of the left kidney (longitudinal view) reflects a focal pyelonephritic scar, which is an appearance distinct from the more global parenchymal scarring seen in the next image.
 Longitudinal sonogram of the left kidney in an 18-year-old woman with a history of recurrent urinary tract infections demonstrates normal parenchymal thickness in the upper portion of the kidney and generalized marked parenchymal thinning in the lower portion. The latter reflects chronic pyelonephritic scarring secondary to urinary tract infection and vesicoureteral reflux that occurred in childhood.
Longitudinal sonogram of the left kidney in an 18-year-old woman with a history of recurrent urinary tract infections demonstrates normal parenchymal thickness in the upper portion of the kidney and generalized marked parenchymal thinning in the lower portion. The latter reflects chronic pyelonephritic scarring secondary to urinary tract infection and vesicoureteral reflux that occurred in childhood.
Echo-enhanced cystosonography performed by using ultrasonographic contrast media has the major attribute of the exclusion of ionizing radiation.
With ultrasonography, the degree of confidence is moderate in the detection of reflux nephropathy. Lesser degrees of renal scarring may not be evident with ultrasonography.
Echo-enhanced cystosonography, in limited experience, is reported to be as accurate as radiographic VCU in the identification of reflux.
Fetal lobation and other normal variants of renal development may be mistaken for renal scarring on ultrasonograms.
Nuclear Imaging
Technetium-99m dimercaptosuccinic acid and 99mTc glucoheptonate are scintigraphic agents with a high affinity for the renal cortex (as demonstrated in the image below), because they are concentrated by renal tubular cells. [18, 19] As a result, they produce a relatively high level of renal detail. Concern for acute pyelonephritis, the assessment of renal cortical scarring, and the identification of a malpositioned kidney are among the indications for cortical scintigraphy. The use of single-photon emission CT (SPECT) scanning increases the sensitivity of the agents to changes of renal scarring and acute pyelonephritis.
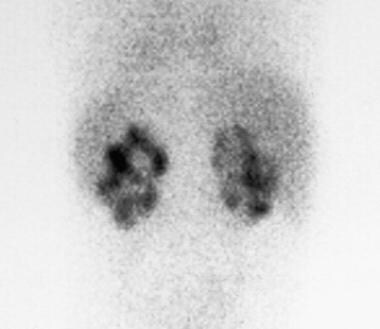 Renal scan by using the cortical imaging agent technetium-99m dimercaptosuccinic acid in a 2-year-old boy with a history of multiple urinary tract infections demonstrates diffuse bilateral renal scarring, which is indicated by the multifocal areas of absence of renal cortical isotope accumulation.
Renal scan by using the cortical imaging agent technetium-99m dimercaptosuccinic acid in a 2-year-old boy with a history of multiple urinary tract infections demonstrates diffuse bilateral renal scarring, which is indicated by the multifocal areas of absence of renal cortical isotope accumulation.
Reduced accumulation of a cortical imaging isotope within the renal margins is an indication of renal scarring. Radionuclide cystogram provides an alternative to VCUG in identifying renal scarring. Cystograms have the primary disadvantage of poor anatomic resolution but the advantage of a lower radiation dose.
The degree of confidence is high with renal cortical imaging performed with 99mTc dimercaptosuccinic acid.
Patient motion, structural abnormalities of the kidneys, and unsatisfactory isotope administration may result in false-positive and false-negative findings.
Patient motion results in inaccurate imaging depiction of isotope distribution and greater probability of underestimating renal scarring (false-negative findings). Hydronephrosis, anomalies such as ectopic and/or fused kidneys, and renal masses or cysts may result in the overestimation of severity of renal scarring (false-positive findings).
-
Sonogram in a child with recurrent urinary tract infections and vesicoureteral reflux. Focal contour indentation along the lower lateral margin of the left kidney (longitudinal view) reflects a focal pyelonephritic scar, which is an appearance distinct from the more global parenchymal scarring seen in the next image.
-
Longitudinal sonogram of the left kidney in an 18-year-old woman with a history of recurrent urinary tract infections demonstrates normal parenchymal thickness in the upper portion of the kidney and generalized marked parenchymal thinning in the lower portion. The latter reflects chronic pyelonephritic scarring secondary to urinary tract infection and vesicoureteral reflux that occurred in childhood.
-
Anteroposterior digital view during voiding cystoureterography of the upper bladder to the kidneys demonstrates bilateral grade 5 vesicoureteral reflux, with severe dilatation of both ureters, the renal pelves, and the bilateral calyces.
-
A 15-minute postinjection anteroposterior view of the kidneys in a 9-year-old boy with a history of multiple urinary tract infections who presented with hypertension demonstrates bilateral diffuse calyceal clubbing (arrows) and deformity accompanied by thinning of the adjacent renal parenchyma (arrowheads). These findings reflect chronic pyelonephritis and demonstrate the characteristic appearance of reflux nephropathy on intravenous urography.
-
Renal scan by using the cortical imaging agent technetium-99m dimercaptosuccinic acid in a 2-year-old boy with a history of multiple urinary tract infections demonstrates diffuse bilateral renal scarring, which is indicated by the multifocal areas of absence of renal cortical isotope accumulation.



